The effect of persistent high intraocular pressure on cataract surgery in eyes with acute primary closed angle glaucoma
Department of Ophthalmology, Tongji Hospital, Tongji Medical College Huazhong University of Science and Technology, Wuhan 430030, Hubei Province, China
Abstract
•AIM: To explore the effect of persistent high intraocular pressure (IOP) on cataract surgery in eyes with acute primary angle-closure glaucoma (PACG)and its correlative factor, and to discuss the choice of treatment for persistent high IOP.
•METHODS: Totally 284 cases(293 eyes) were diagnosed as acute PACG and underwent cataract surgery. According to preoperative IOP, these patients were divided into three groups: Group 1(188 eyes), Group 2 (61 eyes) and Group 3(44 eyes). Group 1 was defined that preoperative IOP can be controlled within the normal range under systemic and local drug. Group 2 was defined that preoperative IOP higher than 40 mmHg after drug therapy, which can be controlled after an anterior chamber puncture treatment. Group 3 was defined that preoperative IOP higher than 40 mmHg after multiple anterior chamber puncture. Group 1 underwent cataract extraction and intraocular lens (IOL) implantation. Group 2 and Group 3 underwent cataract extraction and IOL implantation with goniosynechiolysis. The preoperative and postoperative visual acuity, IOP, anterior chamber depth(ACD) and subfoveal choroidal thickness were obtained, and gonioscopic measurement of chamber angle was recorded. Preoperative and postoperative measurements were compared using non-parametric tests.
•RESULTS: After surgical treatment, the rate of postoperative one-week IOP control rate was respectively: Group 1 (100%), Group 2 (95%), Group 3 (82%) (the rate of Group 2 is higher than Group 3, χ2=4.795, P<0.05). The rate of the improved postoperative vision was respectively: Group 1 (92%), Group 2 (84%) and Group 3 (52%). Postoperative central anterior chamber depth of each group deepened obviously compared to preoperative, but the postoperative goniosynechia range of Group 3 was significantly wider than that of Group 1 and Group 2. Group 1 and Group 2 did not record postoperative hyphema, while 18% of Group 3 had recorded hyphema.
•CONCLUSION: Acute PACG eyes with persistent high preoperative IOP had good effects after cataract surgery, but demonstrated wider goniosynechia range and higher risk of hyphema compared to eyes with normal preoperative IOP.
•KEYWORDS:primary angle-closure glaucoma; acute attack; intraocular pressure
INTRODUCTION
Acute primary angle-closure glaucoma (PACG) is a sight-threatening situation characterized by a sudden and marked rise in intraocular pressure (IOP) due to obstruction of aqueous humour outflow. It is a true medical emergency that can cause permanent blindness in the affected eye in a short time. Once diagnosed, treatment should be immediately taken to reduce IOP and protect the visual function.
Usually IOP should be controlled within or near normal levels under systemic and local drugs before further treatment such as laser peripheral iridotomy and surgery, but occasionally there are some patients with severe adhesion, whose IOP failed to drop to normal range even after repeated anterior chamber puncture. In this case, surgery treatment should be taken in condition of high IOP and inflammation, but the controversy remains in the option of the surgical timing and appropriate treatment[1].
There is widespread sentiment that phacoemulsification and intraocular lens(IOL) implantation is an useful and safe method for the treatment of acute angle-closure glaucoma[2], but there is no clear answer to the question of whether cataract surgery can effectively reopen the closed anterior chamber for patients with persistent high preoperative IOP[3]. For this we analyzed retrospectively 284 cases of acute PACG had cataract surgery.
SUBJECTS AND METHODS
BasicDataTotally 284 cases (293 eyes) of acute PACG which accepted the cataract surgery admitted in Ophthalmology Department of Wuhan Tongji hospital from June 2013 to June 2017. All patients had different degrees of cataract. One hundred and seventeen cases(122 eyes)were male, 167 cases(171 eyes)were female, and the average age is 54±9 years old. Patients were excluded if they had undergone prior intraocular surgery or diagnosed as plateau iris by gonioscopy. All the participation was voluntary without a stipend and informed consent was signed from the subjects in written or in fingerprint. The principles outlined in the Declaration of Helsinki were fully followed.
