Body mass index trends and quality of life from breast cancer diagnosis through seven years' survivorship
Allison Brandt Anbari, Chelsea B Deroche, Jane M Armer
Abstract BACKGROUND Weight gain is a potential negative outcome of breast-cancer treatment, occurring in 50%-to-96% of breast-cancer patients, although the amount of weight gain is inconsistently reported in the literature. Research has also shown a relationship between overweight/obesity and breast-cancer mortality. Correspondingly,weight management is a self-care approach known to benefit quality of life(QOL). These research questions and analysis add to existing literature by examining participants’ body mass index (BMI) trend and its relationship with QOL indicators over seven years.AIM To examine: (1) BMI trends among breast cancer survivors; and (2) The trends’relationship to QOL indicators over seven years.METHODS During the Breast Cancer and Lymphedema Project, 378 patients’ weight and height were recorded by nurses prior to or just after beginning breast cancer treatment and repeated at quarterly-to-semiannual intervals over seven years.Additionally, participants annually completed the 36-Item Short Form Health Survey (SF-36), a valid and reliable tool assessing QOL and health concepts,including physical function, pain, and emotional well-being. BMI trends, change in BMI, and change in SF-36 subscales over seven years were calculated using a random-intercept repeated-measures regression. Patients were placed into BMI categories at each time point: Normal, Overweight and Obese. As patients’weights changed, they were categorized accordingly.RESULTS During the seven-year study and while controlling for age and residence,participants gained an average of 0.3534 kg/m2 (P = 0.0009). This amount remained fairly consistent across BMI categories with those in the normal-weight category (n = 134) gaining 0.4546 kg/m2 (P = 0.0003); Overweight (n = 190)gaining 0.2985 kg/m2 (P = 0.0123); and obese (n = 199) gaining 0.3147 kg/m2, (P =0.0649). Age (under or over 55) and region (metro/micro vs small/rural) were significantly associated with BMI increase in both the normal and obese categories. There were statistically significant (P < 0.0100) changes in five of the eight SF-36 domains; however, the directions of change were different and somewhat divergent from that hypothesized. Controlling for age and region,these five were statistically significant, so there were no change or differences between the micropolitan/metropolitan and small town/rural groups.CONCLUSION Although only modest increases in mean BMI were observed, mean BMI change was associated with selected QOL indicators, suggesting the continued need for self-care emphasis during breast cancer survivorship.
Key words: Breast cancer; Survivorship; Breast cancer treatment effects; Quality of life
INTRODUCTION
There are 3.5 million breast cancer survivors (BCS) living in the United States[1].Increasingly, women diagnosed with breast cancer are living longer and healthier lives. However, they are at a lifelong risk for developing complications from their previous cancer treatments[2]. Knowing this, emphasis has been placed on survivorship care-planning which highlights the specific needs of BCS, including mitigating the psychological and physical effects of treatment, as well as promoting healthy behaviors[2].
Breast cancer treatment and weight gain
Weight gain is a potential negative outcome of breast cancer treatment, occurring in 50% to 96% of breast cancer patients[3]. More recently, Raghavendra et al[4]found that 33.7% of 1281 long-term survivors in their study gained more than 5% of their pretreatment weight after 5 years of endocrine therapy. That said, the amount of weight gain and reasons for it remain inconsistently reported in the literature[5-9]. Research has also shown a relationship between overweight/obesity and breast-cancer mortality[3,8,10].
Breast cancer treatment and quality of life
Both weight loss and gain remain common after treatment for breast cancer, with weight loss being a marker for mortality risk[5]. Moreover, weight gain after breast cancer diagnosis (treatment) has been associated with higher risk for co-morbid conditions such as diabetes and cardiovascular disease[11]. However, weight gain or a higher body mass index (BMI) at diagnosis have also been found to actually increase certain quality of life (QOL) domains[12]. Regardless of amount or timing, weight gain and body changes caused by cancer treatments are known to cause distress among BCS[9,13].The impact of a breast cancer diagnosis and treatment sequelae on QOL domains can vary depending on the age and rural/urban residence of the survivor. The median age of a BCS is 62 years which means they typically have many additional years of specific survivorship care ahead of them, activities involving special screening and/or symptom management[1]. In addition, BCS living in rural areas may face different challenges than their urban counterparts. First, women living in rural settings are more likely to have higher BMI at diagnosis of breast cancer[14].Furthermore, rural BCS may face additional difficulties in accessing follow-up care,adjusting to new roles or limitations, and navigating mental health changes[15].
