Cataract in diabetes mellitus
Hasan Kiziltoprak,Kemal Tekin,Merve Inanc,Yasin Sakir Goker
Hasan Kiziltoprak,Yasin Sakir Goker,Department of Ophthalmology,University of Health Sciences,Ulucanlar Eye Training and Research Hospital,Ankara 06240,Turkey
Kemal Tekin,Merve Inanc,Ophthalmology Department,Ercis State Hospital,Van 65400,Ercis,Turkey
Abstract
Key words:Diabetes;Cataract;Complications;Surgery
INTRODUCTION
The prevalence of diabetes mellitus (DM) is increasing on a daily basis,with the International Diabetes Federation estimating that there will be 439 million DM patients by 2030[1].An aging population and longer patient life expectancy also means that the prevalence of DM will exceed 33% by 2050[2].DM can lead to pathologies in many tissues in the eye structure,with both a systemic chronic metabolic disease and a microangiopathic character[3].Cataract is one of the major causes of visual impairment in diabetic patients[4].Patients with DM are reported to be up to five times more likely to develop cataract,in particular at an early age[5-8].Due to the increasing prevalence of DM,the incidence of diabetic cataracts has also risen.Cataract extraction is one of the most common surgical procedures among the general population,and the number of cataract surgeries each year also continues to increase.Recent technological advancements in cataract surgery have improved surgical outcomes.However,in diabetic individuals,the scale of improvement is still a matter of debate,and many studies have revealed both the results and complications of cataract surgery in diabetic patients.In the light of these findings,this study will review related articles in order to highlight current developments and controversies regarding cataract surgery management in patients with DM.
BIOCHEMICAL MECHANISMS FOR CATARACT IN DIABETES
Different types of mechanisms have been proposed for the pathogenesis of cataract in cases of DM.
Polyol pathway
It has been suggested that the polyol pathway-viawhich the enzyme aldose reductase(AR) catalyzes the reduction of glucose into sorbitol-is a central part of the mechanism of cataract development[9-11].Multiple studies have been conducted to explain the AR pathway’s role in this process.The increased intracellular accumulation of sorbitol leads to a hyperosmotic effect,resulting in hydropic lens fibers that degenerate and form cataract[9,12].The production of sorbitol in diabetic patients (as compared to nondiabetic patients) takes place more quickly than it can be converted into fructose by the enzyme sorbitol dehydrogenase.Intracellular removal of sorbitol through diffusion is also prevented because of its polar character.A hyperosmotic effect is created when an accumulation of sorbitol results in an infusion of fluid.Finally,animal studies have shown that the intracellular accumulation of polyols causes liquefaction of lens fibers resulting in the formation of lens opacities[9,10,12,13].In the study of Oishiet al[13],it was found that AR levels in red blood cells of patients under the age of 60 and with short duration of DM had a positive correlation with the prevalence of posterior subcapsular cataract.Moreover,a negative correlation was reported between the level of AR in erythrocytes and the density of lens epithelial cells,which is known to be lower in diabetics than in nondiabetics.These findings suggest that AR may play a role in this pathomechanism.
Osmotic and oxidative stress
Some studies have shown that osmotic stress in the lens resulting from sorbitol accumulation causes apoptosis in lens epithelial cells and leads to cataract formation[25].Rapid glycemic control can also increase these effects in the lens by creating a hypoxic environment that reduces protective enzymes and increases oxidative radicals.High AR expression could constitute a risk factor that predisposes the lens to distortions in signaling through the extracellular signal-regulated kinase and c-Jun N-terminal kinase pathways-involved in cell growth and apoptosis,respectively-thereby altering the balance required for lens homoeostasis[11,26].These findings show that impairments in osmoregulation may render the lens susceptible to even the smallest increase in AR-mediated osmotic stress,potentially leading to progressive cataract formation.
Autoimmunity
Another recently proposed mechanism is autoimmune hypothesis in acute bilateral type 1 diabetic cataracts[26].The authors reported that insulin autoantibodies became positive within three months of beginning insulin treatment,and that this period coincided with cataract formation.Their suggestion that there could be an autoimmune process behind acute bilateral cataract in DM warrants further investigation[26].