GroupingSystemic drugs (mannitol, methazolamide) and local drugs (pilocarpine and beta blockers such as 0.5% timoptol eye drops) were routinely used. Anterior chamber punctured by 15 degree knife was immediately given when drugs failed to control IOP. Group 1 was defined as IOP could be controlled within the normal range under systemic and local drug; Group 2 was defined as preoperative IOP higher than 40 mmHg after drug therapy, but can be controlled after an anterior chamber puncture treatment. Group 3 was defined as whose preoperative IOP higher than 40 mmHg after multiple anterior chamber puncture.
SurgicalMethodsGroup 1 had cataract extraction and IOL implantation. Groups 2 and 3 had cataract extraction and IOL implantation with goniosynechialysis. The cataract extraction was performed with routine phacoemulsification through a temporal clear corneal incision, and a foldable posterior chamber IOL was placed within the capsular bag. For Groups 2 and 3, then with an ophthalmic viscosugical device (OVD) [hydroxypropyl methylcellulose 2% (Coatel)], the anterior chamber was deepened, then the OVD was injected two times over the entire angle to break the synechia, principally to the area of peripheral anterior synechia (PAS) without touching the trabecular meshwork or iris. Gonioscopy was not performed intraoperatively. At the end of the surgery, the OVD was carefully removed, and the anterior chamber was formed with balanced salt solution. All procedures were performed by two experienced surgeons.
All subjects’ eyes underwent a thorough ophthalmic evaluation, including anterior optical coherence tomography(OCT), gonioscopy, IOL-master, corneal endothelial counting, ultrasonic B-scan, enhanced depth imaging OCT(EDI-OCT), and optic nerve fiber layer thickness analysis. Axial length(AL), spur-spur distance, preoperative and one-week postoperative anterior chamber depth(ACD) measurement are completed by anterior OCT. Subfoveal choroidal thickness was scanned by EDI-OCT, and two images (horizontal and vertical sections)scanned using a single, 30° linear scan centered on the fovea. The choroid was measured from the outer portion of the hyper-reflective line that corresponded to the retinal pigment epithelium to the inner surface of the sclera. Demographic data, such as age, sex and blood pressure were collected. Tobramycin dexamethasone and nonsteroidal anti-inflammatory drugs were used locally postoperatively, once every 2h for 1wk,then four times a day for 2-3wk.
StatisticsThe experimental data were analyzed by SPSS 20.0 software, all measuring data expressed as mean±SD. The K-S non-parametric test was adopted to compare preoperative and postoperative data when one sample K-S test show discontinuity. Theχ2test was adopted to compare the inter-group difference of measurement data. Logistic regression analysis was applied to dispose the relativity among the indexes. The difference was statistically significant (P<0.05).
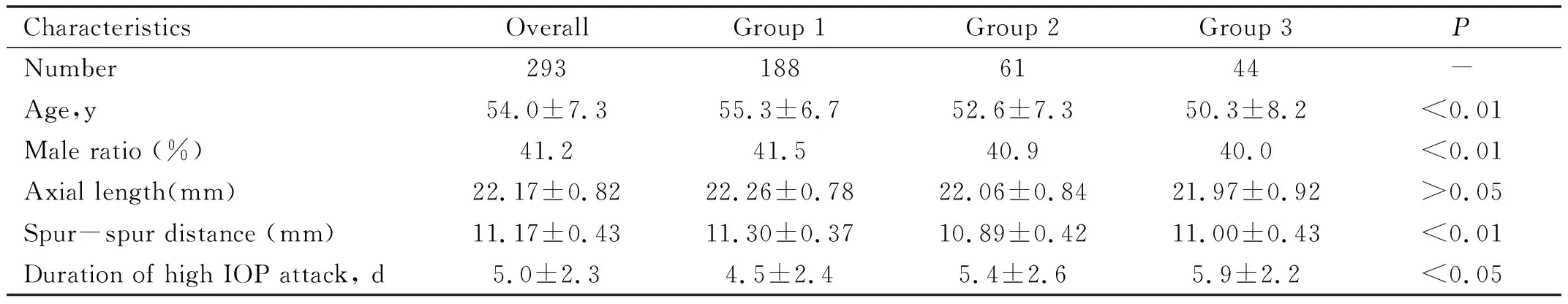
Table 1 Characteristics of the three groups mean±SD
IOP: Intraocular pressure. Significance of differences among subgroups:χ2test, ANOVA or Kruskal-Wallis test.
