Low platelet count: Predictor of death and graft loss after liver transplantation
Pedro Beltrame, Santiago Rodriguez, Ajacio Bandeira de Mello Brandão
Abstract BACKGROUND The impact of platelets on liver transplantation (LT) is well recognized, but not completely understood. Platelets exert dichotomous effects on the graft and on the patient. On the one hand, they are essential for primary hemostasis and tissue repair and regeneration. On the other hand, they support ischemia/reperfusion injury and inflammatory processes. Recent evidence has shown a new role for platelet count (PC) in predicting outcomes after LT.AIM To evaluate if low PC is a predictor of short- and long-term outcomes after LT.METHODS Four hundred and eighty consecutive LT patients were retrospectively assessed.PC from the preoperative to the seventh postoperative day (POD) were considered. C-statistic analysis defined the ideal cutoff point for PC. Cox regression was performed to check whether low PC was a predictor of death,retransplantation or primary changes in graft function within one year after LT.RESULTS The highest median PC was 86 × 109/L [interquartile range (IQR) = 65-100 ×109/L] on seventh POD, and the lowest was 51 × 109/L (IQR = 38-71 × 109/L) on third POD. The C-statistic defined a PC < 70 × 109/L on fifth POD as the ideal cutoff point for predicting death and retransplantation. In the multivariate analysis, platelets < 70 × 109/L on 5POD was an independent risk factor for death at 12 mo after LT [hazard ratio (HR) = 2.01; 95% confidence interval (CI) 1.06-3.79;P = 0.031]. In the Cox regression, patients with PC < 70 × 109/L on 5POD had worse graft survival rates up to one year after LT (HR = 2.76; 95%CI 1.52-4.99; P =0.001).CONCLUSION PC < 70 × 109/L on 5POD is an independent predictor of death in the first year after LT. These results are in agreement with other studies that indicate that low PC after LT is associated with negative outcomes.
Key words: Predictive factors; Prognosis; Platelet count; Liver transplantation; Graft survival; Mortality
INTRODUCTION
Low platelet count (PC) is common in candidates for liver transplantation (LT). Its etiology is multifactorial, including increased spleen destruction, inability to produce bone marrow and reduced production of thrombopoietin[1-3]. Reduction in PC is also commonly observed in the postoperative period of LT. In this period, there are other possible contributing factors for its occurrence, such as graft and splenic sequestration, hemodilution, use of some medications and immunological reactions[4-8]. After LT, PC reach their lowest level around the third or fifth postoperative day (POD), returning to preoperative values in around two weeks[9].Low PC after LT is associated with shorter graft and patient survival and higher rates of negative outcomes[10], possibly due to the fact that platelets play an important role in the promotion of angiogenesis[11-14]and hepatic regeneration[15,16].
Lesurtel et al[17]observed that a PC < 60 × 109/L on the fifth POD was an independent risk factor for complications and shorter graft and patient survival within the first 90 d posttransplantation. They then proposed the “60-5 criterion”,where a PC of < 60 × 109/L on 5POD of LT could be used to predict severe complications[17]. Subsequently, Takahashi et al[18]reported that a PC of < 72 × 109/L on 5POD was associated with graft loss and shorter patient survival. The present study aimed to confirm the hypothesis that a low PC in the immediate postoperative period of LT is a predictor of death or retransplantation.
MATERIALS AND METHODS
All adult patients consecutively submitted to LT with a deceased donor between June 2006 and June 2016 were eligible at a referral center in southern Brazil. Excluded from the study were patients who underwent double organ transplantation (liver and kidney), late liver retransplantation (more than one year between LT and retransplantation) or LT due to acute liver failure and who had incomplete medical records. The study followed the recommended guidelines for observational studies[19]and was approved by the Institutional Review Board of Santa Casa de Misericórdia de Porto Alegre (No. 1.183.375).
Variables analyzed
The following variables were analyzed: (1) Demographic characteristics of the recipient and donor (sex, age and body mass index); (2) variables related to the procedure (times of cold and warm ischemia, volume of bleeding and transfusions during transplantation); (3) blood components transfused up to the first week after LT; (4) biochemical tests performed immediately before LT and up to the seventh POD: PC, international normalized ratio (INR), aspartate aminotransferase, alanine aminotransferase (ALT), total bilirubin, factor V, alkaline phosphatase and gamma-GT; and (5) relevant preoperative characteristics of the recipient: Need for ventilation or hemodynamic support, renal replacement therapy, hepatorenal syndrome,cirrhosis etiology, model for end-stage liver disease (MELD) score, and Child-Turcotte-Pugh (CTP) score[20-22].
