Rare empty sella syndrome found after postoperative hypotension and respiratory failure:A case report
Peng Guo,Zeng-Jun Xu,Chang-En Hu,Yue-Ying Zheng,Dan-Feng Xu
Abstract
Key words: Empty sella; Hypotension; Respiratory failure; Case report
INTRODUCTION
The pituitary gland is a pea-sized gland located within the sella turcica[1,2].Empty sella syndrome is a condition in which the pituitary gland shrinks or flattens,and thus the pituitary cannot be visualised by magnetic resonance imaging (MRI).In this condition,the sella turcica also becomes partially or completely filled with cerebrospinal fluid (CSF).Primary empty sella syndrome occurs when there is a defect in the diaphragma sellae accompanied by an increase in CSF pressure[3].Secondary empty sella syndrome occurs when the pituitary gland has been damaged or injured; common causes include malignancy,trans-sphenoidal surgery,radiotherapy,and medications[4].Patients with empty sella syndrome often suffer from headaches,hypertension,obesity,visual disturbances,CSF rhinorrhoea,or endocrine dysfunction.Postoperatively,our patient presented with hypotension and respiratory failure,and was subsequently diagnosed with empty sella syndrome.
CASE PRESENTATION
Chief complaints
Left shoulder pain and activity restriction for 3 h.
History of present illness
A 60-year-old man was admitted for further workup of left shoulder pain.X-ray demonstrated a left distal clavicle and shoulder blade fracture.He was assessed by the orthopaedics team and booked for internal fixation of the left clavicle.General anaesthesia with a nerve block was administered.Pre-operative vitals included a blood pressure (BP) of 120/63 mmHg,heart rate (HR) of 65 bpm,and SpO2of 95% in room air.After induction,BP and HR decreased to 90/52 mmHg and 50 bpm,respectively.A 6 mg dose of ephedrine was given intravenously.A total of 24 mg ephedrine was given over the whole operation.No further muscle relaxants were required.The surgery was uneventful and lasted for 1 h.Total blood loss was 100 mL and a total of 1000 mL of crystalloid was given.After surgery,he was transferred to the post-anaesthesia care unit to continue machine ventilation.The patient began spontaneously breathing at 40 min postoperatively,at which point the laryngeal mask was removed and an oxygen mask provided.However,SpO2remained below 92%without the use of the oxygen mask.The patient was subsequently admitted to the orthopaedics ward.Vitals at that time were BP 115/76 mmHg,HR 72 bpm,SPO299%,and temperature (T) 37.2°C.
Unfortunately,his BP continued to decrease over the next 6 hours,to 80/50 mmHg.The next morning,the patient appeared confused and was not cognisant to person,place,or time.Arterial blood gas indicated respiratory acidosis without any evidence of electrolyte imbalance.Due to increasing respiratory distress,emergent intubation was performed and the patient was transferred to the intensive care unit for machineassisted ventilation and vasopressor medications.Over the next 2 d,there was minimal improvement in the patient’s condition despite ongoing treatment.
Careful review of the patient’s history,as provided by his family,revealed that over the last year,he began demonstrating signs of progressive indifference,lack of communication,and lethargy.Further physical examination revealed a diffuse loss of body hair and dry skin.This new information,combined with the current episode of hypotension and respiratory distress,strongly suggested a possible aetiology of hormonal dysfunction.As such,endocrine tests were performed,with the results supporting a diagnosis of hypopituitarism with hypocortisolism and hypothyroidism.Then,he underwent brain MRI.
History of past illness
He denied any other medical conditions.
Personal and family history
He worked as a manual labourer.He neither smokes nor drinks.
Physical examination upon admission
The left shoulder joint is tender,the snoring pain is positive,and the activity is limited.
Laboratory examinations
Haemoglobin concentration was 108 g/dL.The results of endocrine tests are listed in Table 1.
Imaging examinations
X-ray of the shoulder demonstrated a left distal clavicle.Brain computed tomography revealed a low density shadow in the saddle region of the brain.Brain MRI (Figure 1)demonstrated that the sella was enlarged and filled with CSF.
FINAL DIAGNOSIS
Empty sella syndrome.
TREATMENT
The patient was started on replacement therapy with once-daily intravenous hydrocortisone 100 mg.After 3 d,levothyroxine was added.
