Left Ventricular Dysfunction in Ischemic Heart Disease
Robert F.Hamburger,DO,MPH,FACC
1 University of Florida College of Medicine,Malcom Randall VA Medical Center,Gainesville,FL,USA
Abstract
Keywords: ischemic heart disease;ischemic cardiomyopathy;heart failure;viability
Introduction
With the increasing prevalence of risk factors for coronary artery disease (CAD),such as diabetes,hypertension,and obesity,the contribution of ischemic heart disease as the primary cause of heart failure has increased.Data from the Framingham Heart Study showed the prevalence of coronary disease as the cause of heart failure increased by 41% per calendar decade in men and 25% in women [1].For this reason,it is important for cardiologists to have a general awareness of the interplay between CAD and left ventricular (LV)dysfunction.
This review discusses the key elements of the pathophysiology of ischemia in L V dysfunction,modes of myocardial viability assessment,medical management,and the role of revascularization in ischemic cardiomyopathy.
Principles of Ischemic Heart Disease and the Relationship with Hibernation and Stunning
Stunned Myocardiu m
Prolonged ischemia can result in L V systolic dysfunction [2].It is important to distinguish between the concepts of stunned and hibernating myocardium.Stunned myocardium occurs when there is total or near total coronary fow reduction for 5- 15 minutes with a related abnormality in regional LV wall motion that after reperfusion typically lasts for hours to days [3,4].It is essentially a persistence of LV dysfunction after reperfusion with normal fow and despite the absence of irreversible damage [5].The key points of this def nition are a brief fow reduction with eventual reperfusion with L V dysfunction that persists for a short time.Dysfunction can remain for up to 6 hours after the ischemia has resolved,and includes demand ischemia such as that related to exercise [3].
Hibernating Myocardium
Hibernating myocardium represents resting L V systolic dysfunction due to reduced coronary blood fow that can be partially or completely reversed with revascularization [3,6].Decreased systolic function is thought to represent a mechanism to allow equilibrium between myocardial function and coronary blood fow-a concept referred to asperfusion-contraction matching[6-8].In chronic hibernation there are structural changes that further allow the myocardium to adapt to reduced fow [3,8].Viability studies typically help to determine the dif ference between hibernating myocardium and myocardial infarction (MI)as opposed to stunned myocardium since resting fow is normal in stunned myocardium.In both hibernating and stunned myocardium,there is a conversion from free fatty acid metabolism to glucose metabolism-a concept that allows us to study viability using f uorine-18-labeled deoxyglucose (18FDG)PET [3,7,8].
A summary of the key concepts of hibernating and stunned myocardium is given in Table 1.
Prognosis in Ischemic Cardiomyopathy and Ventricular Remodeling
Ischemic cardiomyopathy is usually seen in patients with coronary stenosis of 75% or greater in one of the three major epicardial vessels in the setting of an ejection fraction of less than 40% with New York Heart Association class II or greater symptoms [9].The presence of LV systolic dysfunction and CAD is known to have a poorer prognosis,which worsens as the degree of CAD increases.Coronary Artery Surgery Study registry data showed that the 12-year survival rate of patients with normal coronary arteries was 91%,compared with 74% for those with one-vessel disease,59% for those with two-vessel disease,and 40% for those with three-vessel disease,and there was a signif cant effect of LV dysfunction in this population.The 12-year survival rate of patients with at least one-vessel CAD and ejection fraction less than 35% was 21%,compared with 73% in those with ejection fraction greater than 50% (P < 0.0001)[10].
Ventricular Remodeling
Ventricular remodeling is an important response to myocardial ischemia and MI.In the initial phase after MI,scar formation occurs in the infarct zone along with thinning and elongation of the myocar -dial f bers.At this point L V volumes increase in what is likely an initial adaptive response.This is followed by a more maladaptive phase of myocyte hypertrophy in the noninfarct zone,at which point the LV cavity evolves from a more elliptical shape to a more spherical shape,further compromising mechanical function [11].