Surgical procedure
All patients underwent LT by the same team, where the technique of choice was hepatectomy with preservation of the inferior vena cava (piggy-back technique). The preservation solutions used during the period were: First, the University of Wisconsin solution, then histidine-tryptophan-ketoglutarate and, since 2013, the Institute Georges Lopez-1 solution. The decision to transfuse blood components was based on clinical, laboratory and hemodynamic parameters. Blood loss was restored by transfusion of packed red blood cells, with the goal of maintaining hemoglobin levels between 8.0 and 10.0 g/dL. Platelet concentrate was administered only in patients with platelet dysfunction and persistent bleeding, even after correction of other coagulation factors.
Outcomes
The primary outcome was death, by any cause, within 30, 90 and 365 d after LT. The secondary outcome was the need for liver retransplantation in the same period. We considered any cause of death and retransplantation after LT, which could be primary or secondary. Secondary death/retransplantation was due to technical,immunological, infectious or cardiovascular causes. Primary death/retransplantation was due to delayed graft function or primary graft dysfunction. Delayed graft function was defined as the presence of at least 1 of the following parameters 7 d after LT: A serum bilirubin level ≥ 10 mg/dL and an INR ≥ 1.6 or an ALT level > 2000 IU/L[17]. Primary graft dysfunction was defined as the presence of one or more of the following postoperative laboratory parameters: A serum bilirubin level ≥ 10mg/dL on day 7, INR ≥ 1.6 on day 7, and an ALT level > 2000 IU/L within the first 7 d[23].
Statistical analysis
Statistical analysis was performed with IBM SPSS software version 22.0 for Windows(IBM, Armonk, NY, United States). Quantitative variables were described by mean and SD, and significance was determined by Student t-test. Categorical variables were described by counts and percentages, and significance was assessed using the chisquare test or Fisher exact, when needed. The C-statistic, equivalent to the area under the receiver operating characteristics (ROC) curve (AUC) assessed on each POD of LT,was adopted to establish the day on which the PC showed the best performance.Recursive analyses of ROC curves, within the day previously detected, allowed us to identify the cutoff point. Univariate and multivariate Cox regression analyses were performed to adjust the PC findings with the potential effect of other factors. The preoperative variables chosen, with potential confounding effect over PC in the postoperative period, as previously shown in similar studies[17,18,23], were: MELD score before LT > 20, pre-LT PC < 70 × 109/L, age of the recipient > 60 yr, donor age > 40 yr and diagnosis of hepatorenal syndrome at the time of transplantation. In addition, the need for intraoperative transfusion of platelet concentrates, perioperative bleeding >2500 mL and cold ischemia time > 8 h were considered. Survival curves were obtained using the Kaplan-Meier method. P < 0.05 was considered statistically significant.
RESULTS
Population studied
Of the 617 eligible patients for study, 137 (22.2%) were excluded from the analysis for the following reasons: Underwent combined liver and kidney transplantation (n = 32;5.2%); late liver retransplantation (performed one year after the initial LT) (n = 21;3.4%); transplantation for acute liver failure (n = 21; 3.4%); or incomplete information in medical records up to seventh POD, due to either death, retransplantation or inadequate completion of medical records (n = 63; 10.2%). Therefore, 480 patients were included in the study. Approximately 20% of them were older than 60 yr, with the majority being male, and hepatitis C virus infection was the most frequent etiology of cirrhosis. At the time of LT, the mean MELD score was 16; approximately 49% of patients were in the B classification of the CTP score and 3.5% underwent hemodialysis immediately before transplantation. About 48% of the donors were older than 40, and most times the cold ischemia time was < 8 h (Table 1).
Characteristics of patients in relation to platelet count
The highest median number of PC was observed on seventh POD: 86 × 109/L[interquartile range (IQR) = 65-100 × 109/L], exceeding the preoperative median, i.e.,77 × 109/L (IQR = 57-97 × 109/L). The lowest median was found on the third POD: 51× 109/L (IQR = 38-71 × 109/L).
C-statistical analysis showed that a PC < 70 × 109/L on 5POD was the ideal cutoff point for predicting death and retransplantation at 365 d after LT [AUC-ROC = 0.632;95% confidence interval (CI) 0.558-0.705; P = 0.001]. Patients were then stratified into two groups according to PC on 5POD: Patients with ≥ 70 × 109/L platelets and those with < 70 × 109/L platelets (Table 1). In the group with < 70 × 109/L PC, the recipients were transplanted at later stages of their disease according to the CTP score (P =0.014) and, although without statistical significance, they received organs with a longer time of cold ischemia and from donors over 40 yr old (Table 1).
Outcomes and platelet counts on 5POD
Univariate analysis (Table 2) showed that patients with a PC of < 70 × 109/L on 5POD had higher all-cause mortality rates at 90 and 365 d after LT, compared to patients with a higher PC. The 90-day mortality rate was 7.5%, higher in patients with a PC <70 × 109/L on 5POD (9.7% vs 4.2%, P = 0.037). Overall mortality at 365 d post-LT was 13.3%. Likewise, the highest mortality rates occurred in the group with PC < 70 ×109/L on 5POD (17.4% vs 7.3%; P = 0.002). Retransplantation rates at 30, 90 and 365 d were higher in patients with lower PC (< 70 × 109/L) on 5POD. In fact, the need for retransplantation up to 90 d after LT was only observed in the group of patients with a lower PC, and only one patient with a PC of ≥ 70 × 109/L on 5POD required retransplantation within 365 d post-LT (5.2% vs 0.5%; P = 0.004) (Table 2).
