Porphyromonas gingivalis and digestive system cancers
Ying Zhou,Guang-Hua Luo
Abstract
Key words:Porphyromonas gingivalis;Oral squamous cell carcinoma;Oesophageal squamous cell carcinoma;Pancreatic cancer;Periodontal diseases
INTRODUCTION
Porphyromonas gingivalis(P.gingivalis),one of several hundred bacterial species in the oral cavity,is an anaerobic gram-negative bacterium[1]and is highly associated with periodontal diseases[2].Dental plaque is a biofilm on the surface of teeth[3]and functions as a highly organized and integrated microbial community in the mouth[4].P.gingivalisis part of the composition of dental plaque and endows dental plaque with a panoply of critical virulence attributes[5].This bacterium regulates the immune reaction of host to promote the proliferation of microbial biofilm,thereby destroying the homeostasis of the host and causing biological disorders and disease[6].P.gingivaliscan be found in the gingival epithelium[7].To effectively colonize,P.gingivalissecretes protein adhesins,heminbinding proteins and proteinases.Such factors could cause toxicity as well[8-10].Arg-specific gingipains (RgpA and RgpB) and Lys-specific gingipain (Kgp) are cysteine proteinases,which are extracellular proteases with multiple effects on both the innate and adaptive immune responses[11,12].These cysteine proteinases are capable of degrading extensive connective tissues and large host defence molecules[13,14].The R-gingipains (Rgp) and Kgp are demonstrated highly related to the relief of inflammation and host defence evasion by means of activating kinin cascade and liquid phase transformation of complement C3 and C5 proteins[15,16].Apart from these defences,some other factors,such as fimbriae,haemagglutinins,lipopolysaccharide,capsule polysaccharides,and major outer membrane protein,have also been demonstrated for potential virulence[17,18].Recently,an increasing number of investigations have focused on cancers related toP.gingivalis.With the deepening of the research concerning this bacterium,outer membrane protein has been reported to make contributions to the interaction and colonization of host,the evasion of immune defense,as well as the destruction of periodontal tissues[19],which may explain howP.gingivalispushes impacts on several digestive cancers.However,more and complicated internal mechanisms still need to be uncovered.This article aims to review the current relationship betweenP.gingivalisand cancer.
P.GINGIVALIS AND ORAL CANCER
Oral cavity consists of diverse boundary surfaces,such as the gingiva,the back of the tongue,tongue side,oral mucosa and so on which contribute to the colonization and growth of various microorganisms.In 2016,accompanying an approximate 48330 new diagnoses and 9570 deaths,oral cancer was considered the sixth most common carcinoma globally[20].Among these,what most commonly happened in oral cavity is oral squamous cell carcinoma (OSCC)[21].P.gingivalishas been discovered colonizing in periodontium and spreading in the original lesion locations of OSCC as well,such as oral and lingual mucosa[22].It is well known that tobacco and alcohol are the major risk factors for oral cancer,and approximately three-fourths of all oral and pharyngeal cancers are owing to tobacco smoking and alcohol drinking in the United States[23].Upon alcohol drinking,P.gingivaliswould dehydrogenate ethanol to acetaldehyde,which is a carcinogenic derivative and capable of contributing to DNA damage,mutation and excessive proliferation of the epithelium[24,25].