The type of cataract seen in diabetic patients has also been investigated.The most common is the senile type[10].However,snowflake cataracts,which are characteristic for DM,are very common in type 1 diabetics.Posterior subcapsular cataracts have also been shown to be significantly associated with diabetes.Increased levels of glycated hemoglobin were demonstrably associated with an increased risk of nuclear and cortical cataracts[6].Further analysis revealed that diabetic patients were prone to developing cortical cataracts and that this process was associated with the duration of diabetes[5,7].
Finally,the initiating mechanism in diabetic cataract formation is the generation of polyols from glucose by AR.However,osmotic stress,apoptosis of the lens epithelial cells,and the autoimmune theories may be confounding mechanisms in the development of the cataract formation in DM.
CATARACT INCIDENCE IN DIABETIC PATIENTS
Several clinical studies have reported that cataract formation occurs more frequently and at an earlier age in diabetic patients than in nondiabetic patients[7,27-29].Some studies indicate that cataracts are three to four times more prevalent in patients with diabetes under the age of 65.In patients over 65,cataracts are twice as prevalent[27,30].The main risk factors are longer duration of diabetes and poor metabolic control.Although older patients suffer from irreversible cataract formation,good metabolic control may reverse cataract in young diabetics.
Several important study groups have investigated cataract incidence in diabetic patients.The Wisconsin Epidemiologic Study of Diabetic Retinopathy investigated the incidence of cataract and factors associated with a higher risk of cataract surgery[7].They found 8.3% of patients suffering from type 1 diabetes and 24.9% of those with type 2 diabetes had a 10-year cumulative incidence of cataract surgery.For type 1 diabetics,they found some risk factors,including age,severity of diabetic retinopathy(DR),and proteinuria;for Type 2 diabetics,risk factors included age and use of insulin[7].
The Beaver Dam Eye Study also reported an association between DM and cataract formation[5].The study took place over five years and consisted of 3684 participants aged 43 and older.It showed an increased incidence and progression of cortical and posterior subcapsular cataracts for DM patients.It also found an increased risk of nuclear and cortical cataracts with increased levels of glycated hemoglobin.Further analysis of the study showed that diabetics had a higher rate of cortical lens opacities and previous cataract surgery than nondiabetics[6].A longer duration of diabetes was also associated with increased frequency of both cortical cataracts and cataract surgery.
从《内蒙古地区旅游业收入情况表》中可以看出:自2010年~2017年,内蒙古地区旅游业发展总体趋势向好。全年旅游业总收入呈逐年递增趋势,在第三产业增加值中所占比重由2010年的17.5%上升至2017年的42.7%,翻一倍的贡献。
The Blue Mountains Eye Study aimed to examine the relationship between nuclear,cortical,and posterior subcapsular cataracts[31].The study supported the findings of previous research,but also found an association between posterior subcapsular cataracts and DM.In contrast to the Beaver Dam Eye Study,nuclear cataracts showed a weak association with DM.
The Barbados Eye Study evaluated the relationship between diabetes and lens opacities among 4314 black participants[32].The authors found that a history of DM(18% prevalence) was related to all lens changes,especially at younger ages.Another study by Srinivasanet al[33]found,for diabetics,the cumulative incidence of cataracts is much higher than that of progression.Moreover,they indicated that the main risk factor for cumulative incidence and progression of most types of cataract is age,with higher rates of both in older patients.
TIMING OF SURGERY
Approaches to the timing of cataract surgery in diabetic patients seem to be changing worldwide.Where once a more conservative approach was applied,now there is a growing tendency toward early surgery.Pollacket al[34]reported that the main cause of poor visual outcomes is macular edema (ME).For this reason,they do not recommend cataract extraction for eyes with DR until visual acuity has deteriorated to 20/100-20/200.Similarly,Schatzet al[35]stated that diabetic patients with cataracts might wish to postpone surgery,especially if there is any retinopathy present preoperatively.
The growing tendency toward earlier cataract surgery in patients with diabetes has contributed to improved visual outcomes[36].This approach facilitates panretinal photocoagulation (PRP) and also allows for the identification and adequate treatment of diabetic macular edema (DME) before cataract surgery.In addition,if surgery is undertaken before lens opacities make it more difficult to detect retinal thickening using macular assessment,then risk of ME decreases and visual outcomes may be considerably improved[37].