Multivariate analysis
Multivariate analysis (Figure 1) showed that, in the first year after LT, a PC < 70 ×109/L on 5POD was a risk factor for death, independently of age of the recipient > 60 yr, pre-LT MELD score > 20, bleeding volume > 2500 mL intraoperatively and need for transfusion of platelet concentrates during the procedure. Pre-LT MELD > 20 and age of the recipient > 60 yr also appeared to be independent risk factors for mortality up to one year after LT (P = 0.031 and P = 0.012, respectively).
Survival of grafts and recipients
Eighty grafts were lost in up to one year of follow-up: 64 (80.0%) due to death of the recipient and 16 (20.0%) due to the need for liver retransplantation. Of the patients who underwent liver retransplantation, six were due to primary causes: three for primary graft nonfunction (18.75%), two for primary graft dysfunction (12.5%) and one for delayed graft function (6.25%). The most common causes of death were infection (28.1%), cardiovascular events (21.8%) and primary causes related to the graft (7.8%). Graft survival in the first year after LT was significantly lower in the group with PC < 70 × 109/L on 5POD compared to ≥ 70 × 109/L on 5POD group, even when adjusted for the factors used in multivariate analysis (77.5% vs 92.2%, P = 0.001)(Figure 2). Overall survival at 12 mo for patients with a PC ≥ 70 × 109/L on 5POD was higher than for those with a lower PC (92.8% vs 82.7%, P = 0.002) (Figure 3).
DISCUSSION
This study showed that PC < 70 × 109/L on 5POD of LT were independently associated with shorter patient and graft survival within one year after LT. These results are in agreement with other studies indicating that thrombocytopenia in the immediate postoperative period of LT is associated with negative outcomes[17,18,23].
Platelets contain a marked number of secretory granules, filled with proteins essential for hemostasis and different tissue growth factors, such as platelet-derived growth factor (PDGF), hepatocyte growth factor (HGF), insulin-like growth factor type 1 (IGF-1), vascular endothelial growth factor (VEGF), serotonin, ADP and ATP[14].Platelets are activated by various types of stimuli and release these substances depending on the situation. In addition to its known role in primary hemostasis and thrombosis, platelets exert other functions, such as promoting liver regeneration andliver protection[10-14]. In liver recipients, it is common to have thrombocytopenia[1,24], a situation that worsens during transplantation, for reasons not completely understood[10]. However, many factors have been identified and associated with thrombocytopenia, such as their consumption in the process of hemostasis and sequestration by reperfusion graft or spleen[4,10,25,26].
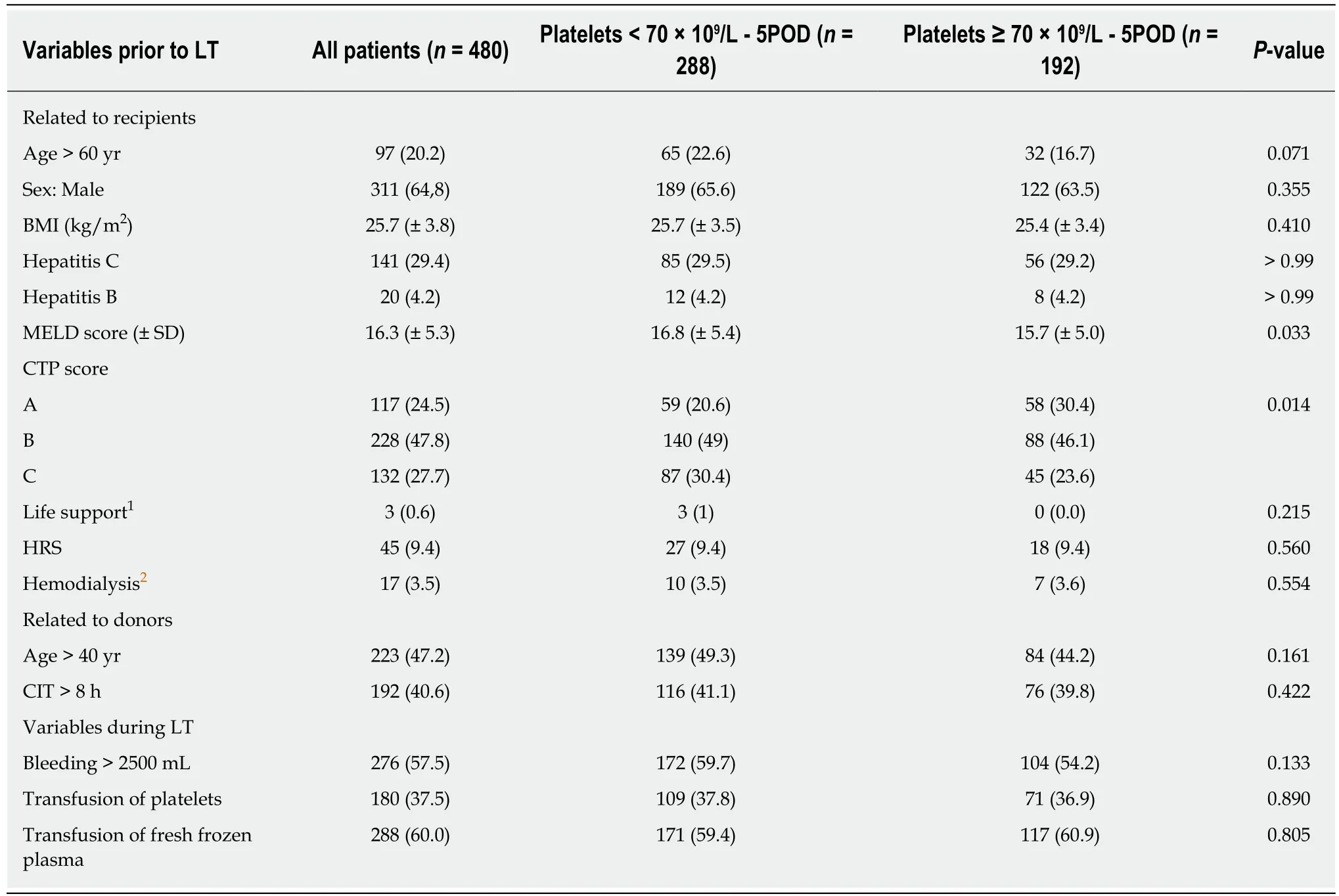
Table 1 Comparison of patients according to platelet count on fifth postoperative day of liver transplantation, n (%)