The concentration rate ofP.gingivaliswas discovered to be higher among cancer cells than normal tissues of the mouth by Katzet al[26]in 2011.Meanwhile,these authors suggested thatP.gingivalismay lead to mouth cancer and the induction of epithelial cell transformation into a tumour.In a meta-analysis,the prevalence ofP.gingivaliswas 40.7%,andP.gingivalismade the chances of cancer and periodontal disease increasing 1.36 times[27].Kanget al[28]’s study also showed that the incidence ofP.gingivalisin patients with head and neck cancer and in healthy subjects is significantly different.Besides,compared to non-infected withP.gingivaliscontrols,those with long-term infection showed the up-regulating expressions of CD44 and CD133 which are the well-known cancer stem cell markers,and promoted the tumorigenic properties[29].By activating ERK1/2-Ets1,p38/HSP27,and PAR2/NF-kB pathways,P.gingivalisincreases pro-matrix metalloproteinase-9 (proMMP-9) levels and consequently promotes cellular invasion of OSCC cell lines when the proenzyme is stimulated by gingipains[30].Comparing to uninfected cells,those infected withP.gingivaliscells were monitored to increase MMP-1,-2,-9 and -10 levels in time dependence[31].In addition,activated MMP-9 has been illustrated to enhance the invasion of tumour cells;this study was performed with the help of a specific anti-MMP-9 blocking monoclonal antibody[32].As Haet al[33]’s findings also suggested,P.gingivalisinfection makes significant functions in promoting the invasion of OSCC cells,including SCC-25,OSC-20 and SAS cells,through upregulating levels of IL-8 and MMPs (particularly MMP-1 and MMP-2).By establishing a long-term model in which human immortalized oral epithelial cells were chronically challenged withP.gingivalisfor up to 23 wk,Genget al[34]found that long-term exposure toP.gingivalisaccelerated the cell cycle and promoted cell migration as well as invasion abilities,both of which eventually induced metastatic proliferation in distant organs.Compared with non-infectedP.gingivalisin mice,it was demonstrated that chronic infection would make the promotion of metastasisviathe blood pathwayin vivo[21].
P.GINGIVALIS AND OESOPHAGEAL CANCER
On a global scale,oesophageal cancer,the eighth incidence of tumour also contributes to the sixth highest mortality.Asia,especially Central China,is a high-incidence area,whereas data recently revealed that newly-diagnosed cases are rising in Western Europe and America[35].Oesophageal cancer is characteristic of difficulty in early diagnosis,rapid development and high mortality.Tobacco smoking and excess alcohol consumption are risk factors for oesophageal cancer[36].This cancer has two major histological subtypes,squamous cell carcinoma and adenocarcinoma;the former is common in developing countries and the latter is more common in developed nations[37].In this review,oesophageal squamous cell carcinoma (ESCC) is the focus.The similarity in histology between oesophageal squamous cells and oral squamous cells is well-known,and it has been revealed that there is a high frequency ofP.gingivalis(61%) in ESCC[36].In this study,the expression intensity ofP.gingivalisantigen and the exclusive Lys-gingipain protease,as well as the detection of theP.gingivalis-specific 16S rDNA in ESCC patients,all of them were notably higher in tumour tissue than in ambient tissue or normal controls.In addition,the differentiation of tumour cells,the distant metastasis of ESCC,the survival ratio of ESCC patients and other clinicopathological factors all positively relate to the existence ofP.gingivalis.Such conclusions not only firstly proved that infection withP.gingivaliswould act as a new risk factor of ESCC,but also indicated thatP.gingivaliscould serve as a prognostic biomarker for ESCC[36].The inhibition of epithelial cell apoptosis,the promotion of tumour cell immune invasion and the metabolism of potentially carcinogenic substances induced byP.gingivalisall contribute to the occurrence and development of ESCC[12,24,25,32,38,39].Gaoet al[40]firstly reported the implication between host immunologic reaction to P.gingivalis and malignant proliferation of ESCC cells.They also suggested that IgG and IgA for P.gingivalis played a role as possible serum markers of ESCC,and combining the both would advance the diagnosis and improve prognosis[40].Finally,interestingly,the rate of infection of P.gingivalis is much higher in oesophageal cancers than in cardiac cancers and is approximately as low as zero in gastric cancer,which is due to lack of acid adaptation[41].