Greater degrees of ventricular remodeling have been shown to have an effect on clinical outcomes.White et al.[12] showed that patients after MI with greater degrees of LV remodeling signif ed by elevated end-systolic volume had an elevated risk of post-MI death.The VALIANT study showed that increased end-diastolic volume,lower ejection fraction,and increased infarct segment length after MI were related to an increase in the composite of death and hospitalization for heart failure [13].
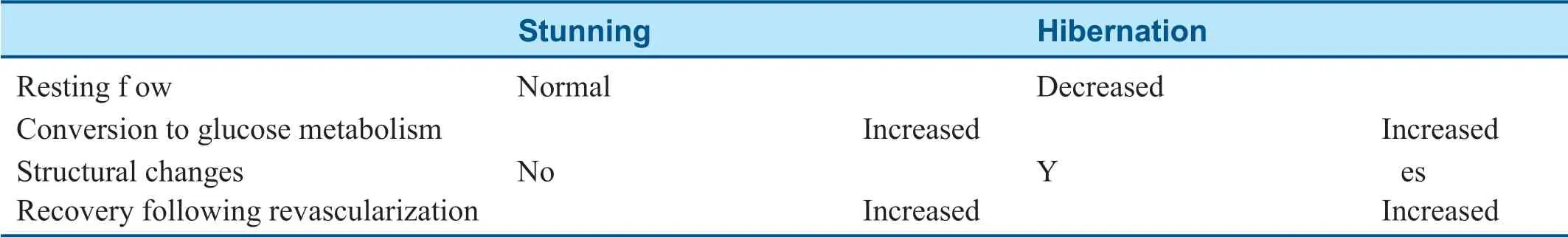
Table1 Comparison between Myocardial Hibernation and Stunning.
Myocardial Viability
Myocardial stunning and myocardial hibernation are both potentially reversible states of LV dysfunction with revascularization.The extent to which regional LV wall motion will improve following revascularization depends on the viability of the region in question.There are multiple methods for assessing myocardial viability,and a brief discussion of each modality follows.
Dobutamine Stress Echocardiography
With low levels of dobutamine,viable myocardium may show increased contractility with recruitment of contractile reserve.With higher levels of dobutamine,ischemia becomes the predominant factor and wall motion worsens.This biphasic response to dobutamine is the best predictor of myocardial viability in dobutamine stress echocardiography and the one most predictive of recovery following revascularization [14,15].In this situation,infusion of low-dosage dobutamine (5-10 µ g/kg/min)improves contractility initially,with further decline in contractility at higher dosages (up to 40 µ g/kg/min)as greater degrees of ischemia occur.
Thallium Single-Photon Emission Computed Tomography
Thallium-201 is injected at rest,and a perfusion abnormality is visualized that could be caused by f brosis from a prior infarct or resting hypoperfusion in the setting of hibernation.Repeated images are typically taken at 24 hours,with viable myocardium showing redistribution in the region where the resting perfusion abnormality was previously visualized.A f xed defect on both rest and redistribution imaging suggests f brosis without viability [16].
Technetium Single-Photon Emission Computed Tomography with Nitroglycerin
Technetium-99m does not have the propensity of thallium-201 to redistribute in the myocardium.
However,immediate administration of nitrates has been shown to increase resting fow in viable territories [17].After resting technetium-99m imaging,a perfusion abnormality is recognized on resting images.The patient is then given nitroglycerin sublingually,and repeated imaging is performed,with viability noted by an improvement in the prior resting perfusion abnormality [16].
Positron Emission Tomography
As mentioned previously,hibernating myocardium changes its metabolism from free fatty acids to glucose;thus uptake of a glucose analog,18FDG,by myocytes in an area of regional dysfunction would indicate viable myocardium.After a period of glucose loading,imaging with a traditional myocardial positron emission tomography (PET)tracer such as rubidium-82 is performed and a resting perfusion abnormality is identif ed.18FDG PET is then performed,with viable myocardium representing tracer uptake in the region of the resting perfusion abnormality,hence showing a mismatch pattern [16].