The relationship between low PC and events after LT was suggested in the late 1990s, when thrombocytopenia (defined arbitrarily) in the immediate postoperative period of LT was associated with shorter patient and graft survival[10,25,27,28]. However,it was the Lesurtel et al[17]who established a cutoff point in the number of platelets that could be used as a predictor of outcomes after LT. In a retrospective study, Lesurtel et al[17]evaluated a cohort of 257 patients who underwent LT with a deceased donor.They observed that a PC < 60 × 109/L on 5POD was an independent predictor of Clavien-Dindo IIIb/V complications (OR = 1.96; 95%CI 1.07-3.56), graft loss [hazard ratio (HR) = 2.0; 95%CI 1.1-3.6], and lower survival of patients (HR = 2.2; 95%CI 1.4-4.6, P = 0.03) within 90 d after LT. They then proposed the “60-5” criterion, in which the determination of the number of platelets on 5POD could be used to predict outcomes, anticipate complications, and thus be used prophylactically. Later,Takahashi et al[18], also retrospectively analyzing a cohort of transplanted patients with a deceased donor, reported that a PC < 72 × 109/L on 5POD was associated with graft loss and shorter patient survival within one year after LT. The authors postulated that in patients with a greater number of platelets, more thrombocytes accumulate in the graft, which would allow the release of a greater amount of growth factors (PDGF,HGF, IGF-1 and VEGF), improving graft survival and survival in general[18]. In studying 234 adult patients submitted to LT with living donors, a Chinese study[23]concluded that a PC of ≤ 68 × 109/L at any time in the immediate postoperative period was an independent risk factor for early graft dysfunction (OR = 2.88; 95%CI 1.22-6.82, P = 0.016).
The present study validated the “60-5 criterion”, where we found that a PC < 70 ×109/L on 5 POD was independently associated with mortality at 365 d after LT.Overall survival of patients with < 70 × 109/L on 5POD was 2.5-fold lower than forpatients with a PC ≥ 70 × 109/L on 5POD. In addition, lower liver graft survival was observed in the first year after surgery: patients with PC < 70 × 109/L on 5POD had a 2.76-fold greater risk of graft loss than patients with a higher PC. Therefore, our results are in line with the “60-5 criterion”, although the cutoff point was different. In fact, another study[29]validating the “60-5 criterion” also identified a cutoff point different from the one originally proposed. At the time of transplantation, patients with a lower PC on 5POD had a more severe disease: The mean MELD was higher(16.8 ± 5.4 vs 15.7 ± 5.0; P = 0.033), and most of them were in the C category of the CTP score (30.4% vs 23.6%, P = 0.014), which could predict the onset of intra- and postoperative complications. However, the intraoperative variables analyzed, such as the requirement for transfusion of blood components (including platelets), were similar in the two groups, and it is unlikely that the severity of the disease at the time of LT showed any clinical significance. Another issue to be pondered is how a decreased PC on 5POD can have an influence on late outcomes. Considering that patients with a reduced number of platelets on 5POD have a higher rate of biliary tract complications[29], and that these are associated with infectious complications,hospital readmissions and endoscopic or surgical interventions, it is possible that such complications may have an impact on the survival of grafts and patients in the long run[18,29].