PREOPERATIVE EVALUATION
Preoperative counseling is crucial for diabetic patients.Before surgery,patients should have good glycemic control and no evidence of ocular or periocular infection.Transient refractive changes related to morphologic and functional changes in the crystalline lens should be observed during periods of unstable blood sugar[38].Hyperglycemia induces myopia and,when intensive medical therapy is applied,patients tend to become more hyperopic as opposed to hyperglycemia.Changes in corneal topographic parameters during periods of glycemic changes can be a potential source of error in keratorefractive and biometric calculations[39].
A thorough and comprehensive ophthalmologic examination-including an assessment of bestcorrected visual acuity (BCVA) and relative afferent pupillary defect;using slitlamp biomicroscopy to assess the corneal health and neovascularization of the iris (NVI);and using tonometry,dilated fundoscopy,and gonioscopy for the evaluation of neovascularization at the angle-is mandatory.In select cases,advanced diagnostic evaluations such as fluorescein angiography,optical coherence tomography (OCT),and Bscan ultrasonography may be helpful.Due to the range of diabetic anterior segment changes,an experienced surgeon will perform better[40].
Consultation with vitreoretinal subspecialists is recommended by some authors,especially in complicated cases[41].PRP is recommended preoperatively in patients with pre-existing proliferative diabetic retinopathy (PDR),because of its possible rapid progression after cataract surgery.In situations where lens opacity precludes PRP,it can be performed after surgery.Another approach is preoperative panretinal cryopexy or combined cataract surgery with vitrectomy and endolaser photocoagulation,particularly in cases with posterior pole tractional retinal detachment(TRD).ME should be efficiently treated preoperatively,since pre-existing maculopathy may worsen postoperatively and is strongly associated with a poor visual outcome[42].
Treatment options for ME are laser photocoagulation,pharmacotherapy with intravitreal injections of antivascular endothelial growth factor (anti-VEGF) agents,or steroids[43,44].Because preexisting DME can increase the risk of ME progression by 20%-50%,intravitreal antiVEGF agents are recommended perioperatively[45,46].Steroids,on the other hand,have been shown to be effective for persistent or refractory DME[47].Dexamethasone implants and fluocinolone implants resulted in significant improvement in clinically significant ME and visual outcomes[48,49].It has also been shown that dexametason has a potentially lower risk of intraocular pressure elevation and cataract formation compared to fluocinolone acetonide and triamcinolone acetate[50].Recently,preoperative use of nonsteroidal antiinflammatory drugs,such as diclofenac and nepafenac,has been examined.Most studies suggested that they did not reduce the chances of postoperative ME in patients with DR[51-54].
Patients with NVI also need prompt treatment,including PRP.In patients who develop neovascular glaucoma (NVG),medical therapy is the first line of defense,however,it is usually ineffective.Eyes with active NVI are at greater risk for intraoperative and postoperative complications.Anti-VEGF agents such as bevacizumab showed dramatic short-term responses in terms of intraocular pressure reduction and regression of neovascularization in the treatment of NVG[55,56].Cataract surgery after administering anti-VEGF agents should be done with or without vitrectomy as early as possible to enable treatment of the posterior segment.When NVG is a problem,a combination of trabeculectomy with phacoemulsification may also be considered after regression of NVI.Despite all these options,the visual outcomes following phacoemulsification in eyes with NVG are generally poor.
CATARACT SURGERY IN DIABETIC PATIENTS
Cataract surgery in diabetic patients yields better results since the introduction of phacoemulsification,when compared to extracapsular or intracapsular cataract surgery[57,58].Different options are available during surgery that can lead to better surgical results and improved postoperative retinopathy evaluation.As anterior capsular phimosis is more common in diabetic eyes,capsulorhexis size should be larger than normal but smaller than the intraocular lense (IOL) optic diameter,in order to prevent anterior IOL displacement and posterior capsular opacification(PCO)[59-61].However,a large diameter optic is also important for the postoperative diagnosis and treatment of peripheral retinal pathology[8].
Progression of retinopathy after cataract surgery is another problem in diabetic patients[62].The duration and complexity of cataract surgery are the main risk factors for progression of retinopathy[63];it is therefore important to reduce the time and complexity of the surgery.Poor pupillary dilatation can be seen in diabetic patients as the result of damage to pupillary parasympathetic supply and elevated prostoglandin levels[64,65].This means that pupil dilation is also a problem for these patients.As such,iris hooks,malyugin rings,or other iris expanders should be considered for intraoperative use.In cases with NVI,bleeding in the anterior chamber during or after surgery should also be kept in mind.Photic retinopathy during cataract surgery,especially surgeries of a longer duration,was also more prevalent in diabetic patients than nondiabetics[66].