Purpose
This study’s purpose was to examine: (1) BMI trends among BCS; and (2) The trends’relationship to QOL indicators over seven years’ survivorship as measured by the 36-Item Short Form Survey (SF-36). Research questions were: (1) How do patients’ BMI change from breast cancer diagnosis to seven years’ survivorship? and (2) When controlling for age and rural residence, what is the relationship between BMI change and QOL (as indicated by change in SF-36 subscale scores) from diagnosis to seven years’ survivorship?
MATERIALS AND METHODS
Data collection
During the Breast Cancer and Lymphedema Project, 378 women diagnosed with breast cancer agreed to have their weight and height recorded by nurses prior to or just after beginning breast cancer treatment as a part of their overall survivorship assessment[16]. An initial height was measured in centimeters by the research nurses using a wall-mounted height rod. Weight measurements using a standing scale were repeated at quarterly-to-semiannual intervals over the following seven years (17 total possible visits; Visit 1 through Visit 17). For analysis purposes, Time 1 was either right after diagnosis or right after the first treatment (surgery). Time points from that point forward corresponded to quarterly, semi-annually, and annual measurements during study enrollment. The study was approved by the Health Sciences Institutional Review Board and all participants signed an informed consent.
BMI was calculated using the participant’s weight in kilograms divided by the square of her height in meters (kg/m2). BMI was calculated and recorded for each study visit. For this analysis, participants were assigned into one of three BMI categories of Normal (BMI equal to 18.5000 to 24.9999), Overweight (BMI equal to 25.0000 to 29.9999), and Obese (BMI greater than or equal to 30.0000). The six participants with BMIs in the Underweight category (BMI less than 18.5000) were included in the Normal category for analysis.
Participants’ dates of birth were collected upon enrollment in the study and used to calculate age by comparison to date of each data collection time point. Participants’zip codes were collected upon enrollment in the study at the time of diagnosis.Participants were placed into two categories using the Rural-Urban Commuting Area Codes (RUCA) for zip code categorization process provided by United States Department of Agriculture[17]. For this analysis we chose to compare Micropolitan/Metropolitan and Small Town/Rural.
Finally, participants completed the SF-36 annually. Participants were given the survey to fill out on their own and return to the research office. The SF-36 is a valid and reliable tool assessing QOL and health domains, including physical function,pain, and emotional well-being[18]. The SF-36 is publicly available and has been frequently used to assess breast cancer and QOL[19,20]. It includes eight health concepts or subscales: (1) Limitations in physical activities; (2) Limitations in social activities;(3) Limitations in usual role activities; (4) Pain; (5) Mental health; (6) Limitations in role activities related to emotional well-being; (7) Vitality; and (8) General health perceptions[15]. The SF-36 survey has consistent reliability; 0.93 (physical functioning)and 0.90 (mental health); to 0.82 to 0.85 (bodily pain, emotional and physical attribution, and social functioning); to 0.78 (general health perceptions)[21].
Data analysis
BMI trends:Patients were placed into one of the three BMI categories at each time point: Normal, Overweight, and Obese. As a patient’s weight changed, she was recategorized accordingly. Using a random-intercept repeated-measures regression analysis, BMI trends within each of the BMI categories were assessed using a sample size equal to 322 and 4059 observations. This method was used because the data were rich and longitudinal and allowed accounting for the non-dependency between observations within a participant[22]. Results of this method modeled the average BMI change over time, while also controlling for other influences on BMI change, such as region and age. The random-intercept model allows each person to have her own starting point (intercept) while the slopes are assumed equal.