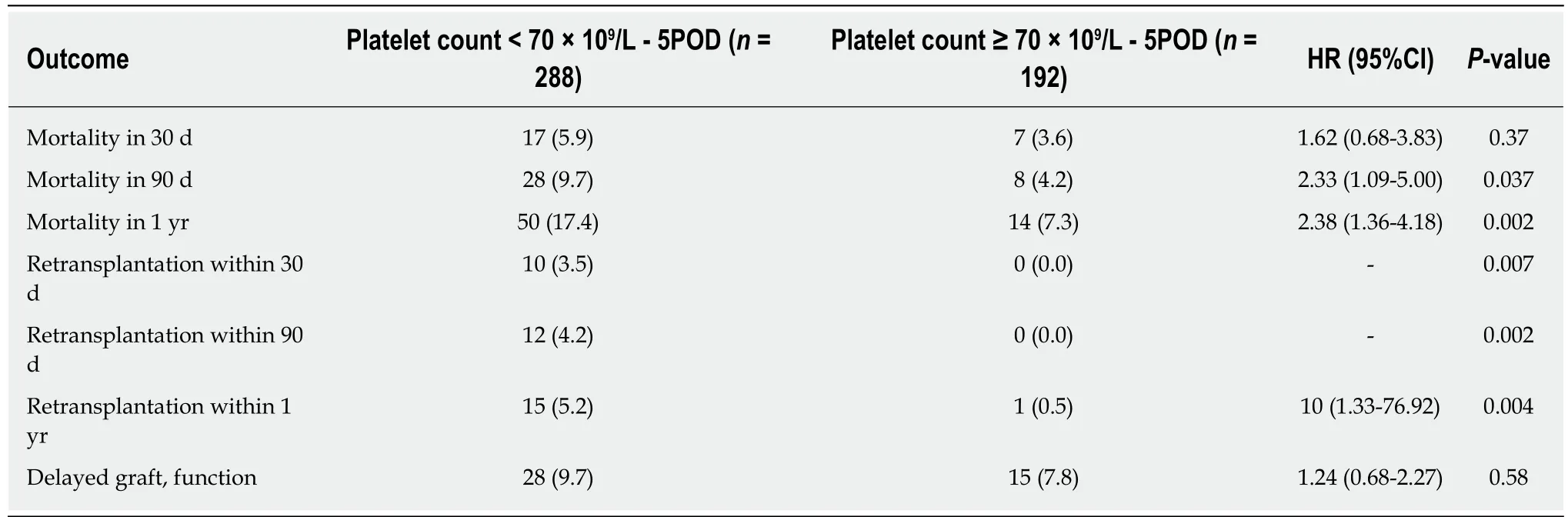
Table 2 Univariate analyses of postoperative outcomes according to patients’ platelet count after liver transplantation, n (%)
Theoretically, for patients with post-transplant thrombocytopenia, preventive measures should be taken to avoid or minimize adverse effects: Platelet transfusion,suspension of potentially myelosuppressive drugs, or administration of serotonin or thrombopoietin. However, further studies are needed before these interventions are considered in clinical practice, although transfusion of platelets in transplant recipients seems to be positively associated with graft regeneration[30,31]. In addition,this study pointed out that a pre-LT MELD > 20 and age of the recipient > 60 yr was also independent risk factors for mortality up to one year after LT.
This study had some limitations. One of them is inherent to retrospective studies;this study was carried out in a single center. However, the same team of surgeons and anesthesiologists performed the procedures, and in the immediate postoperative period, patients were treated in an intensive care unit exclusively for patients undergoing organ transplantation. The study design also did not allow us to demonstrate that platelet transfusion could effectively exert a protective effect for the graft and patient. In addition, with this study, it was not possible to clarify, in fact, if low PC in the postoperative period is the cause of negative outcomes after LT or if it is a surrogate marker of another clinical condition, which could be the real problem.
In summary, patients with PC of < 70 × 109/L on 5POD of LT showed higher mortality within 365 d after transplantation and lower graft survival. This study reinforces the need to evaluate the role of interventions to maintain a minimum PC after LT to potentially improve outcomes after LT.