P.GINGIVALIS AND PANCREATIC CANCER
Pancreatic cancer,which has a low frequency,is unexpectedly the fourth leading cause of death among various carcinomas,with an overall five-year survival rate of merely 8.2% (in 2007-2013) for all stages[42,43].There are several factors leading to a poor prognostic performance of this devastating cancer,such as the deficiency of serum biomarkers for diagnosis and prognosis,the absence of biomarkers which could function as guidelines for individual therapy,and the broad and primary resistance to chemotherapy[43].The bacterial colony is critical to developing gastrointestinal mucosal immune system,maintaining a normal physiological circumstance,and providing necessary nourishment,which has been of significance in various disease states[44,45].Multiple observations have shown that there is an overlap between oral microbiota and digestive tract microbiota partly due to mastication and daily oral hygiene,such as tooth brushing and flossing[42],which promotes multiple avenues for the dissemination of dysbiosis[44].Furthermore,poor oral health is linked with an increased risk of pancreatic cancer development[46].Those who suffer from 2 types of periodontitis caused by oral microorganism tend to be subsequent at higher risks of increasing the occurrence of pancreatic cancer[47].A large European prospective cohort study found that elevated serum antibodies to the ATTC 53978 strain ofP.gingivaliscould triple the risks of pancreatic carcinoma[48].As Dr Miller recently demonstrated,P.gingivalisinitiated the Toll-like receptor (TLR)signalling pathways[49],while TLR activation critically contributed to pancreatic carcinogenesis in animal models[50].This result was considered direct evidence thatP.gingivalisincreases pancreatic cancer development.Additionally,high rates of tumour suppressor gene p53 mutations were detected in pancreatic cancer patients,and it was concluded that abnormality of the p53 gene is a significant event in human pancreatic tumourigenesis[51].In addition,in the progression ofP.gingivalisinhibiting epithelial cell apoptosis,p53 can be activated byP.gingivalisinvasion[52,53].As a result,mutations in p53 can play a role as a bridge that linksP.gingivaliswith the development of pancreatic cancer,but further investigations are needed to enrich this link.
In summary,P.gingivalismay be considered a biomarker in the occurrence and development of pancreatic cancer.It is urgent to conduct more research to explain the mechanism by whichP.gingivalisacts on pancreatic cancer and to improve the prevention and treatment of pancreatic cancer.Through these studies,it is hopeful to contain the high mortality of pancreatic cancer and release the tense status quo in pancreatic cancer.
PERIODONTAL DISEASE AND CANCERS
Periodontal disease is an inflammation that occurs in gums,which could induce the recession of gum,the damage of soft tissue,and the loss of bone and tooth (severe periodontitis)[54].The identification of the “red complex”,which consists ofTannerella forsythia,P.gingivalisandTreponema denticola,is a major milestone in the research of periodontal microbiology.In terms of esophageal adenocarcinoma risk,Tannerella forsythiahas to be found increasing this risk,while the exhaustion ofNeisseriaandStreptococcus pneumoniaewas related to lower risk,and the abundance ofP.gingivalistended to increase the risk of ESCC[55].Among these bacterial species,P.gingivalisshows the strongest association with periodontitis[56].Additionally,P.gingivalisacts as an independent risk factor for the above-mentioned cancers.Therefore,we further discuss the relationship between periodontitis and these cancers.Substantial investigations have accumulated evidence supporting that periodontitis causes the host maintain a chronic inflammatory state[57]and confirming that cancer is associated with chronic infections or inflammation[58].Taking the receptor to advanced glycation end products (RAGE) as an example,which is a multi-ligand receptor that can express on numerous cytomembrane and link with chronic infections,has been suggested to play a role in carcinogenesis[59].Consequently,we can conclude that periodontitis has direct effects on cancers.As a prospective cohort study revealed,periodontal disease might play the role of being a marker for a susceptible immune system or having a direct impact on cancer risk[60].Some others also suggested that there are positive connections between periodontitis and several tumours,including pancreatic carcinoma,lung tumours and