Magnetic Resonance Imaging
Cardiac magnetic resonance imaging typically detects viability by measuring the length of transmural scar by late gadolinium enhancement since areas of signif cant f brosis will retain gadolinium.Viability is typically def ned as a scar of 50% or less transmural thickness [18].
The role of myocardial viability has remained somewhat controversial owing in part to trials such as the STICH trial.The viability substudy of the STICH trial failed to show reduction in the primary end point,overall mortality,between those treated with coronary artery bypass grafting (CABG)and those treated with medical therapy (P = 0.21),although secondary end points showed a signif cant reduction in cardiovascular mortality (28 vs.33%,P = 0.05)[19].However,this study has been criticized in that it did not randomize patients on the basis of viability (which could lead to selection bias)and it also used older methods of viability in dobutamine stress echocardiography and single-photon emission computed tomography as opposed to PET and magnetic resonance imaging,which may be more reliable at predicting outcomes.For example,the Ottawa-FIVE study noted a reduction in the composite end point of cardiac death,MI,and cardiac rehospitalization in patients with L V dysfunction receiving18FDG PET- assisted management compared with standard care [20].Nonetheless,further randomized trials are needed to test the ef fect of viability on clinical outcomes in a prospective fashion.
Medical Therapy for Ischemic Cardiomyopathy
ACE Inhibitors
Numerous large randomized trials have evaluated the usefulness of ACE inhibitors in patients after MI.In ISIS-4 and GISSI-3,therapy with ACE inhibitors was started within 24 hours after an MI (with most events being ST -segment-elevation MI receiving f brinolysis)and even though the duration of therapy was brief (1 month in ISIS-4 and 6 weeks in GISSI-3),there were demonstrable reductions in mortality and improvements in L V function for months after therapy was stopped [21,22].
The SAVE trial determined whether long-term therapy with captopril reduces morbidity and mor -tality in patients with L V dysfunction after MI.Long-term captopril therapy over a mean 3.5-year period signif cantly increased overall survival rates (19% risk reduction,95% conf dence interval [CI] 3-32%,P = 0.019),including a signif cant reduction in the risk of death due to cardiovascular causes (21% risk reduction,95% CI 20-50%,P < 0.001),and reduced risk of recurrent MI,development of severe heart failure,and congestive heart failure requiring hospitalization [23].The TRACE trial with trandolapril and the AIRE trial with ramipril showed similar reductions in mortality and progression to severe heart failure [24,25].
Angiotensin II Receptor Blockers
Two large clinical trials have compared the use of angiotensin II receptor blockers with ACE inhibitors after MI in patients with heart failure,with the OPTIMAAL trial comparing losartan with captopril and the VALIANT trial comparing valsartan with captopril.Neither trial showed a signif cant difference between the two classes with regard to allcause mortality,with the VALIANT trial conf rming noninferiority.There was less cough or angioedema in the group that received angiotensin II receptor blockers [26,27].
Beta-Blockers
The CAPRICORN trial investigated the use of carvedilol in patients with acute MI and LV ejection fraction of 40% or less and showed reductions in all-cause and cardiovascular mortality,and the rate of recurrent,nonfatal MIs [28].
The CHRISTMAS trial was designed to test the hypothesis that patients with L V dysfunction and viable myocardium would have a greater response in ejection fraction to carvedilol than patients with nonviable myocardium.The trial showed an over -all increase in ejection fraction in patients given carvedilol compared with patients given placebo but did not show a statistically signif cant difference in ejection fraction increase between patients with nonviable myocardium and patients with viable myocardium.The study showed a linear trend between the number of viable segments and ejection fraction increase (P < 0.0001)[29].