RESULTS
Preoperative IOP could be controlled within the normal range under systemic and local drug(Group 1):188 eyes. Preoperative IOP higher than 40 mmHg after drug therapy, but can be controlled after an anterior chamber puncture treatment(Group 2):61 eyes. Preoperative IOP higher than 40 mmHg after multiple anterior chamber puncture(Group 3): 44 eyes(Table 1).
VisualAcuityFor each group, postoperative one week best corrected visual acuity improved obviously (one sample K-S test,P<0.01, non-parametric test,P<0.01) (Figure 1).
Improved visual acuity was defined as an increased of more than 2 rows based on International Standard Chart, improved visual acuity rate was respectively: Group 1 (92%), Group 2 (84%), Group 3 (52%) (for Groups 2 and 3,improved visual acuity rate had no statistical difference, Chi-square,χ2=12.06,P<0.01).
IntraocularPressureAll IOP were measured by non-contact tonometer. Control of IOP was defined as without hypotensive drugs, IOP was controlled between 10 to 21 mmHg; partial control was defined as with the addition of topical glaucoma medications, IOP was controlled between 10 to 21 mmHg; invalid was defined as IOP was greater than 21 mmHg with the addition of topical glaucoma medications, and no significant improvement in the symptoms caused by high IOP. IOP control rate was defined as the control+ partial control/the total ratio. The postoperative one-week IOP of each group were well controlled. The postoperative one-week IOP control rate was respectively: Group 1 (100%), Group 2 (95%), Group 3 (82%). (IOP control rate of Group 2 was higher than that of Group 3, Chi-square,χ2=4.795,P<0.05).
AnteriorChamberBiologicalParametersChangeThe preoperative angle close range was respectively: Group 1, goniosynechia range less than 180°; Group 2, goniosynechia range were between 180°-270°; Group 3 goniosynechia range were between 180°-360°. The postoperative angle close range of the three groups had statistical differences (Table 2). The three groups all had significant deeper postoperative central ACD compared with preoperatively, and had no significant differences among groups (Table 3).
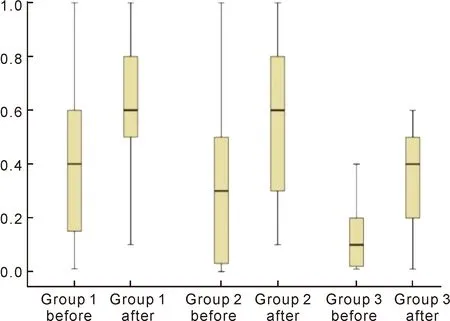
Figure1preoperativeandpostoperativevisualacuity.
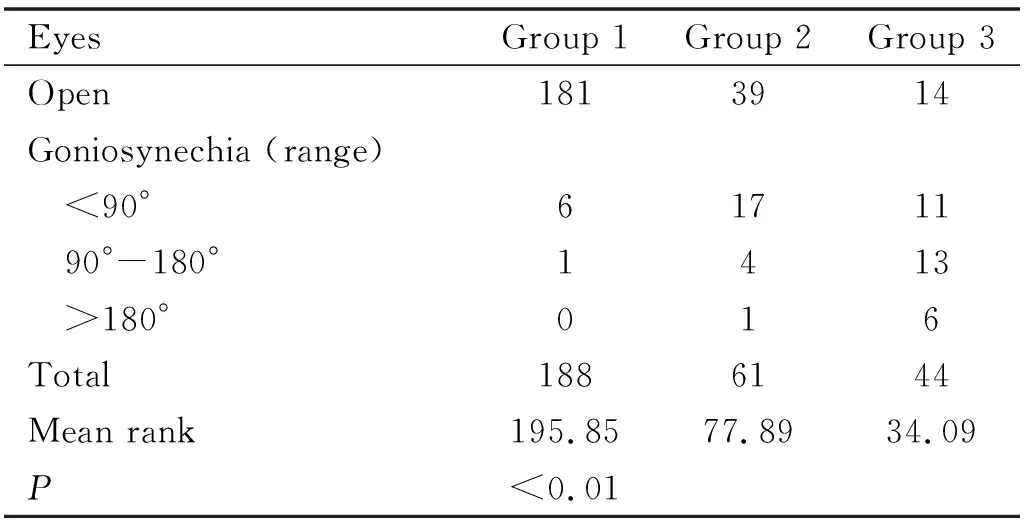
Table 2 Comparison of the postoperative angle close range of three groups (n)
PosteriorSegmentChangesPictures of optic disk were taken preoperatively(Figure 2). No optic disc hemorrhages was found in eyes of Group 1, and 5% of eyes in Group 2 found optic disc linear hemorrhages, 9% of eyes in Group 3 found optic disc linear hemorrhages. Eyes of Group 1 had postoperative greater subfoveal choroidal thickness compared with preoperatively, and had no significant differences among groups, as shown in Table 3.
