Contemporary Management of Patients with Stable Ischemic Heart Disease
Radmila Lyubarova,MD ,Joshua Schulman-Marcus,MD and William E.Boden,MD
1 Division of Cardiology,Department of Medicine,Albany Medical Center,113 Holland Avenue,Albany,NY 12208,USA
2 VA New England Healthcare System,VA Boston-Jamaica Plain Campus,150 S.Huntington Avenue,Boston,MA 02130,USA
Abstract
Keywords: stable ischemic heart disease;coronary artery disease;optimal medical therapy
Introduction
The Coronary Artery Disease in General Practice (CADENCE)study used a cluster-stratif ed,crosssectional design to examine angina frequency in patients with stable angina attending Australian primary care practices [1].Among primary care practice patients with stable angina,29% (95% conf dence interval [CI] 26-31%)experienced one or more episodes of angina weekly,which was associated with greater physical limitations and worse quality of life,24 and 27% lower Seattle Angina Questionnaire scores,respectively (P < 0.05),compared with those with minimal angina (angina less than once a week in the preceding 4 weeks)[1].Patient characteristics associated with one or more episodes of angina weekly included female sex (odds ratio 1.42,P < 0.003),history of heart failure (odds ratio 1.59,P < 0.001),and peripheral artery disease (odds ratio 1.89,P < 0.001)[1].
Alexander et al.[2] conducted a survey of patients with coronary disease and angina pectoris at 6 months and 1 year after catheterization for selfreported symptoms and quality of life.At the 1-year follow-up (n= 1109),19% had chronic angina pectoris,11% had recurrent angina pectoris,and 70% were free of angina pectoris.Patients with chronic and recurrent angina pectoris had more single- vessel coronary artery disease (CAD),and under -went revascularization less often.Patients with chronic angina pectoris were younger,more likely to be women,had higher body mass index,had more depression and lung disease,and had more frequent baseline angina pectoris.In addition,patients in this group took more antianginals and other medications and had reduced physical function and healthrelated quality of life in relation to the persistence and frequency of symptoms (P < 0.001).
General Approach to Therapy
The overall goals of therapy for patients with stable ischemic heart disease (SIHD)are to minimize the likelihood of death while maximizing health and function.This includes reducing the likelihood of premature cardiovascular death,preventing complications of SIHD that directly or indirectly impair patients’functional well-being (including nonfatal myocardial infarction and heart failure),maintaining or restoring functional capacity and quality of life,reducing ischemic symptoms,minimizing costs of health care,and avoiding adverse effects of tests and treatments [3,4].
Risk Assessment
Multiple noninvasive modalities,including functional or anatomical testing,used to diagnose CAD also provide prognostic information about long-term risk.Functional assessment testing may be performed by standard exercise ECG,exercise stress testing with imaging (myocardial perfusion imaging or echocardiography),or pharmacologic stress testing with imaging when the patient is unable to exercise (myocardial perfusion imaging,echocardiography,or magnetic resonance imaging).Anatomical assessment is by coronary computed tomography angiogram or magnetic resonance angiography.Exercise capacity is very strong predictor of death and cardiac events,and it is prefer -able to perform exercise stress testing if the patient is able to achieve the maximal workload.Addition of imaging to exercise stress testing provides additional risk stratif cation markers,such as the extent of ischemia and left ventricular systolic function.If noninvasive testing suggests a low or intermediate CAD risk,then it is recommended to proceed with optimal medical therapy (OMT).If testing suggests a high risk of ischemia or if all adequate trials of OMT do not resolve anginal symptoms in patients with SIHD,then invasive coronary angiography with possible revascularization should be considered [3,4].
Risk Factor Modifi cation
Risk factor management is the foundation of guideline-directed medical therapy.As chronic stable angina is almost always related to underlying coronary atherosclerosis,attention should be paid to the presence of risk factors and/or lifestyle habits that facilitate the progression of CAD.Patients should be assessed for smoking status,hypertension,hyperlipidemia,diabetes,and overall dietary and activity status,as well as for hyperuricemia and psychosocial factors.If these are identif ed,lifestyle and/or pharmacologic interventions should be implemented to modify/reduce these modif -able risk factors and thereby reduce the progression of CAD,as well as prevent morbidity and death.However,some risk factors are not modif able,such as sex,age,and family history,and factor into the antianginal management plan [5].