digestive cancers[61,62].Tezalet al[63]concluded that chronic periodontal disease could function as a risk factor for oral premalignant lesions and cancers.OSCC patients are highly sensitive to chronic periodontitis,which suggests the existence of OSCC cells in a chronic inflammatory state.Since periodontitis is attributed to multiple bacterial pathogens,OSCC patients infected with such inflammation are in consistent exposure to excessive periodontal bacteria[64,65].These bacterial pathogens may subsequently affect the biological behaviour of oral cancer by modulating inflammatory mediators and invading related molecules[31].Chronic periodontitis not only affects the occurrence and development of oral cancer but also contributes to the metastasis of this cancer[29,31].The relationship between periodontitis and pancreatic cancer has also been revealed from a great deal of research.An evidence-based review showed that inflammation plays a key role in pancreatic cancer[66],and in a prospective cohort study of male health,professionals confirmed the strong positive association between periodontal disease and pancreatic cancer.In this cohort study,the existence of periodontal disease increases the risk of pancreatic cancer by 64%[46].The systemic dissemination of oral microorganism and their toxic substance may also cause systemic inflammation and immune reaction,which could trigger the incidence of pancreatic cancer[66-68].However,the role of oral microbiota in the development of pancreatic cancer is still under study.As mentioned in a former section of this review,periodontal disease could induce the loss of a tooth[54].A prospective study also suggested that tooth loss has increased the incidence of esophageal and gastric cancers,which may owe to the alterations of oral microflora and subsequent increased carcinogensin vivo[69,70].As a result,periodontal disease is connected with such tumours.In addition,the risk of lung tumour has been increased for those who suffering from periodontal disease in cohort studies,which may be because of the aspiration of oral pathogens into the lungs,the modification of the mucosal surface,the destruction of salivary pellicles,and the alteration of the respiratory epithelium[71].Periodontal disease may establish more connections with other cancers,such as bladder cancer,colorectal cancer and so on,but a large amount of research is needed to verify this connection.
PREVENTION AND TREATMENT OF CANCERS ASSOCIATED WITH P.GINGIVALIS INFECTION
The prevention and treatment to those digestive cancers are specific and complicated for the existence ofP.gingivalis.As a result,the intervention strategies are separate to antimicrobial therapy[72]and tumour site[73],but which both devote to thoroughly extracting carcinomas and managing good prognosis.
For thatP.gingivalisowns the characteristics of high genetic capability,this bacterium could resist any adverse environment that hindering its development;P.gingivaliscould also be capable of resisting various antibiotics that in use currently.In addition,the results of Deshpandeet al[74]’s study indicated thatP.gingivaliscan actively invade endothelial cells with the help of fimbriae.Because of the specificity of this bacterium,the cancer treatment related toP.gingivalisis more directional and targeted.First,screening forP.gingivalisin dental plaques may identify susceptible subjects,which could help decrease the occurrence of cancers.Second,we can improve oral hygiene to reduce the risk of cancer.Third,the use of antibiotics or other antibacterial strategies may prevent the progression of cancers[36].Blue light-emitting diode (BL) could inhibit the growth ofP.gingivalisand play antimicrobial roles,and antimicrobial photodynamic therapy combining BL and rose bengal was expected to be a new technology for the elimination of bacteria[72].Besides,AM404,an active metabolite of paracetamol,is an inhibitor of the growth and biofilm formation ofP.gingivalisand could potentially make guidance in developing new drugs that is specific to infections and cancers with regard toP.gingivalis[75].There are data suggesting that Kgp,a factor that playing the role of nutrition and toxicity forP.gingivalis,may act as the therapeutic point in controllingP.gingivalisinfections.On account of it relating to the inhibition of other bacterial pathogens,protease inhibitors may have a potential to be an emerging antibacterial drug[76].However,when cancers occur,treatment decisions are often complicated.The location,staging and