Aldosterone Antagonists
The EPHESUS trial studied the use of eplerenone in patients with an acute MI as well as LV dysfunction and heart failure.The trial showed signif cant reductions in overall death (relative risk 0.85,95% CI 0.75-0.96,P = 0.008)and cardiovascular death (relative risk 0.83,95% CI 0.72-0.94,P = 0.005)[30].Because of the results of EPHESUS,American College of Cardiology/American Heart Association guidelines have given a class I,level of evidence B recommendation for use of aldosterone antagonists after MI with ejection fraction less than 40% in patients receiving a therapeutic dose of an ACE inhibitor and a beta-blocker [31].Despite this class I,level of evidence B guideline,physician adher -ence has been as low as 9.3% in eligible patients on hospital discharge [32].
Revascularization
Most of the data on outcomes of revascularization in patients with CAD and L V dysfunction come from trials on coronary artery bypass sur gery.The largest clinical trial evaluating CABG in patients with L V dysfunction was the STICH trial,which tested the hypothesis that revascularization would improve outcomes compared with medical therapy alone.The primary outcome of death from any cause was not statistically signif cant in the CABG group compared with the group that received medical therapy alone (P = 0.12)but there were lower rates of death from cardiovascular causes (28 vs.33%,hazard ratio [HR] 0.81,95% CI 0.66-1.00,P = 0.05)and of the combined outcome of death from any cause and hospitalization for cardiovascular causes (58 vs.68%,HR 0.74,95% CI 0.64-0.85,P < 0.001).However,17% of the patients in the medical therapy arm under -went CABG,and with adjustment for crossover,the primary outcome was signif cant (HR 0.7,95% CI 0.58-0.84,P < 0.001)[33].Post hoc analysis also showed that in patients with reasonable exercise capacity def ned as a physical activity score greater than 55 and a 6-minute walk distance of 300 m or more,mortality was signif cantly lower in the CABG group (HR 0.71,95% CI 0.52- 0.97,P = 0.033)[34].
Trials regarding the long-term outcomes of revascularization with PCI in patients with chronic L V systolic dysfunction are lacking.A propensitymatched study of patients with multivessel disease and severe L V systolic dysfunction (election fraction of 35% or less)comparing patients who underwent PCI with everolimus-eluting stents ver -sus patients who underwent CABG showed a lower risk of long-term stroke,similar risk of long-term death,and a higher risk of MI and repeated revascularization [35].A meta-analysis by Kunadian et al.[36] showed acceptable in-hospital mortality (1.8%)and long-term mortality (15.6%)in patients undergoing PCI with LV systolic dysfunction with similar outcomes to CABG.However,most of the studies included were performed either in the era before the use of drug-eluting stents or with f rstgeneration drug-eluting stents,but drug-eluting stents and pharmacotherapy have improved since these trials were conducted.At the time writing,the REVIVED-BCIS2 randomized trial is enrolling participants to study the ef fect of PCI on survival in patients with LV systolic dysfunction,but results have not yet been released [37].Perhaps at the conclusion of this trial we will have a better answer regarding clinical outcomes in this population.
Conclusion
LV dysfunction with ischemic heart disease is a prevalent problem.The pathophysiology,including myocardial stunning,hibernation,and viability,has been discussed here,and while there are numerous methods of assessing viability,more prospective trials are needed to assess clinical outcomes.Revascularization with coronary artery bypass sur gery may be of benef t to patients with L V dysfunction and multivessel coronary disease,but more research is needed to assess outcomes in patients receiving PCI.
Conflict of Interest
The authors declare that they have no conf icts of interest.
 Cardiovascular Innovations and Applications2019年1期
Cardiovascular Innovations and Applications2019年1期
- Cardiovascular Innovations and Applications的其它文章
- Diabetes Mellitus and Stable Ischemic Heart Disease
- Contemporary Management of Patients with Stable Ischemic Heart Disease
- Reading Electrocardiograms “Blind”
- Sudden Cardiac Death in Adult Patients with Stable Ischemic Heart Disease
- Ischemic Heart Disease in Women
- Stable Ischemic Heart Disease in the Older Adult