All patients should be counseled about the need for lifestyle modif cation (class Ib),such as weight control,increased physical activity,alcohol consumption moderation,sodium intake reduction,increased consumption of fresh fruits and vegetables,and consumption of low-fat dairy products [3,4](Table 1).
It is crucial to implement OMT for risk factor modif cation.For lipid management,dietary therapy should be advised,with restriction of saturated fats to less than 7% of calories andtransfatty acids to less than 1% of calories [3].Starting moderate- or high-intensity statin therapy to achieve 50% or more LDL cholesterol level reduction from the baseline is recommended [3,8].Addition of nonstatin therapy with ezetimibe or a proprotein convertase subtilisin/kexin type 9 inhibitor to maximal tolerated statin therapy should be considered when additional LDL cholesterol level lowering is desired [9].Hypertension management should be according to the latest guidelines for achievement of a blood pressure goal of less than 130/80 mmHg with lifestyle modif cations and blood pressure-lowering medications,with the initial choice of a beta-blocker or renin-angiotensin-aldosterone inhibitors [6].The management of diabetes has shifted with the development of new classes of agents,and has recently been reviewed [10].
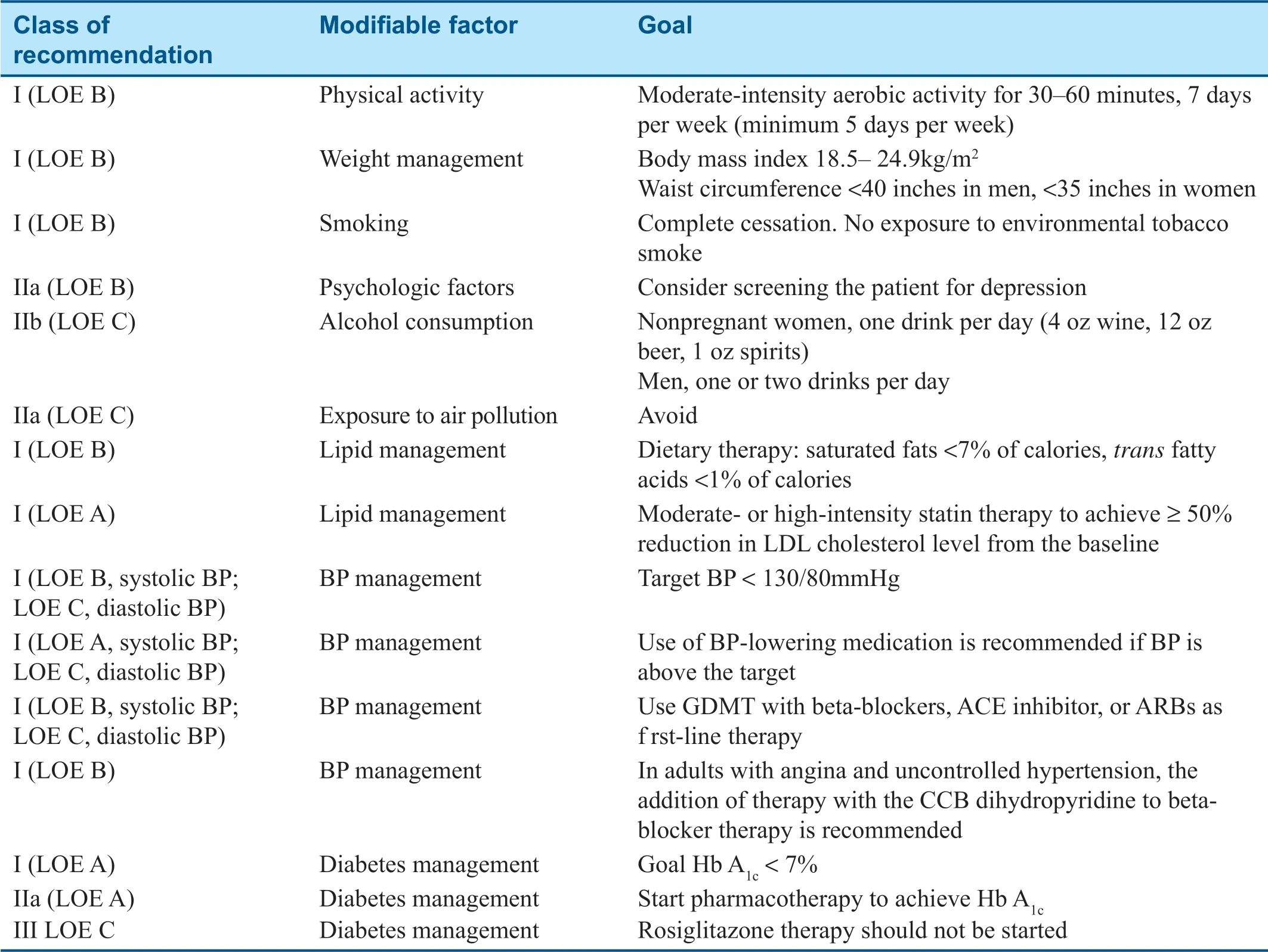
Table1 Optimal Medical Therapy for Stable Ischemic Heart Disease: Risk Factor Modif cation.