While the presence of DM does not increase complications such as posterior capsular rupture,zonular dehiscence,or vitreous loss,the effect of DM on the entire eye can result in other problems.The effects of DM on the ocular surface include neurogenic effects (subbasal nerve abnormalities) and impaired corneal stem cell and epithelial cell division,which can result in keratoepitelyopathy and lead to corneal epithelial defects/abrasions,which may heal slowly[40,67].It has also been shown that corneal endothelial cell loss is higher in people with diabetes than in nondiabetics[68-70];this means that routine evaluation of diabetic patients using specular microscopy is recommended.Moreover,surgeons should take greater care in order to reduce endothelial stress during surgery.
INTRAOCULAR LENS CHOICE
The most common problem for diabetic patients is DR.For this reason,optimal visualization and treatment of the retina should be kept in mind during cataract surgery.As the diameter of the lens increases,it will provide a larger optical area-a difference that may be crucial for optimal management of DR.
PCO is another concern following cataract extraction.It has been reported that the development and severity of PCO is increased in DM patients as compared to nondiabetic patients[60,71].Several studies have shown a relationship between the development of PCO and lens material type,and that the shape of the lens[72].A square edge design seems to inhibit lens epithelial cell proliferation and may therefore prevent PCO formation[72].
Several studies have evaluated the biocompatibility of three common materials used to manufacture foldable IOLs with diabetic patients.One performed a comparison between hydrophobic acrylic and plate-haptic silicone IOLs in diabetic patients;although PCO developed less frequently with hydrophobic acrylic IOLs,it was demonstrated that this material was associated with a higher risk of anterior chamber flare in the early postoperative period[72].In addition,hydrophobic acrylic lenses have the lowest propensity for silicone oil adhesion,meaning that they may be the IOL of choice for diabetic patients.Because diabetic patients may need vitreoretinal surgery during the course of managing their disease,silicone IOLs that develop condensation during pars plana vitrectomy may be relatively contraindicated in such individuals[73].Hydrophilic acrylic IOLs are prone to opacification,particularly in patients with PDR,since elevated levels of phosphorus in the serum combined with the aqueous humor of diabetic patients may lead to opacification.Several reports have proved progressive calcific opacification of hydrophilic acrylic IOLs in diabetic patients[74-77].Rodríguez-Galieteroet al[78]evaluated contrast sensitivity and color discrimination in diabetic patients and suggested that blue-light filtering IOLs do not cause chromatic discrimination defects,but that they may even improve color vision in the blue-yellow chromatic axis.Multifocal and accommodative IOLs in people with diabetes are controversial.Postoperative laser treatment and fundus visualization during vitrectomy are difficult because of the optics of these types of lenses[79].Additionally,the design of multifocal IOLs reduces contrast sensitivity and could be a cause of visual dissatisfaction for patients with preexisting maculopathy[79].
The implantation site in diabetic patients is also important.For DM patients,the ideal site is the capsular bag,as usual.The use of anterior chamber angle-fixated lenses and sulcus fixated posterior chamber IOLs in diabetic patients is controversial.It is recommended that iris claw lenses be avoided in patients with DM,due to the increased risk of iris neovascularization.The theoretical risk of cystoid ME,ovalization of the pupil,and poor mydriasis are other risk factors for diabetic patients after iris claw IOL implantation.
POSTOPERATIVE MANAGEMENT AND INDICATORS OF POOR VISUAL OUTCOMES
Carefully performed cataract surgery in diabetic patients should yield optimal postoperative results.Patient follow-up should also be done carefully.Preoperatively,patients diagnosed with NPDR who have adequate retinal view should undergo detailed retinal examination within three months of cataract extraction.Patients with PDR or those with inadequate retinal view prior to cataract extraction should be examined closely after surgery in order to evaluate their DR status[80].
Endophthalmitis is the most serious complication of cataract surgery.The risk of postoperative endophthalmitis in diabetic patients has increased and is associated with a poor visual prognosis.