Using the 2010 RUCA codes, participants were grouped into two regional categories: micropolitan/metropolitan (more than 50000 persons); and rural/small town (less than 49999)[17]. Using just above the median age of the natural onset of menopause[23], which can influence weight changes, participants were grouped into two categories: Under 55 years of age and equal to or over 55 years of age.
Change in BMI and SF-36 subscale scores:Change in BMI and its relationship to the SF-36 scores in each of the eight QOL domains was calculated using a repeatedmeasures general linear mixed model with a variance components covariance structure. The variance components covariance structure assumes equal correlation between any two time-points, in this case, visits[22]. BMI change was the dependent variable and the change in the eight SF-36 domains were the independent variables,while controlling for age categorized into two groups (under 55 and equal to or over 55 years) and region categorized into two groups (micropolitan/metropolitan and rural/small).
RESULTS
BMI trends
During the seven-year study (visit 1 to visit 17), participants gained an average of 0.3534 kg/m2(P = 0.0009). This modest gain remained fairly consistent across BMI categories, with those in the Normal category (n = 134) gaining 0.4546kg/m2(P =0.0003); Overweight (n = 190) gaining 0.2985 kg/m2(P = 0.0123); and Obese (n = 199)gaining 0.3147 kg/m2, (P = 0.0649) as seen in Table 1 and Figures 1-3. For the normal BMI group, visit (time variable) was significant which indicates that on average, the normal group’s BMI changed significantly by 17 × 0.0267 or 0.4546 kg/m2from visit 1 to visit 17 (P = 0.0003). Likewise, for the overweight BMI group, visit (time variable)was significant which indicates that on average, the group’s BMI changed significantly by 17 × 0.01756 or 0.2985 kg/m2from visit 1 to visit 17 (P = 0.0123).Results were consistent for the obese group, with an estimated BMI increase of 0.0185× 17 or 0.3146 kg/m2; however, this change did not meet the level of statistical significance (P = 0.0649). Age (under or over 55) and region (micro/metro vs rural/small) were significantly associated with BMI increase in both the normal and obese categories (P < 0.0500 for both categories).
Change in BMI and SF-36
BMI change corresponded significantly (P < 0.0500) to five SF-36 domain scores:Physical functioning; role limitations related to physical functioning; role limitations related to emotional problems; social functioning; and energy/fatigue (Table 2). The relationships with these five domains were statistically significant when controlling for age and commuting region; however, there were no change or differences between the micropolitan/metropolitan and small town/rural groups. Referring to Table 2 and extrapolating this further, each domain is scaled to range zero to 100. If a person’s score changes from a 0 to 100 score, which would be extreme, but not necessarily impossible, within our sample, their BMI is expected to decrease by 0.5120 kg/m2.Considering the overweight BMI category is only 4.9000 kg/m2wide (25.0000-29.9 kg/m2), this could be a clinically significant change.
There were statistically significant changes in five of the eight SF-36 domains;however, their directions of change were varied and somewhat divergent from what one might hypothesize, as one might presume that QOL in each domain would decrease somewhat with weight gain. Although modestly, three QOL domains moved statistically significantly in the opposite direction as BMI - that is, as BMI increased,the participants’ QOL decreased, as would be hypothesized. These domains were:Physical functioning (SE = -0.0093; P = 0.0052); role limitations related to emotional problems (SE = -0.0039; P = 0.0216); and energy/fatigue (SE = -0.0104; P = 0.0045).
The remaining two statistically-significant QOL-affected domains, role limitations related to physical functioning (SE = 0.0039; P = 0.0052); and social functioning (SE =0.0079; P = 0.0014), moved in the same direction as BMI, as would not necessarily be hypothesized to occur. For example, as social functioning increased, BMI is expected to also increase by 0.0082 kg/m2.

Table 1 Parameter estimates for association with body mass index by age (two categories), region, and time
DISCUSSION
This analysis adds to the literature regarding weight changes during breast cancer treatment. Like previous findings, slight BMI changes were observed over the seven years post-diagnosis. The slight change was not surprising, as weight change over time of BCS has been found to be similar to non-BCS[24]. This finding could be supported by a number of possible reasons. Few studies control for location of residence (commuting region). Because residence was statistically significant and associated with weight gain, future research about residence and risk for weight gain for women diagnosed with breast cancer could reveal additional approaches to addressing this groups’ survivorship needs. There is also the possibility that, despite an intervention not being implemented during this prospective study, participants might have adjusted their health behaviors simply because they were being monitored over time. Thus, only slight BMI changes over seven years were realized.