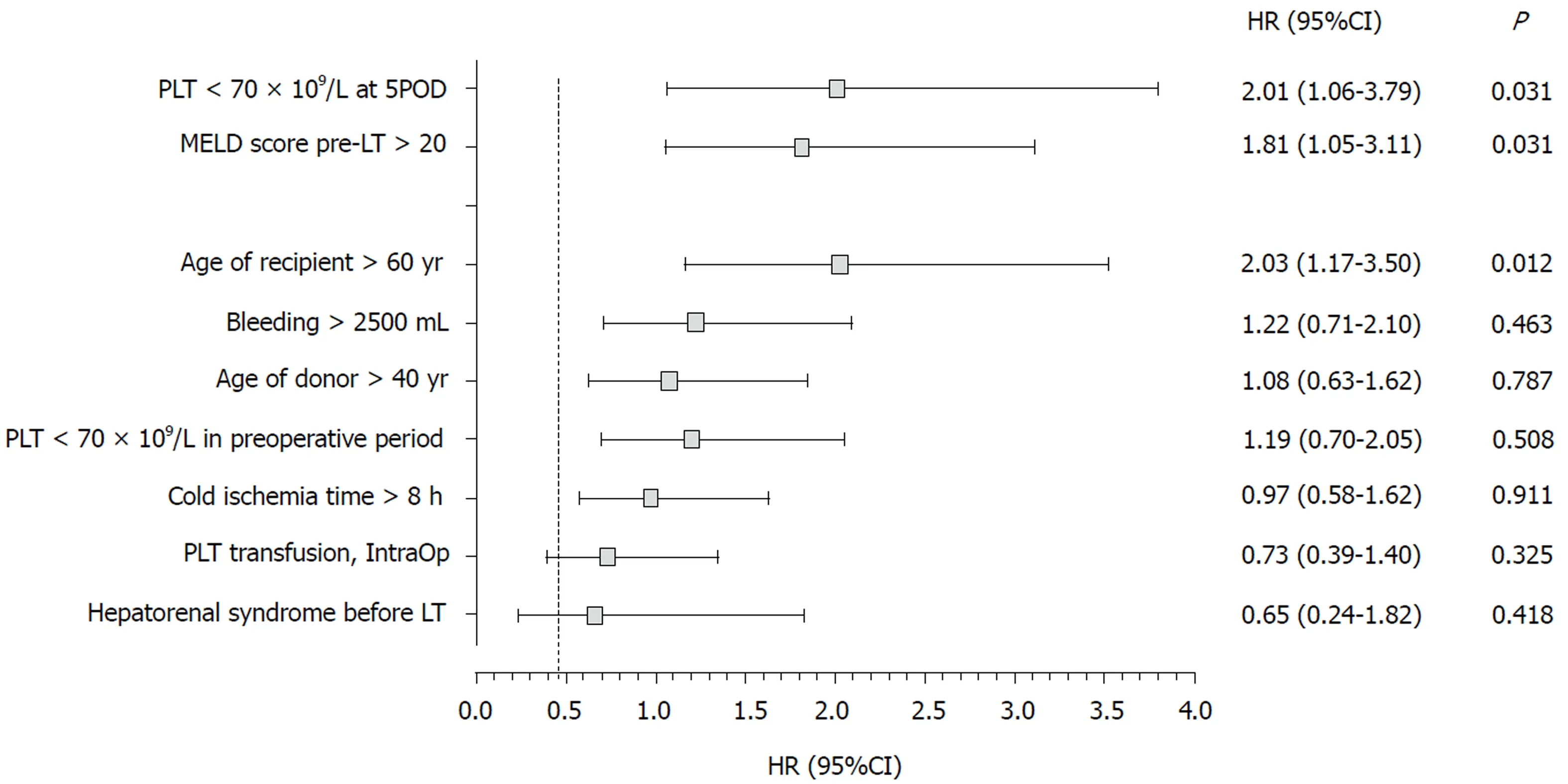
Figure 1 lndependent risk factors of death within one year after liver transplantation, in multivariate analysis. 5POD: Fifth postoperative day; 95%CI: 95%confidence interval; HR: hazard ratio; IntraOp: Intraoperative; PLT: Platelets; MELD: Model for end-stage liver disease; LT: Liver transplantation.