resectability of the primary tumour,individual factors,such as swallowing function and airway condition,wishing to keep organ preserved,and coexisting diseases,all play roles in guiding accurate therapy.The main therapeutic approaches towards cancers are surgical therapy and radiotherapy[73].During the last decade,the introduction of intensity modulated radiation therapy and concomitant chemoradiation have substantially changed the treatment techniques in head and neck cancer[77]and solved problems caused by radiotherapy,such as rapidly progressing dental caries as well as fungal and bacterial infections[78,79].Recently,the chronological order between dental extractions and radiotherapy has also been fully demonstrated[80].As for oesophageal cancer,the avoidance of radiotherapy is a valid choice.And the combination of platinum-based chemotherapy and radiotherapy before operation is the first choice in treating resectable local oesophageal carcinoma.In addition,the use of cisplatin and 5-FU combined with chemo-radiotherapy is an effective strategy for the treatment of ESCC.Surgical retention is a salvage procedure for patients with persistent or recurrent diseases.Several multicentre trials regarding neoadjuvant treatment for pancreatic cancer to improve survival are in progress[81].With regard to pancreatic cancer,considering its characteristic of diagnosis in advanced stages,surgery tends not to be a selection;radiotherapy or chemotherapy is mainly used for palliative care[54].Neoadjuvant therapy has become increasingly important in recent years,and further changes in standards are still needed[82].The improvements in surgery,the advance of radiotherapy and the coordinated use of systemic drugs during treatment have clinically contributed to better outcomes of cancer patients[73].In summary,the combination of antimicrobial therapy againstP.gingivalisand tumour clearance with surgery,radiotherapy or chemotherapy,and neoadjuvant therapy is a good treatment for these digestive system cancers caused byP.gingivalis.However,the prognosises of digestive cancers are not eventually same.As Wooet al[21]put,those OSCC patients who were infected withP.gingivalisare discovered more metastatic foci in the lung than those who were non-infected;ESCC patients those with high levels of IgA or IgG againstP.gingivalistend to worse prognosis and those who were detected with high both IgA and IgG were associated with worst prognosis[40];Pancreatic cancer patients have suffered poor prognosis,partly for lacking diagnostic and prognostic biomarkers.It is better now for discovering the role ofP.gingivalisin this devastating carcinoma,which would guide personalized treatments,improve prognosis and enhance the quality of life[43].
POSSIBLE MECHANISMS OF CANCERS CAUSED BY P.GINGIVALIS
Regarding cancer,diverse degrees of connections betweenP.gingivalisand tumours of the buccal cavity,digestive tract or pancreas have been displayed in multiple clinical and experimental studies[26,48,62].The correlation of orodigestive cancer mortality toP.gingivaliswas first and directly illustrated in a cohort study from Ahnet al[62],who pinpointed thatP.gingivaliswould also act as a microbial marker full of value in such carcinomas.In this study,non-parametric trend analysis for all subjects also showed an increase in orodigestive cancer mortality with the increase of anti-P.gingivalisIgG levels[62].P.gingivalisinteracts with host epithelium in varieties of aspects,which may provide basis at molecular level for potential mechanisms carcinogenesis mediated by this bacterium.In addition toP.gingivalisinducing the invasion of tumour cells and activating TLR mentioned above[30,31,33,50],other possible mechanisms have also been identified.First,nucleoside diphosphate kinase (NDK)excreted byP.gingivalisis capable of promoting tumourigenesis.The NDK inhibits ATP activation of purinergic receptor (P2X7) receptors and consequently depress the production of IL-1β in epithelium[83].In that IL-1β plays a crucial role in priming IFNγ which could produce CD8+T cells that specific to tumour antigen,and NDK secreted byP.gingivaliscan also make tumour escape from immune surveillance[39].The degradation of ATP mediated by NDK also suppresses apoptosis,which is dependent on ATP activation of P2X7 receptors[84].Moreover,the phosphorylation of heat shock protein 27 (HSP27) by NDK fromP.gingivalisconfers an antiapoptotic phenotype to primary gingival epithelial cells,suggesting that HSP27 is a critical molecule for the suppression of host