OUTCOME AND FOLLOW-UP
The patient’s consciousness and breathing improved progressively and the endotracheal catheter was removed after 5 d of treatment.He continued oral medication after he was discharged and was followed regularly to the department of endocrinology.
DISCUSSION
The pituitary gland is composed of an anterior and posterior lobe.The anterior lobe secretes hormones that regulate target glands,including the gonads,thyroid,and adrenal cortex.These hormones serve to regulate growth,sex organ function,pregnancy and nursing,metabolism,and BP.When all or most of the pituitary gland is destroyed,hypopituitarism occurs and a series of characteristic symptoms will manifest depending on the specific hormone deficiency.Common causes of hypopituitarism in adults include pituitary tumours or surgery,cerebral trauma,radiation,or Sheehan syndrome caused by postpartum ischemia.Clinical outcomes vary with the type and degree of hormone deficiency,and with the rapidity of onset,age,and sex.Pituitary crisis occurs if the hypopituitarism is further exacerbated by fatigue,hunger,cold,anaesthetic sedation,trauma,surgery,or infection.The diagnosis and management of the condition are based on history,physical examination and,occasionally,laboratory findings.
In a study by Ghatnattiet al[5],hyperprolactinemia was found to be the most common endocrine abnormality.Thwinet al[6]reported a patient who initially developed meningeal irritation with long-term galactorrhoea.Based on elevated serum prolactin and MRI findings,the patient was subsequently diagnosed withempty sella syndrome.Taiebet al[7]described a 47-year-old woman with bilateral galactorrhoea and spaniomenorrhea since the age of 31 years.Investigation revealed an elevated serum prolactin level of 635 mIU/L and an empty sella turcica on MRI.
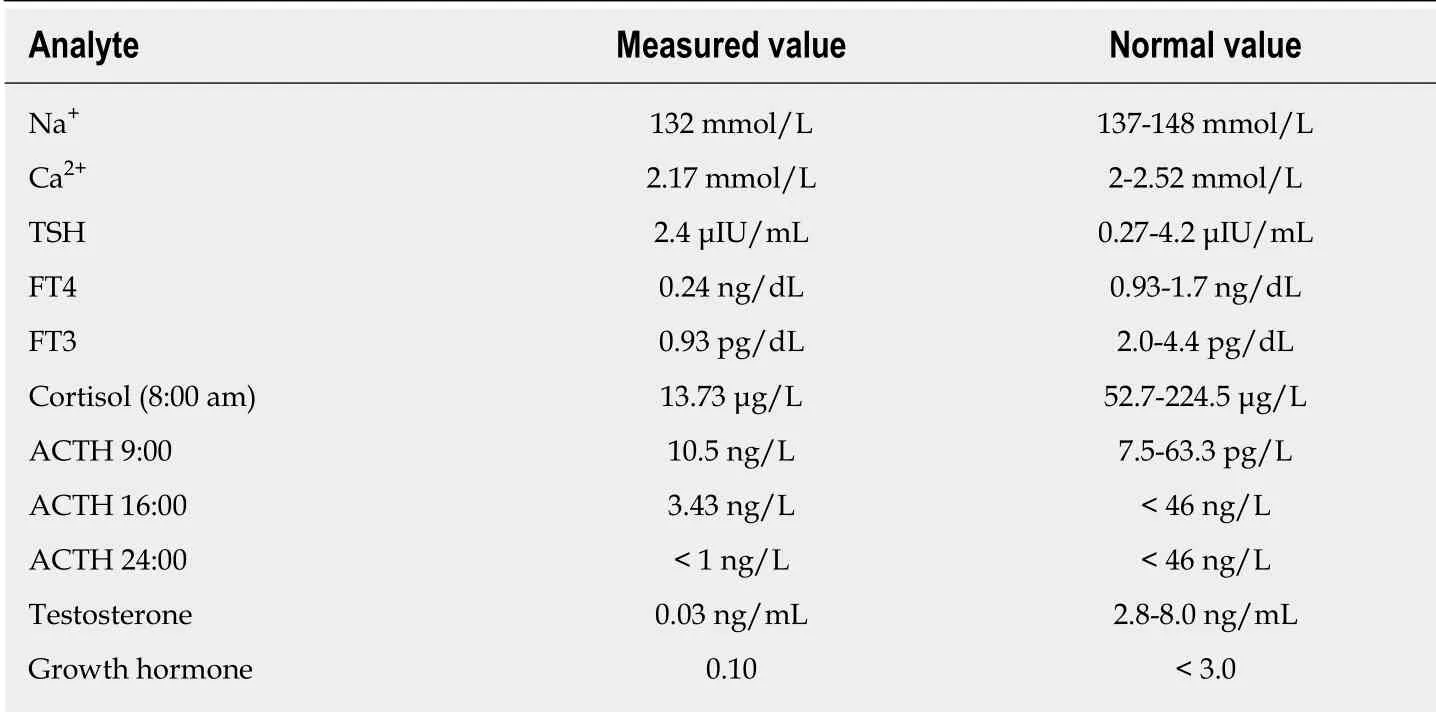
Table 1 Laboratory investigations
Aijaziet al[8]reported a 41-year man with a history of osteogenesis imperfecta,who presented with vomiting,decreased oral intake,and confusion.In treating his hyponatremia,the treatment team was prompted to look for other pituitary hormone deficiencies.Various hormonal defects were found,and the patient was subsequently diagnosed with primary empty sella syndrome.Yanget al[9]described a 69-year-old woman with hyponatremia,who presented with manic symptoms that resolved after plasma sodium was normalised.
Xuet al[10]reported a 41-year-old man with persistent epiphyses and severe osteoporosis.He initially presented with high levels of serum phosphorus and prolactin,and low levels of free triiodothyronine,free thyroxine,and testosterone.Imaging of the brain revealed an empty sella.