First-Line Pharmacologic Therapy
The use of f rst-line agents is focused on preventing myocardial infarction and death [3].Every patient with documented ischemic heart disease should be treated with an antiplatelet agent and aspirin and/or a thienopyridine when indicated [3].Beta-blockers should be used for patients with prior myocardial infarction or systolic heart failure [3].For patients with CAD and hypertension,diabetes,or left ventricular systolic dysfunction,renin-angiotensinaldosterone inhibitors are recommended [3].
Relief of Symptoms
Traditional Antianginal Therapy
It is recommended that adequate trials of medical therapy to control symptoms be undertaken before revascularization is considered to alleviate persistent symptoms.Commonly used antianginal agents include nitrates (isosorbide dinitrate,isosorbide mononitrate,nitroglycerin patch),beta-blockers (propranolol,metoprolol,atenolol,nadolol),calcium channel blockers (amlodipine,nifedipine,verapamil,diltiazem),and a late Na + current inhibitor (ranolazine)(Table 2).Nitrates improve myocardial oxygen supply and demand through their potent vasodilatory effect.Beta-blockers work primarily by decreasing myocardial oxygen consumption through reductions in heart rate,blood pressure,and myocardial contractility.Dihydropyridine (DHP)and non-DHP classes of calcium antagonists both increase blood fow,but non-DHP agents also decrease regulate heart rate (in contrast,some DHP agents increase heart rate).
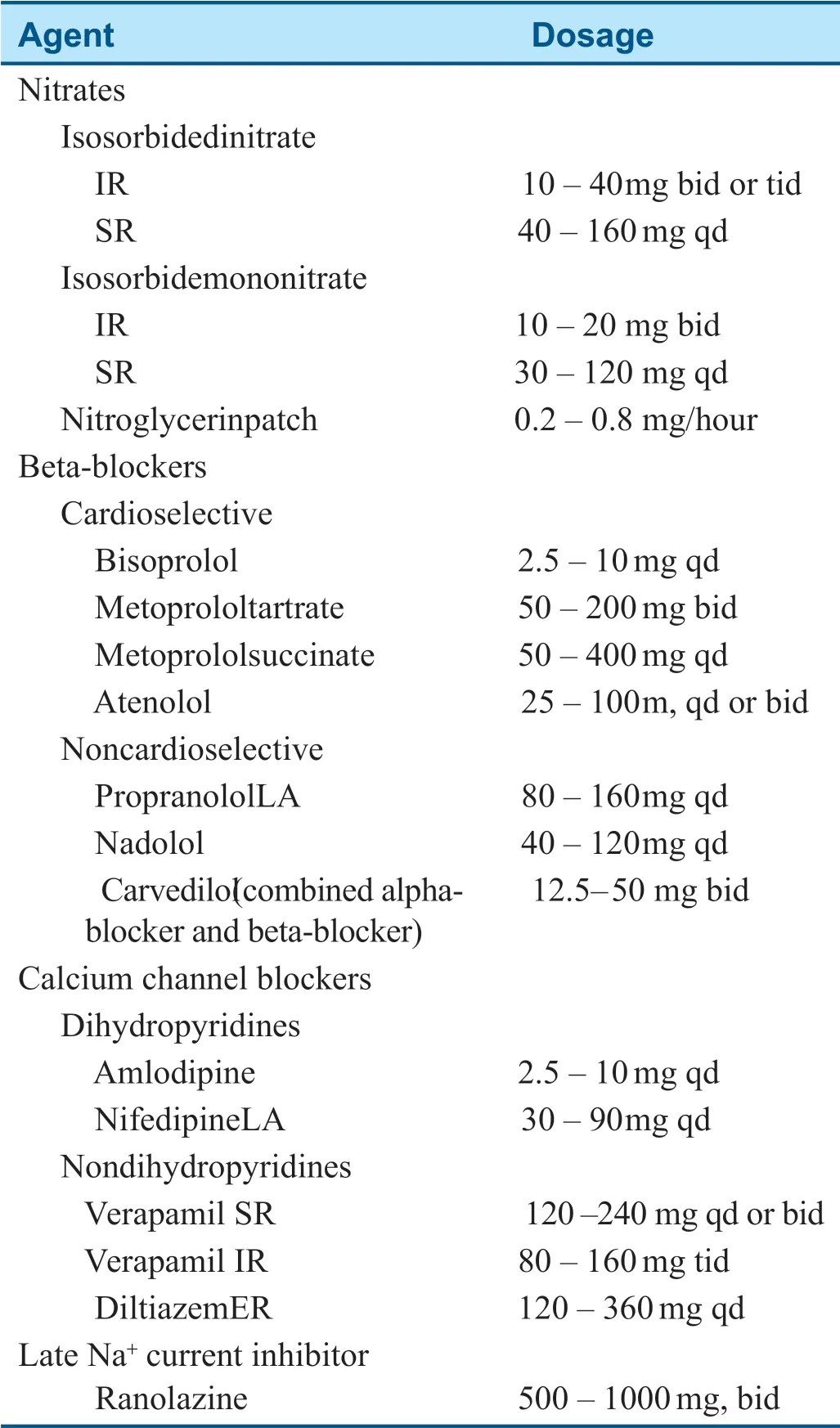
Table2 Antianginal Agents Approved for Treatment of Angina in the United States.
Many patients have relative intolerance to full doses of beta-blockers,calcium antagonists,and nitrates.Limitations to nitrate use include severe aortic stenosis,hypertrophic cardiomyopathy,and erectile dysfunction treated with phosphodiester -ase 5 inhibitors.Limiting factors for beta-blocker therapy include asthma,severe bradycardia,heart block,severe depression,Raynaud syndrome,and sick sinus syndrome.Limitations for use of calcium channel blockers include bradycardia and heart block,left ventricular dysfunction,and heart failure.