cell apoptosis caused byP.gingivalis[85].Second,Yilmazet al[84]have noted that the inhibition of epithelial cell apoptosis is an important carcinogenic effect ofP.gingivalisand is also an intrinsic protective mechanism of cancerous cells.Activating the Jak1/Akt/Stat3 signalling,increasing the Bcl2 (anti-apoptosis):Bax(pro-apoptosis) ratio,curtailing releasing pro-apoptotic factor cytochrome c,and blocking activating both caspase-9 and the executioner caspase-3 may all contribute to this progression[38,86,87].In addition,P.gingivalismodulates the expressing levels of microRNAs (miRNAs),and the upregulation of miR-203 caused byP.gingivalisresults in the decreasing levels of negative regulator SOCS3 and subsequently suppressing apoptosis of epithelium[88].Since SOCS3 can bind to phosphorylated JAK receptors,SOCS3 consequently inhibits JAK/STAT3 signalling[89].Third,P.gingivalisinfection induces expression of the B7-H1 receptor which belongs to the B7 family and plays a significant regulatory role in immunologic reaction mediated by cells[90,91],suggesting that this pathogen is involved in transferring to the distant and advancing nuclear grading of carcinoma cells[92].On the other hand,B7-H1 receptors-mediated costimulatory signal could cause the anergy and apoptotic effect of those activated T cells,which subsequently make tumours evade immune reaction[93].Fourth,those carcinogenesis caused byP.gingivalisalso contributes to metabolising potential carcinogen.For instance,P.gingivaliscould dehydrogenate ethanol to acetaldehyde which is a carcinogenic derivative and capable of making the damage of DNA,the mutation and excessive proliferation of the epithelial cells[24,25].Certainly,the above contributions could suitably explain why excessive drinking is a risk factor for orodigestive cancer[39].Lastly,P.gingivalisestablishes chronic infections that involve intracellular persistence within epithelial cells[94].Chronic inflammation has a close connection with the development of cancer for the release of inflammatory factors,such as IL-6,which can promote tumourigenesis by causing DNA hypomethylation as well as aberrant changes in promoter hypermethylation[95].All the above-mentioned possible mechanisms of cancers caused byP.gingivalisare shown in Figure 1.
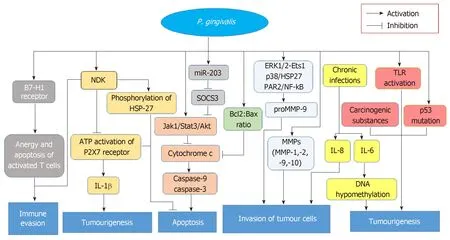
Figure 1 Possible mechanisms of cancers caused by Porphyromonas gingivalis.
CONCLUSION
P.gingivalisis involved in periodontal disease and several cancers.This bacterium not only independently affects the development of cancers by RgpA,RgpB and Kgp[11,12]but also indirectly impacts cancersviaperiodontal disease that causes the host be in an inflammatory state[57,58].One critical carcinogenesis caused byP.gingivalisis inhibiting the apoptotic effects of epithelium,which also function as the intrinsic protective mechanism of cancer cells[87].P.gingivalishas a strong association with oral cancer,and the treatment of oral cancer is abundant and has been improved in the clinic.The significant function ofP.gingivalisin oesophageal cancer was conducted by Gaoet al[36]in 2017,which was considered a breakthrough in the research of oesophageal cancer and indicated thatP.gingivaliscan be an important biomarker for monitoring the occurrence and progression of this cancer.For pancreatic cancer,the evidence concerning the role ofP.gingivalisis still limited,while the relationship between periodontal diseases and pancreatic cancer is very large[66-68].Therefore,more investigations are still needed to reduce the incidence,increase the five-year survival rate and improve the treatments for this devastating cancer.Collectively,maintaining oral hygiene,seeking more biomarkers,improving therapeutic measures,and improving the prognosis of these diseases are the focus for clinical research and work in the future.
 World Journal of Clinical Cases2019年7期
World Journal of Clinical Cases2019年7期
- World Journal of Clinical Cases的其它文章
- Ultrasound imaging of abdominal sarcoidosis:State of the art
- Clinical evaluation of endoscopic resection for treatment of large gastric stromal tumors
- Value of superb micro-vascular imaging in predicting ischemic stroke in patients with carotid atherosclerotic plaques
- Open anterior glenohumeral dislocation with associated supraspinatus avulsion:A case report
- Vein of Galen aneurismal malformations - clinical characteristics,treatment and presentation:Three cases report
- Non-lnvasive management of invasive cervical resorption associated with periodontal pocket:A case report