SurgicalComplicationsThere were no severe complications in Groups 1 and 2, while 3 cases of Group 3 were recorded hyphema, including 1 case of suprachoroidal hemorrhage, 2 cases of Group 3 had fibrinoid aqueous reaction, and they recovered naturally.
DISCUSSION
Drug treatment has a limited and slow effect of lowering IOP. Especially for the frail elderly, systemic ocular hypotensive agents may be dangerous, as over time it may cause serious complications, such as renal damage or drug allergies. Therefore, for patients with persistent high preoperative IOP,surgery needs to be taken, as soon as possible, to control IOP and protect the visual function[4].
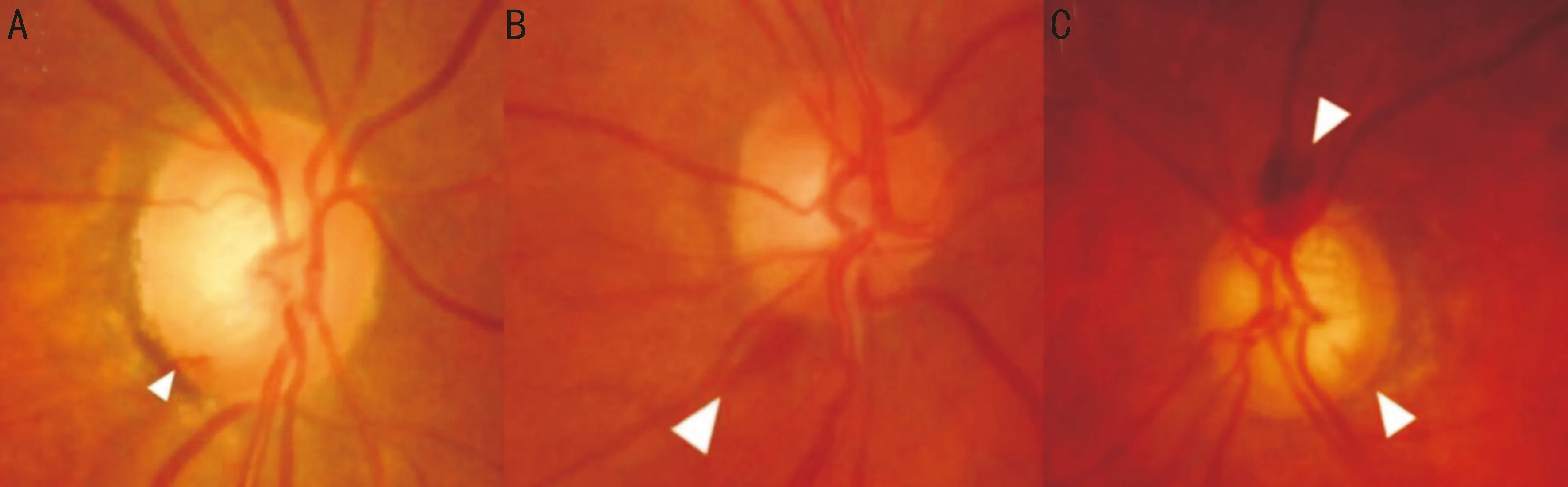
Figure2Threeofthepicturesofopticdisk(opticdischemorrhagesareindicatedbyawhitearrow).