As previously mentioned,as a patient’s age and duration of diabetes increases,there is greater prevalence of corneal epithelial defects and persistent erosions due to impaired corneal innervation[40,68].Corneal endothelial cell damage and persistent corneal edema in diabetic patients following cataract surgery have also increased[81,82].Specular microscopy should therefore be used to evaluate DM patients and all the necessary precautions should be taken intraoperatively.Also more frequently observed in diabetic patients are severe iritis,posterior synechiae,pupillary block,and pigmented precipitates on the IOL[83].
The Early Treatment Diabetic Retinopathy Study (ETDRS) outlines the prognostic factors after cataract surgery.The presence of clinically significant macular edema(CSME) at the time of surgery was found to be a predictor of poor final BCVA in cases of uncomplicated phacoemulsification[84].Another determinant of poor postoperative BCVA was the severity of DR at the time of surgery.As the severity of retinopathy increased,the risk of macular ischemia or edema also increased[36,58,85].More severe retinopathy also correlated with a reduced tendency for spontaneous resolution of postoperative ME,which is itself associated with poor postoperative BCVA.PDR without any treatment prior to cataract surgery is another factor-one which comes with an increased risk of vitreous hemorrhage and TRD following surgery[86].
COMPLICATIONS
Despite the advancement in phacoemulsification technology,poor visual acuity following cataract extraction is still common in patients with DM.PCO,postoperative cystoid macular edema (CME),DME,and worsening of the DR are the main complications seen in diabetic patients[87].
PCO formation
PCO is one of the most common causes of decreased vision after cataract extraction.Although modifications in surgical technique and improvements in IOL technology have reduced the incidence of PCO,it is still a problem for these patients.Proliferation of lens epithelial cells and the degree of postoperative inflammation are associated with development of PCO.Proliferation of lens epithelial cells is affected by several factors,including optic edge design,optic-haptic junction,and IOL material.However,surgical trauma and contact with the IOL can induce inflammation and cause epithelial cells to produce cytokines,which induce collagen production and fibrous metaplasia[88].
While some studies revealed a higher incidence of PCO in diabetic patients[60,89],others showed fewer cases of PCO in diabetic eyes,regardless of the retinopathy stage,over the course of two years[90].In a study by Hyashiet al[91],the development of PCO was significantly higher in diabetic patients 18 mo after surgery,even though it was similar to the control group for the first 12 mo.Severity of retinopathy did not have an impact on the development of PCO,according to some studies[92].Figure1 demonstrates PCO development in a diabetic patient six months after cataract surgery.
Macular edema
The development of DME,pseudophakic macular edema (PCME),CME,or Irvine-Gass syndrome are other frequent causes of postoperative vision deterioration among the general population[93,94].Altered concentrations of angiogenic factors after cataract surgery may aggravate maculopathy[95].OCT imaging has also revealed increased retinal thickness following an uneventful cataract surgery in diabetic eyes without retinopathy as compared to non-diabetic eyes[96].Chuet al[93]reviewed 81,984 eyes and reported that,even in the absence of retinopathy,diabetic patients’ eyes had an increased relative risk of ME after surgery.In addition,patients with preexisting DR had a higher relative risk of ME,with this risk being proportional to the increasing severity of retinopathy[93].Figure2 shows the development of CME in a diabetic patient after cataract surgery.
The incidence of CME varied between 0.2% and 20% in older studies.However,recent studies report lower rates of CME,ranging from less than 1% to 2%-3%[97].The methods of detection used in these studies have a significant effect on the rate of CME detection.Fluorescein angiography and OCT were more sensitive,for example,reporting higher rates of CME than clinical detection[97].It is also important to differentiate DME from PCME (Irvine-Gass syndrome),since the pathogenesis,treatment,natural course,and outcomes for both are very different.While the underlying presence of DR,exudates,and ME point toward DME,if there is minimal or no DR and there are no exudates in the posterior pole,this suggests PCME.When in doubt,fluorescein angiography can help to distinguish;if the angiography shows a petaloid pattern associated with hyperfluorescence of optic disc and there is no retinopathy or microaneurysms,edema may be considered as a result of Irvine-Gass syndrome[36].