Heidenreich et al.[7] conducted a meta-analysis to determine the relative eff cacy and tolerability of treatment with beta-blockers,calcium channel blockers,and nitrates in patients with stable angina.Randomized or crossover studies compar -ing antianginal drugs from two or three dif ferent classes lasting at least 1 week were reviewed.The rates of cardiac death and myocardial infarction were not signif cantly different for treatment with beta-blockers versus calcium antagonists.There were fewer episodes of angina per week with betablockers than with calcium antagonists.Too few trials compared nitrates with calcium antagonists or beta-blockers to draw f rm conclusions about relative eff cacy.
Nitrate tolerance is a well-described phenomenon that occurs with long-term and continuous nitrate exposure.With each sequential dose,blood vessels become less responsive to the vasodilating ef fects of the nitrates.Tolerance develops primarily with the use of long-acting nitrates.The exact mechanism behind the development of nitrate tolerance is unclear.Current theories include increased generation of vascular superoxide anion,plasma volume expansion,impaired biotransformation of nitrates to nitric oxide,decreased end-oxygen responsiveness to nitric oxide,and neurohormonal activation.Nitrate tolerance is readily reversed by provision of a 10- to 12-hour nitrate-free period each day.This can be achieved by administration of nitrates three times per day.Cross tolerance exists and could be clinically important,as noted in a study that demonstrated long-term continuous exposure to orally administered sustained-release isosorbide dinitrate led to abolition of anti-ischemic ef fects,with simultaneous loss of ef fects of sublingually administered nitroglycerin [11].