Table3ACDandsubfovealchoroidalthickness
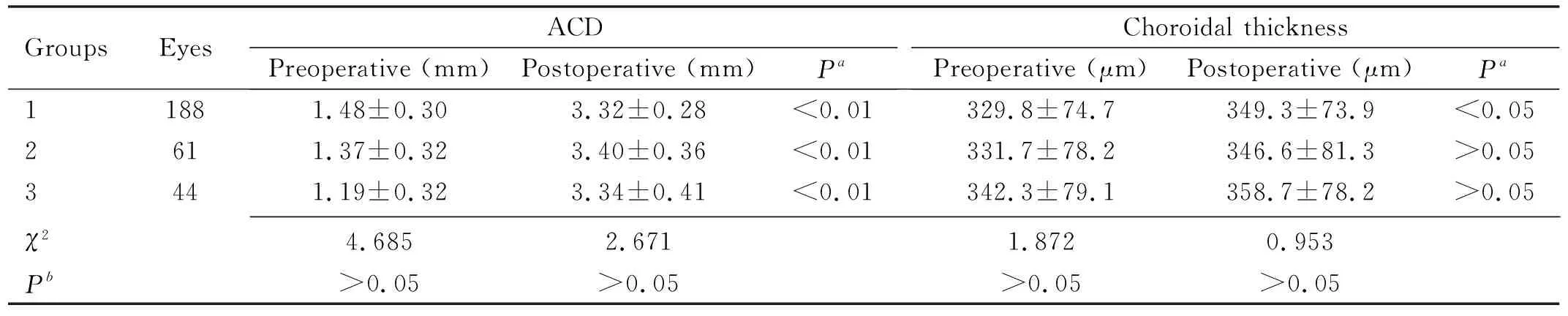
GroupsEyesACDPreoperative (mm)Postoperative (mm)PaChoroidal thicknessPreoperative (μm)Postoperative (μm)Pa11881.48±0.303.32±0.28<0.01329.8±74.7349.3±73.9<0.052611.37±0.323.40±0.36<0.01331.7±78.2346.6±81.3>0.053441.19±0.323.34±0.41<0.01342.3±79.1358.7±78.2>0.05χ24.6852.6711.8720.953Pb>0.05>0.05>0.05>0.05
ACD:Anterior chamber depth.aPmeans significance of differences between preoperative and postoperative: Wilcoxonnon-parametric test;bPmeans significance of differences among subgroups: Kruskal-Wallis test.
Cataract extraction with phacoemulsification reduces IOP by deepening the anterior chamber and opening the drainage angle in PACG eyes[5]. Although the role of cataract extraction in the treatment of PACG is becoming more affirmative, the challenge ahead is to predict which PACG eye will respond to removal of the cataract and the magnitude of response in terms of IOP reduction. So far, the effect of clear lens extraction surgery on acute PACG patients with persistent high preoperative IOP is rarely reported.
Our study found that in all groups eyes had significant deeper central ACD, broader chamber angle and flatter iris postoperatively, and no significant differences between groups. The main reasons are: on one hand, lens vault reduced postoperatively and the volume of anterior chamber decreased, on the other hand, cataract ultrasonic emulsification surgery may make the contact plane of pupil edge and the lens backwards, relieve lens-induced pupillary block and angle-closure, and make the non-adhesive chamber angle reopen[6-7]. However, in our study, the postoperative goniosynechia range of Group 3 was significantly wider than that of Groups 1 and 2, even combined with goniosynechialysis. Normally, surgical goniosynechialysis has been performed using surgical instruments or an Nd∶YAG laser, and proved effectively to release PAS in patients with angle-closure glaucoma[8]. In this study, goniosynechialysis was performed with OVD as a substitute for surgical instruments. The residual synechiae is probably due to permanent goniosynechia as a result of high IOP and inflammation. Some anatomical abnormality of anterior chamber angle, such as the ciliary body rotation, may also be involved[9].
The improved visual acuity rate of eyes with persistent high preoperative IOP is 52%, significantly lower than normal IOP group. The main reason may be optic nerve injury and corneal endothelial cells damage. Research has shown that corneal endothelial cell density was significantly reduced in acute PACG eyes compared with normal eyes[10-11]. Moreover, the suspensory ligament relaxation has been seen at times in acute PACG. It may cause deviation of IOL, thus may also have something to do with postoperative low vision.