According to Medicare data,the cost of cataract surgery and related patient care in the United States can be doubled due to ME[98,99].Therefore,the prevention of CME in diabetic patients is very important.Recently,both prophylactic and therapeutic usage of both topical steroidal and non-steroidal anti-inflammatory eye drops (NSAIDs) has become central to perioperative management of CME in diabetic patients.Especially NSAIDs have been shown to decrease the incidence of CME in the general population.In a systematic review of 15 randomized trials,Kesselet al[100]showed that topical NSAIDs are more efficient in preventing CME than topical steroids.However,the use of NSAIDs did not change the incidence of CME in patients with DR[101].
In addition to facing a higher risk of CME,diabetic patients with preexisting DME are at an increased risk of worsening edema following cataract surgery[29,36].In ETDRS Report 25,the presence of preexisting,CSME-though it showed no statistically significant difference in the prevalence of ME before and one year after surgery-was associated with worse visual outcomes[36].Although ME is commonly seen after cataract surgery,it can follow a benign course.The development of postoperative CSME may be the result of the natural progression of the disease rather than a direct effect of surgery on many patients.On the other hand,the clinical course was quite different in eyes with CSME at the time of surgery.None of them resolved spontaneously within a year and the majority showed clinical and angiographic signs of deterioration.Dowleret al[37]have shown that CSME at the time of cataract surgery is associated with worse visual acuity outcomes at one year post-surgery.It seems possible that severe ME after cataract surgery represents a postoperative deterioration of pre-existing ME that was previously untreated because of lens opacity[36].
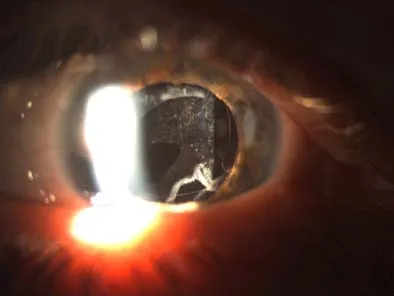
Figure1 Anterior segment photograph of a diabetic patient who developed posterior capsular opacification six months after phacoemulsification surgery.
Attempts to stabilize and resolve DME will help improve outcomes,if DME is present prior to cataract surgery.Many strategies for the preoperative medical management of DME are available.Postoperative laser photocoagulation for diabetic ME is controversial.The ETDRS established the utility of focal/grid laser photocoagulation for the treatment of ME[102].Focal/grid laser treatment (as described in the ETDRS) was considered as first line treatment for CSME,prior to the use of anti-VEGF agents for central involved DME.It remains an alternative treatment in cases in which anti-VEGFs are not applicable or the center of the macula is not involved[103].On the other hand,Pollacket al[34]and Dowleret al[37]showed that ME resolves spontaneously if it arises postoperatively but not when it is present preoperatively.They suggested that early laser treatment is unnecessary for all cases of postoperative DME.Generally,experts do not perform argon laser treatment until six months after cataract surgery.
The advent of anti-VEGF injections has shifted the paradigm in the treatment of DME.Many studies performed on anti-VEGF agents in diabetic patients have shown their effectiveness at preventing and treating CSME[104-111].Current opinion supports that anti-VEGF agents are first-line therapy in preoperative treatments,perioperative stabilization of DME,and postoperative management and that they show great success in anatomic recovery and visual function.Focal laser treatment and steroid injections still provide significant additional support.
Progression of retinopathy
Numerous studies have evaluated the effect of cataract surgery on the progression of DR.The progression of DR after intracapsular (ICCE) and extracapsular (ECCE)cataract extraction has been extensively studied[80,112,113].Sebestyenet al[112]and Alparet al[113]demonstrated the progression of retinopathy after ICCE and ECCE,with ICCE showing worse results than ECCE.However,the effect of phacoemulsification is controversial.Modern phacoemulsification procedures are considered faster,safer,and more cost-effective than ICCE and ECCE[114].Even with the advances in modern phacoemulsification techniques,some studies have demonstrated a similar trend of DR progression after phacoemulsification surgery;others have reported no significant change[37,42,115].Figure3 shows the progression of DR in a diabetic patient’s right eye after phacoemulsification surgery.