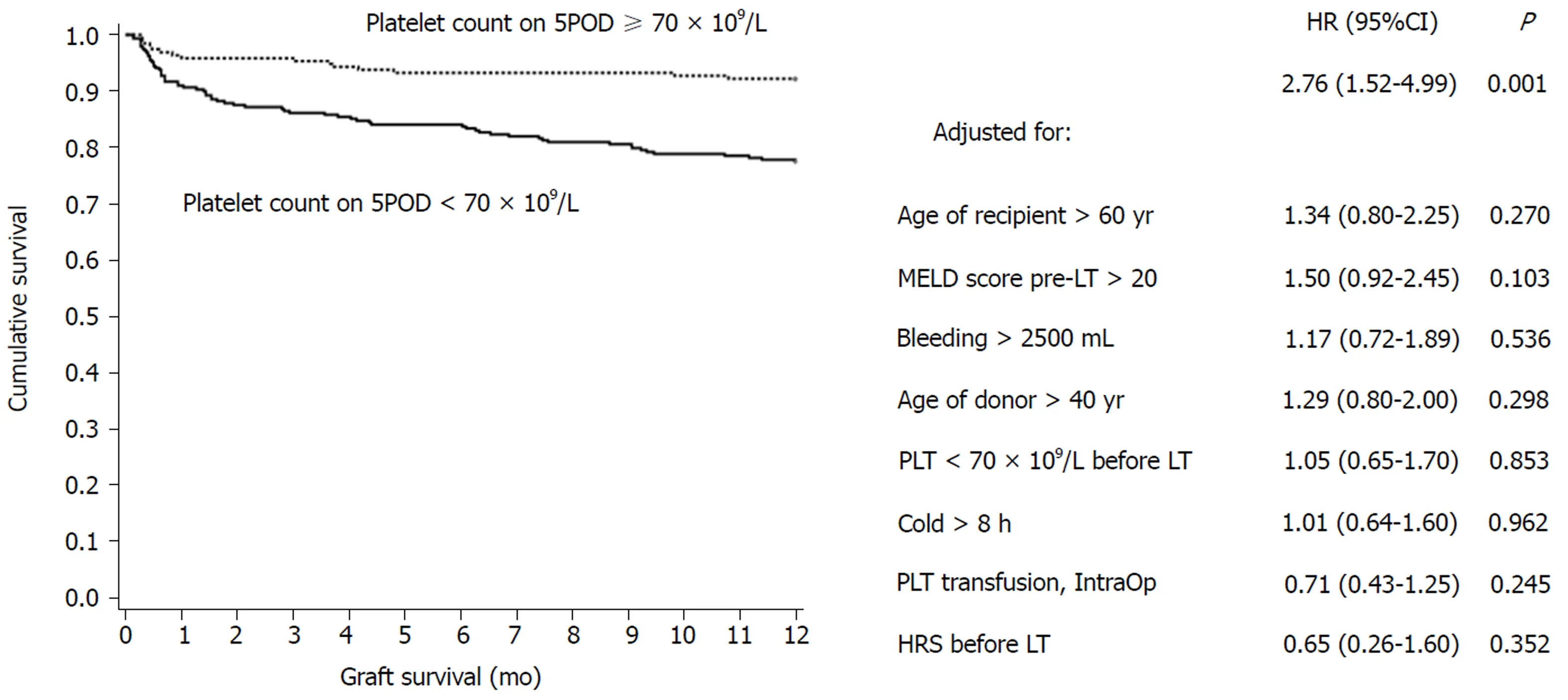
Figure 2 Cumulative survival of liver graft of patients with platelets < 70 × 109/L on fifth postoperative day, adjusted for different variables, during first year of follow-up after liver transplantation. 5POD: Fifth postoperative day; CI: confidence interval; HR: hazard ratio; HRS: Hepatorenal syndrome; IntraOp:Intraoperative; PLT: platelets; MELD: Model for end-stage liver disease; LT: Liver transplantation.
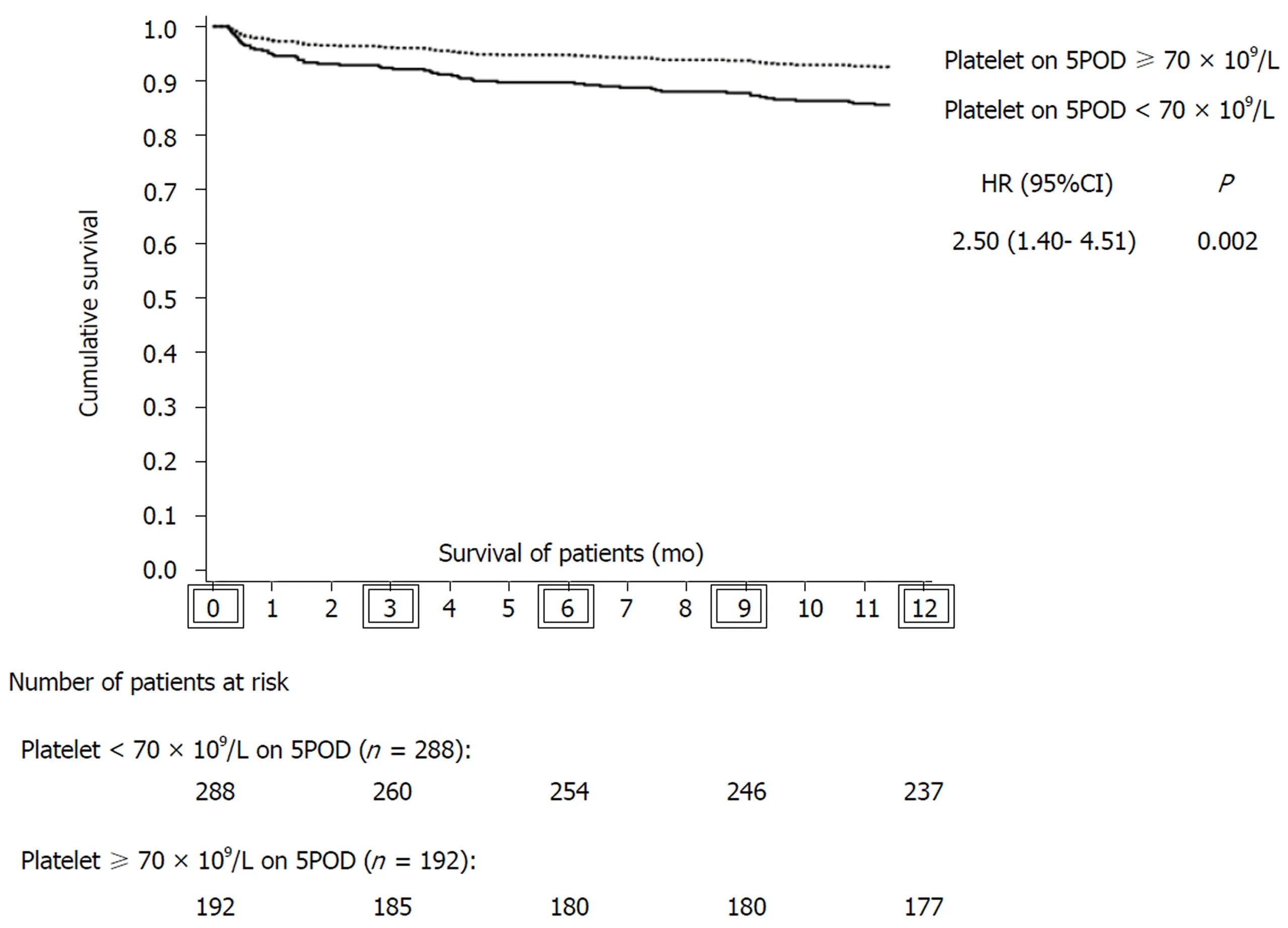
Figure 3 General survival within first year after liver transplantation (LT) of patients with platelet count < 70 × 109/L on fifth postoperative day vs patients with platelet count ≥ 70 × 109/L on 5POD. Together, the description of the number of patients at risk of death at, 0, 3, 6, 9 and 12 mo after liver transplantation,respectively. 5POD: Fifth postoperative day; CI: confidence interval; HR: hazard ratio; LT: liver transplantation.
ARTICLE HIGHLIGHTS
Research background
Platelets have several functions and exert dichotomous effects on the graft and on the patient in the context of liver transplantation (LT). Low platelet count (PC) after LT is associated with higher rates of complications. However, it is not clear whether low PC in the postoperative period is the cause or a surrogate marker of negative outcomes.
Research motivation
The accurate prediction of which LT recipients will do well and which ones will have serious complications remains somewhat elusive. Some authors suggest that low PC after LT can predict early posttransplant survival or graft loss. Confirmation of these findings can provide the clinician with the opportunity to intervene early and theoretically change the postoperative course of the patient.
Research objectives
To confirm the hypothesis that a low PC after LT is a predictor of death or graft loss.
Research methods