Optic disc hemorrhages show acute ischemia of optic disc. It is closely related to the partial optic nerve fiber layer defect, and can be used as a sign of progress in visual field loss. Our study found that 9% of eyes with persistent high preoperative IOP were associated with optic disc linear hemorrhages. Research has shown that, especially when IOP is greater than 40 mmHg, optic nerve damage obviously increases with the duration of the high IOP[12]. Other data suggest that when acute high IOP more than 40 mmHg, it may cause acute anterior optic nerve ischemia or central retinal vein occlusion. When IOP is more than the central retinal artery systolic blood pressure (40 mmHg), central retinal artery occlusion and atrophy may happen within minutes[4]. Other studies have found that, the delay of surgery in glaucoma patients, is the most important single factor of vision loss. In this study, eyes with persistent high preoperative IOP underwent surgical treatment within a week. We attached great importance to reduction of inflammation reactions and IOP before surgery, and anterior chamber puncture were performed slowly for many times. Optic nerve injury was still inevitable. Anyway, clear lens extraction surgery for persistent high IOP eyes have a significant improvement of postoperative visual acuity, compared with traditional filtration surgery[6]. Further, if we took filtration surgery first, cataract after trabeculectomy may affect the filtering bleb.
The predominant mechanism in the development of acute PACG is increased resistance, which is caused by relative pupillary block preventing the aqueous humor from flowing through the pupil[13]. But recent interest has focused on choroidal expansion as an important factor involved in the pathophysiology of acute PACG[14-16]. This conjecture is based on the theory that choroidal expansion leads to forward lens movement and decreases the volume of the anterior chamber, thereby increasing the absolute IOP[17]. Our study found that the subfoveal choroidal thickness had of no significant difference between the persistent high IOP group and preoperative normal IOP group. But it could not prove that choroid expansion had no relation with mechanism of persistent high IOP, because we only measured the subfoveal choroidal thickness, and lack of the data of the remaining parts of the choroid[18].
In this study, the postoperative IOP control rate of persistent high IOP group is as high as 82%, though lower than the other two groups. It proved that cataract surgery was effective for acute PACG, even for persistent high IOP eyes. We also observed that there were still some cases in which postoperative IOP could not be controlled in the normal range, even more than 180°of chamber angle reopened. The reason may be that irreversible damage to the trabecular meshwork may have occurred in areas of synechial closure, with proliferation of iris or fibrous tissue into the intertrabecular space. The decreased aqueous outflow in these cases may be secondary to widening and fusion of adjacent trabecular beams, together with the homogeneous deposit enmeshing trabecular beams and spaces. It’s generally considered irreversible histological change in the trabeculum only occurs in PACG cases of long duration, while in acute PACG the trabecular damage is reversible after goniosynechia was released. But maybe there is some irreversible acute injury mechanism which is still not known to us.
When taking surgery under the state of persistent high IOP, complications is a thorny problem[19]. Because eyes under high IOP have serious ciliary injection and the ciliary body edema, and the lens-iris diaphragm moves forward thus causing ciliary block, when intraoperative and postoperative IOP falls sharply, especially after the traditional filtration surgery, choroidal vessels will rupture bleed, it will lead to explosive suprachoroidal hemorrhage, choroidal detachment and other serious complications[20]. In this study, 18% of persistent high IOP group had recorded hyphema, while the other groups did not appear to have postoperative hyphema. In this cases hyphema were finally absorbed. The hyphema was possibly due to inflammation and ciliary injection or more likely because of operation of goniosynechialysis[21].
In conclusion, the clear lens extraction surgery for the treatment of persistent high IOP of acute angle-closure glaucoma proved safe and effective, though demonstrated wider goniosynechia range had a higher risk of hyphema. Considering the irreversible optic nerve damage caused by continuous high IOP, timely surgery is highly desirable. Our experience is that slow and repeat anterior chamber penetration had great importance for eyes with persistent high IOP[22], as it prevented suprachoroidal hemorrhage and other serious complications.