Consequently,many patients continue to experience ischemic symptoms with traditional antiischemic medication,even when taking two or three antianginal agents [7].Furthermore,traditional antianginal agents have not been shown to reduce the risk of cardiovascular death or myocardial infarction in chronic stable angina.Antianginal agents with new/novel mechanisms of action have thus been a focus of study for some time.
Ranolazine
Ranolazine,a late sodium inf ux inhibitor,in contrast to older antianginal medications,appears to work downstream of the ischemic insult,complementing the mechanism of action of traditional medications.Ranolazine has been studied in lar gescale clinical trials involving patients with chronic stable angina (monotherapy in MARISA,combination therapy in CARISA and ERICA)and patients with non-ST-elevation acute coronary syndrome (MERLIN-TIMI 36)[12-15].Ranolazine was associated with signif cant alleviation of angina,had no signif cant ef fect on heart rate or blood pressure,and was well tolerated.Ranolazine has important drug interactions with strong cytochrome P450 3A4 inhibitors (e.g.,ketoconazole,itraconazole,clarithromycin).A dosage limit of 500 mg twice daily is recommended for patients using concomitant moderate cytochrome P450 3A4 inhibitors (diltiazem,verapamil,erythromycin,f uconazole).With P-glycoprotein inhibitors (cyclosporine),a dose reduction of ranolazine may be required.For drugs transported by P-glycoproteins or metabolized by cytochrome P450 2D6 (digoxin),a reduced dose may be required when they are used in combination with ranolazine.
Ling et al.[16] evaluated the eff cacy of ranolazine in patients with chronic angina pectoris and assessed the impact of ranolazine on health care resource use.Of the 150 patients included in this analysis,most had under gone percutaneous coronary intervention (PCI)and coronary artery bypass grafting (CABG).Long-acting nitrates,betablockers,and calcium antagonists were being used in 83,97,and 75% of patients,respectively [16].With regard to Canadian Cardiovascular Society angina class,at the baseline,8% of patients had class 2 angina,58% had class 3 angina,and 34% had class 4 angina.At the end of ranolazine therapy,the proportions were 18% for class 2 angina,62% for class 3 angina,and 28% for class 4 angina.During the period before ranolazine therapy,the numbers of clinic visits,emer gency department visits,and hospital visits were 428,59,and 137,respectively.During the period after ranolazine therapy,the number of visits decreased to 419,42,and 96,respectively.These data demonstrate that ranolazine reduced the Canadian Cardiovascular Society angina class and reduced health care resource use over a 12-month follow-up period in a diff cult-to-treat group of patients with severe angina pectoris [16].
Alternative Therapies for Angina
Alternative therapies for refractory angina may be considered when traditional antianginal therapy is not ef fective and the patient is not amenable to revascularization,such as spinal cord stimulation,transmyocardial revascularization,and enhanced external counterpulsation,all class IIb recommendations [3].Ongoing studies are investigating other devices in severe refractory angina,such as the coronary sinus reducer [17-19].
Metabolic Modulation: Trimetazidine
The free fatty acid oxidation hypothesis arose out of advances in understanding of myocardial metabolic pathways.Myocardial cells derive their ener gy via fatty acid and glucose metabolism.During ischemia the fatty acid pathway predominates.However,this pathway requires more oxygen than the glucose pathway [20-3].Theoretically,inhibition of fatty acid oxidation should promote a shift toward the more oxygen-eff cient glucose pathway.A number of groups have reported experimental data showing that the antianginal trimetazidine is an inhibitor of partial fatty acid oxidation.However,other investigators have not observed any inhibition with trimetazidine in other experimental models [20-2].Thus inhibition of fatty acid oxidation as a major antianginal mechanism for trimetazidine remains to be def nitively established [20-3].Chazov et al.[24] conducted a randomized,placebo-controlled trial to assess the eff cacy and acceptability of trimetazidine in combination with hemodynamic agents (beta-blockers or long-acting nitrates)in 177 stable angina patients.Patients with stable angina resistant to nitrates or beta-blockers,who had a difference of 10% in the duration between two positive exercise test results,were randomly treated with trimetazidine (n= 9 0)or placebo (n= 8 7)for 12 weeks.Patients in the trimetazidine arm had signif cantly fewer anginal episodes per week compared with patients in the placebo arm (2.1 versus 5.1 angina episodes per week,P < 0.05).There was also a trend for less nitrate use among patients in the trimetazidine arm.Patients in the trimetazidine arm had signif cantly longer duration of exercise at trough compared with patients in the placebo arm (506.8 s vs.458.9 s,P < 0.05).