BMI change was also modestly associated with selected QOL indicators, even when controlling for age and commuting region. Our results support previous studies that have found slightly overweight women might maintain a better QOL or observe less QOL changes, than their normal, obese, or even non-cancer counterparts[11]. Our results also support previous studies that found only slight weight gains over time with no association with age[4]. There is also the possibility that participants adjusted to their health status changes over the seven years of participation and thus only small changes in their QOL were reported. Similar findings were presented in a study by Tessier, Blanchin, and Sebille where an adaptation and shift in BCS’ subjective well-being and health-related QOL were noted over time[25].
Limitations
This analysis did not control for or factor in the varying treatment regimens of participants. Different types and stages of breast cancer are approached differently and thus the long-term effects of treatment vary widely. Including types of treatments as a variable, with this already-limited sample size of 379 participants, would have weakened the power of the modeling used. A final consideration with this analysis is the age of the data collection time period of 2001 to 2008. Oncological surgical practices (e.g., breast conservation surgery and sentinel lymph node biopsy),neoadjuvant and adjuvant chemotherapy treatments, as well as duration, amount,and localization of radiation sessions, have evolved since completion of the data collection.
Implications for practice
The modest increases in BMI, paired with modest changes in QOL, suggest the continued need for self-care emphasis during breast cancer survivorship. Self-care optimally includes weight management at a current state during treatment and survivorship, rather than an emphasis on weight loss. Young et al[26]found that BCS who gained weight or lost weight had a higher risk of functional limitations.Furthermore, exercise can improve physical function and body composition without overt weight loss, thus supporting encouragement of increasing physical activity and weight maintenance (rather than weight loss alone)[10]. These results support this finding that perhaps an emphasis on weight maintenance during and after treatment is a key component of survivorship care-planning. Rather than emphasis on weight loss, perhaps the approach and future research should surround weight maintenance(or prevention of weight gain) that involves increased physical activity and dietary adjustments, both known to reduce fatigue, increase cardiovascular health, and perhaps decrease body fat percentages[27]. Our findings support the notion that survivorship care-planning should involve the patient and should factor in age,commuting region, late side-effects, and health promotion[2,28].
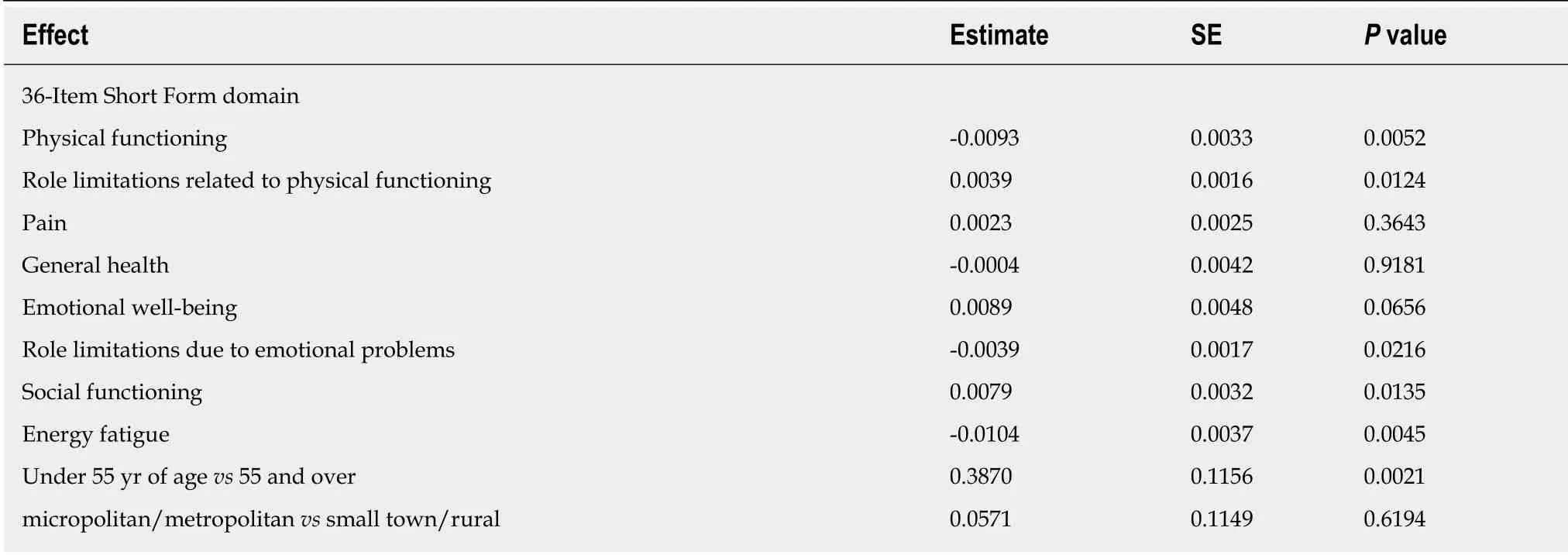
Table 2 Statistically significant changes in 36-ltem Short Form Survey domain scores

Figure 1 Normal body mass index trends over time comparing age group and region.

Figure 2 Overweight body mass index trends over time comparing age group and region.

Figure 3 Obese body mass index trends over time comparing age group and region.
ARTICLE HIGHLIGHTS
Research background