We performed a retrospective database analysis. PC from the preoperative to the seventh postoperative day (POD) were considered. C-statistic analysis was adopted to establish the day on which the PC showed the best performance. Recursive analyses of receiver operating characteristics curves allowed us to identify the cutoff point. Cox regression was performed to check whether low PC was a predictor of death, retransplantation or primary changes in graft function within one year after LT.
Research results
PC < 70 × 109/L on 5POD was defined as the ideal cutoff point for predicting death and retransplantation. PC < 70 × 109/L on 5POD was an independent risk factor for death at 12 mo after LT. In the Cox regression, patients with PC < 70 × 109/L on 5POD had worse graft survival rates up to one year after LT.
Research conclusions
A low PC on 5POD was associated with graft loss and mortality one year after LT. This result is in agreement with previous studies indicating that low PC in the immediate postoperative period of after LT is associated with negative outcomes.
Research perspectives
Our results reinforce the need to evaluate the role of interventions to maintain a minimum PC after LT. Preventive measures, such as platelet transfusion, suspension of potentially myelosuppressive drugs, and administration of serotonin or thrombopoietin, could be used in the future in the LT setting. However, further studies are still required before these interventions can be considered in clinical practice.
ACKNOWLEDGEMENTS
The authors thank the Liver Transplantation Group at Santa Casa de Misericórdia de Porto Alegre, RS, Brazil.
 World Journal of Hepatology2019年1期
World Journal of Hepatology2019年1期
- World Journal of Hepatology的其它文章
- Hepatocellular carcinoma in non-cirrhotic liver: A comprehensive review
- Treatment of primary sclerosing cholangitis in children
- Hepatitis in slaughterhouse workers
- Serum biomarkers and risk of hepatocellular carcinoma recurrence after liver transplantation
- Persistent risk for new, subsequent new and recurrent hepatocellular carcinoma despite successful anti-hepatitis B virus therapy and tumor ablation: The need for hepatitis B virus cure
- Temporal trends of cirrhosis associated conditions