Sinus Node Inhibitor: Ivabradine
Ivabradine is a selective sinus node Ifinhibitor that causes heart rate reduction and decreases myocardial demand.Borer et al.[25] conducted a double-blind,placebo-controlled trial to evaluate the antianginal and anti-ischemic effects of ivabradine in 257 patients with a history of chronic stable angina of 3 months or longer.The time to 1-mm ST-segment depression and limiting angina was signif cantly increased in the ivabradine groups [25].Tardif et al.[26] evaluated the antianginal and anti-ischemic eff cacy of ivabradine in patients with chronic stable angina pectoris receiving betablocker therapy in the ASSOCIATE study.This study demonstrated that the combination of ivabradine (7.5 mg twice daily)and atenolol in patients with chronic stable angina pectoris produced additional eff cacy with no untoward effect on safety or tolerability [20].
Koester et al.[27] conducted a subgroup analysis of 351 octogenarians from the REDUCTION study to assess the antianginal effects of ivabradine as initial or extended medical therapy for angina pectoris.After 4 months,ivabradine therapy signif cantly reduced from the baseline the number of angina attacks,heart rate,and nitrate consumption.The regimen was well tolerated,and physicians reported that the eff cacy of ivabradine was very good.However,the antianginal ef fect of ivabradine did not translate into improvement in cardiac outcomes in the BEAUTIFUL and SIGNIFY trials [28,29].
Preconditioning Agent: Nicorandil
Nicorandil possesses a nitrate moiety,and therefore produces hemodynamic ef fects similar to those of long-acting nitrates.It activates cyclic GMP,dilates capacitance vessels,and decreases preload [23].Nicorandil is also capable of opening ATP-sensitive potassium channels.These channels are involved in dilation of coronary resistance arterioles,which decreases afterload,and are also thought to mimic ischemic preconditioning,a potential cardioprotective effect [23].
Meany et al.[30] conducted a double-blind par -allel group study in 46 patients with chronic stable angina to assess the eff cacy of nicorandil with regard to exercise capacity.Patients were randomized to receive nicorandil at a dosage of 5 mg twice daily (n= 5),nicorandil at a dosage of 10 mg twice daily (n= 10),or placebo.The nicorandil dosages were increased to 10 and 20 mg twice daily,respectively,after 1 week of treatment.A symptomlimited Bruce protocol exercise test was performed before and 2 hours after the initial dose and after 2 weeks of treatment,2 and 12 hours after administration.After initial dosing (day 1),there were signif cant increases in exercise duration and the time to onset of angina in patients receiving nicorandil.After 2 weeks,there was a signif cant increase in the time to onset of angina in both nicorandil groups compared with the placebo group (P < 0.05).The time to 1-mm ST-segment depression,exercise duration,and total workload increased in the nicorandil groups,but the dif ference from the placebo group did not reach statistical signif cance.
The IONA study was a double-blind,randomized study to evaluate whether nicorandil could reduce the frequency of coronary events in men and women with stable angina and additional risk factors (n= 5126 patients)[31].The primary composite end point was coronary heart disease death,nonfatal myocardial infarction,and unplanned hospital admission for cardiac chest pain.Over the mean follow-up of 1.6 years,398 primary end point events (15.5%)were noted in the placebo group compared with 337 (13.1%)in the nicorandil group (hazard ratio 0.83,95% CI 0.72-0.97,P = 0.014)[31].The rate of acute coronary syndromes was 7.6% (n= 195)in the placebo group and 6.1% (n= 156)in the nicorandil group (hazard ratio 0.79,95% CI 0.64-0.98,P = 0.028),and the corresponding rates for all cardiovascular events were 17.0% (n= 436)and 14.7% (n= 378)(hazard ratio 0.86,95% CI 0.75-0.98,P = 0.027).These data show that nicorandil can produce signif cant improvement in outcomes because of a reduction in the rate of major coronary events in patients with stable angina.