Prospective studies by Dowleret al[37]and Squirrellet al[42]have reported that uncomplicated cataract extraction using phacoemulsification have no effect on the progression of DR.However,Squirrellet al[42]have shown an increased risk of DR progression following cataract surgery in patients with elevated hemoglobin A1c.These studies included one eye that underwent phacoemulsification surgery and one eye as a control.Conversely,some studies that included diabetic patients undergoing phacoemulsification cataract surgery showed a retinopathy progression rate that had nearly doubled at the 12-mo period as compared to unoperated eyes[84].Similarly,ETDRS Report 25,which enrolled 3711 patients with a nine-year follow-up period,also showed increased rates of retinopathy progression in cases of phacoemulsification than in unoperated eyes[36].A recent study by Dennistonet al[116]reported significant postoperative progression of center involving DME,which was associated with the preoperative grade of DR.Shahet al[41]found that recent studies do not support the generalized conclusion that phacoemulsification causes progression of retinopathy and ME in all diabetic patients.
The risk factors for DR progression have also been investigated.In a retrospective study by Krepleret al[115],these included being male,the disease duration,and poor glycemic control.Dowleret al[37]reported that a smaller incision size and shorter surgical duration for phacoemulsification decreased inflammation and may induce less breakdown of the blood-ocular barrier,meaning that uncomplicated phacoemulsification cataract surgery does not accelerate DR progression.Additionally,recent studies suggest that anti-VEGF injections may also affect the incidence of DR Figure2 progression[117].Despite no current consensus on the prophylactic use of anti-VEGF,their use for patients with more advanced NPDR or PDR and DME should be considered.Other ocular co-morbidities such as vitreous hemorrhage,epiretinal membranes,or TRD may benefit from a combined pars plana vitrectomy and cataract surgery[118].
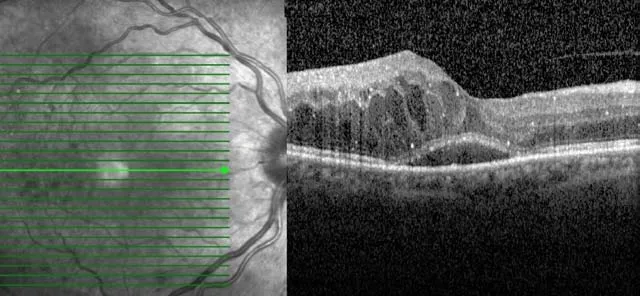
Figure2 Horizontal optical coherence tomography scan of a diabetic patient,showing the development of cystoid macular edema and serous macular detachment after cataract surgery.
CONCLUSION
As the number of people with DM is estimated to continue to increase,cataract surgery will remain important for diabetic patients.Patients with diabetes have multiple issues to be evaluated preoperatively,perioperatively,and in the postoperative period.With the advent of modern surgical and pharmacologic therapies,these patients can,like other cataract patients without diabetes,recover excellent vision.Postoperative monitoring and management of surgical complications will also help to alleviate the risk of vision loss in these patients.
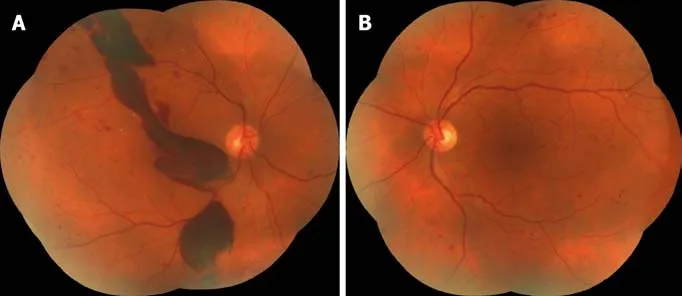
Figure3 Colored fundus photographs of a diabetic patient reveal the progression of diabetic retinopathy in the right eye after surgery.A,B:Both eyes have dot-blot hemorrhages and hard exudates;two months after surgery,massive preretinal hemorrhages occurred in the right eye (A).A:Right eye;B:Left eye.
 World Journal of Diabetes2019年3期
World Journal of Diabetes2019年3期
- World Journal of Diabetes的其它文章
- Crosstalk between gut microbiota and antidiabetic drug action
- Antidiabetic treatment on memory and spatial learning:From the pancreas to the neuron
- Screening the RFX6-DNA binding domain for potential genetic variants in patients with type 2 diabetes
- Targeted genotyping for the prediction of celiac disease autoimmunity development in patients with type 1 diabetes and their family members
- Burden of diabetic foot ulcer in Nigeria:Current evidence from the multicenter evaluation of diabetic foot ulcer in Nigeria
- Optimized health care for subjects with type 1 diabetes in a resource constraint society:A three-year followup study from Pakistan