Weight gain is a potential negative outcome of breast-cancer treatment, occurring in 50%-to-96%of breast cancer patients, although the amount of weight gain is inconsistently reported in the literature. Weight gain can influence quality of life (QOL) during survivorship and even cancer reoccurrence.
Research motivation
We were motivated to do this analysis to examine body mass index (BMI) trends among breast cancer survivors and the trends’ relationship to QOL indicators over seven years. Identifying trends and their relationships to QOL provides insight into cancer survivorship care and careplanning.
Research objectives
We conducted this analysis to assess BMI trends among breast cancer survivors and to investigate whether those trends were related to quality of life. We identified small positive upticks in BMI over time amongst our participants. Future research should continue to examine weight changes in this population.
Research methods
Data for this analysis were collected during a study entitled the Breast Cancer and Lymphedema Project. Three-hundred seventy-eight women enrolled in the study at breast cancer diagnosis or just after surgery for breast cancer treatment. Participants were followed over seven years and the research team recorded their weight and 36-Item Short Form Survey (SF-36) scores at designated intervals during the study. BMI trends, change in BMI, and change in SF-36 subscales over seven years were calculated using a random-intercept repeated-measures regression. This method was selected because the data were longitudinal, and it allows for non-dependency between collection time points.
Research results
We found small upward trends in our participants’ BMI and those upward trends corresponded in a statistically significant way to several of the SF-36 subscales. Age and region were also significantly associated with BMI increase in the normal and obese BMI categories. Our results add to the existing body of work regarding BMI and breast cancer treatment. These results contribute to what is known and support efforts to continue research into breast cancer survivorship and the potentially chronic sequelae of treatment.
Research conclusions
We place an emphasis on the need for continued support and surveillance through the years of survivorship. Our results support continued research in breast cancer survivorship research.Application of weight management and health promotion for survivorship care-planning in the clinical setting has potential to enhance optimal self-care and QOL in living with a chronic condition such as breast cancer survivorship.
Research perspectives
We believe future research involving breast cancer survivors should go beyond weight loss and perhaps focus more on weight management, healthy lifestyle changes, and health promotion.Our results also bring awareness to the potential influences of rural and urban environments and how those environments may contribute to our understanding of the issues surrounding cancer survivorship.
ACKNOWLEDGEMENTS
The research team would like to thank the research nurses and graduate student research assistants who assisted with the collection and management of these data and the cancer center clinical team who supported this research. We would especially like to thank the breast cancer survivors who volunteered to participate to help future survivors.