Referral for Revascularization
To date,no study has clearly demonstrated that revascularization of stable CAD patients with PCI reduces the risk of death or myocardial infarction,although a lar ge randomized study (ISCHEMIA)will soon clarify this matter further.The ideal use of revascularization to reduce anginal symptoms remains an area of active investigation.In general,revascularization with PCI or CABG should be reserved for patients who have inadequate symptom control with at least two antianginal medications.
Recent studies provide some additional considerations when one is weighing the benef ts of PCI versus medical therapy for symptom control.
Data from the COURAGE trial showed that both treatment groups (PCI added to OMT and medical therapy alone)had a substantial reduction in the prevalence of angina during follow-up but the effect attenuated over time [32].The only signif cant difference between the two treatment strategies was a reduced prevalence of angina in the PCI group at 1 and 3 years;however,by 5 years there was no signif cant difference between the groups in freedom from angina.Most of the increase in freedom from angina in the medical therapy group was present at 1 year,with a further improvement at 5 years.
In the BARI 2D study,2368 patients with diabetes mellitus and stable CAD were randomized to receive either medical therapy or coronary revascularization (either surgical or catheter based)[33].At follow-up at 5 years,the rate of death did not differ signif cantly between the medical therapy group and revascularization group.However,the composite end point of death,myocardial infarction,and stroke was signif cantly lower in the CABG stratum in the revascularization group (P = 0.01).The FAME-2 trial randomized patients with stable coronary disease to receive medical therapy or fractional fowreserve-guided PCI [34,35].While the composite primary end point (all-cause death,nonfatal myocardial infarction,and unplanned hospitalization leading to ur gent revascularization)was lower in the PCI group,the rates of death and myocardial infarction were not dif ferent between the groups.ORBITA was the f rst placebo-controlled trial that randomized patients (n= 200)with refractory angina to receive medical therapy and either true or sham PCI [36].There was no signif cant difference in the change in exercise time or angina with PCI.There was improvement in the wall motion score index on stress echocardiography in the PCI group compared with the placebo group.ORBIT A raises questions on how much of PCI angina relief is driven by placebo factors.
When one is deciding on a revascularization strategy with PCI or CABG,several factors should be taken into account,such as the location,extent and complexity of the lesion(s),the presence of left ventricular dysfunction,diabetes mellitus,tar get vessels,age,and comorbidities.In the SYNT AX trial,comparing CABG versus PCI among patients with three-vessel disease,CABG reduced the risk of death,myocardial infarction,and repeated revascularization,especially among those with higher SYNTAX scores [37-39].No difference in mortality was observed in those with SYNT AX scores below 22.Among patients with diabetes and multivessel coronary disease in the FREEDOM trial,CABG had a much lower primary event rate (death,myocardial infarction,or stroke)compared with PCI [40].This trial suggests a beneft from revascularization with CABG for patients with diabetes and advanced CAD.
Summary
Angina persists for many patients despite medical therapy and/or revascularization.In all patients with angina,aggressive risk factor modif cation and optimized medical management must be instituted.Revascularization should be performed for highrisk patients or patients with persistent symptoms.A beta-blocker is likely a frst-line agent;however,most patients require multiple medications for symptom control.Novel agents with new mechanisms improve treatment options,including ivabradine (sinus node inhibitor),and late Na+blockade (with a mechanism of action complementary to traditional agents)is benef cial in a broad range of patients unresponsive to current treatment options.Ongoing trials may help better def ne the role of aggressive medical therapy with or without revascularization.
Funding
This work received no specif c grant from any funding agency in the public,commercial,or not-for -prof t sectors.
Conflict of Interest
The authors declare no conf ict of interest.
 Cardiovascular Innovations and Applications2019年1期
Cardiovascular Innovations and Applications2019年1期
- Cardiovascular Innovations and Applications的其它文章
- Left Ventricular Dysfunction in Ischemic Heart Disease
- Diabetes Mellitus and Stable Ischemic Heart Disease
- Reading Electrocardiograms “Blind”
- Sudden Cardiac Death in Adult Patients with Stable Ischemic Heart Disease
- Ischemic Heart Disease in Women
- Stable Ischemic Heart Disease in the Older Adult