Dangeet al[11]reported a 16-year-old girl with a history of stunted growth and primary amenorrhea,presenting with headache and vomiting.Endocrine testing showed reduced levels of growth hormone,luteinising hormone,and follicular stimulating hormone.MRI of the brain showed an empty sella.
The most common cause for postoperative respiratory and hemodynamic failure is the residual effect of anaesthesia[12].Our patient was administered both general and regional anaesthesia.All anaesthetic types had a short duration of action,except the small dose of sufentanyl given at time of induction.Marked dysfunctions in SpO2,BP,and consciousness emerged in the immediate postoperative period.After careful review of the patient’s history and further physical examination,it was felt that the respiratory distress and impaired consciousness could be secondary to hormonal dysfunction.This hypothesis was supported by further endocrine testing and MRI,with a subsequent diagnosis of empty sella syndrome causing the hypopituitarism with typical hypocortisolism and hypothyroidism.Effective treatment was achieved through hormone replacement therapy.
CONCLUSION
We report a case of empty sella syndrome discovered in the workup of postoperative hypotension and respiratory failure.We believe that the patient’s pituitary crisis was induced by surgery.This case highlights the importance of considering pituitary hormone insufficiency in the context of respiratory and hemodynamic failure during the perioperative period.We recommend that in the preoperative examination,a thyroid function test can be added.If there is any abnormality,the examination can be further improved to exclude related diseases.
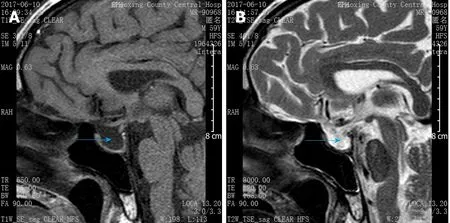
Figure 1 Saggital view of T1 and T2 weighted magnetic resonance images.
 World Journal of Clinical Cases2019年5期
World Journal of Clinical Cases2019年5期
- World Journal of Clinical Cases的其它文章
- Melanotic Xp11-associated tumor of the sigmoid colon:A case report
- Intrauterine cystic adenomyosis:Report of two cases
- Use of tunnel endoscopy for diagnosis of obscure submucosal esophageal adenocarcinoma:A case report and review of the literature with emphasis on causes of esophageal stenosis
- Concomitant paraganglioma and thyroid carcinoma:A case report
- Application of computer-assisted navigation in treating congenital maxillomandibular syngnathia:A case report
- Perioperative topical ascorbic acid for the prevention of phacoemulsification-related corneal endothelial damage:Two case reports and review of literature
