综合护理措施干预在缓解产妇产后乳房胀痛中的应用效果
资海燕 陈少英
[摘要]目的 探討综合护理措施干预对产后产妇乳房胀痛的影响。方法 选取2018年1~12月在我院分娩的62例产妇作为研究对象,根据随机数字表法将其分为对照组和观察组,每组各31例。对照组产妇接受产后常规护理,观察组产妇在对照组基础上给予心理护理等综合性护理措施干预。观察并比较两组产妇不同时间点的泌乳量、乳房硬度分级和乳房胀痛评分。结果 护理后,观察组产妇产后第3、7天的泌乳量均多于对照组,差异有统计学意义(P<0.05)。两组产妇产后第3、7天的泌乳量均多于本组产后第1天,差异有统计学意义(P<0.05)。两组产妇产后第3、7天的乳房硬度分级情况均优于本组产后第1天,差异有统计学意义(P<0.05)。观察组产妇产后第3、7天的乳房硬度分级情况均优于对照组,差异有统计学意义(P<0.05)。两组产妇产后第3、7天的乳房疼痛视觉模拟量表(VAS)评分均低于本组产后第1天,差异有统计学意义(P<0.05)。观察组产妇产后第3、7天的乳房疼痛VAS评分均低于对照组,差异有统计学意义(P<0.05)。结论 对于产后乳胀的产妇,应用综合性护理干预措施具有更好的护理效果,能显著提高产妇的泌乳量,缓解乳胀和乳房疼痛,值得临床应用及推广。
[关键词]综合护理措施;乳胀;乳房疼痛;护理效果
[中图分类号] R473.5 [文献标识码] A [文章编号] 1674-4721(2019)12(c)-0238-04
Application effect of comprehensive nursing measures intervention in relieving postpartum puerperae with breast swelling and pain
ZI Hai-yan CHEN Shao-ying
Department of Obstetrics and Gynecology, the First People′s Hospital of Nansha District in Guangzhou City, Guangdong Province, Guangzhou 511462, China
[Abstract] Objective To explore the effect of comprehensive nursing measures intervention on breast swelling and pain in postpartum puerperae. Methods Sixty-two puerperae delivered in our hospital from January to December 2018 were selected as subjects and divided into control group (31 cases) and observation group (31 cases) according to random number table method. The puerperae in the control group received routine postpartum nursing, while the puerperae in the observation group received comprehensive nursing measures intervention such as psychological nursing on the basis of the control group. The lactation volume, breast hardness grade and breast pain score at different time points were observed and compared between the two groups. Results After nursing, the maternal lactation volumes of the observation group on the 3rd and 7th day after delivery were higher than those of the control group, and the differences were statistically significant (P<0.05). The lactation volumes of the two groups on the 3rd and 7th day after delivery were higher than those on the 1st day after delivery, the differences were statistically significant (P<0.05). The grades of breast hardness on the 3rd and 7th day after delivery were better than those on the 1st day after delivery in the two groups, and the differences were statistically significant (P<0.05). In the observation group, the grades of breast hardness on the 3rd and 7th day after delivery were better than those of the control group, with statistically significant differences (P<0.05). The visual analogue scale (VAS) scores of breast pain on the 3rd and 7th day after delivery were lower than those on the 1st day after delivery, and the differences were statistically significant (P<0.05). The VAS scores of the observation group on the 3rd and 7th day after delivery was lower than those of the control group, with statistically significant differences (P<0.05). Conclusion For puerperae with postpartum breast swelling, the application of comprehensive nursing intervention measures has a better nursing effect, can significantly improve puerperae′s lactation volume, alleviate breast swelling and pain, worthy of clinical application and promotion.
[Key words] Comprehensive nursing measures; Breast swelling; Breast pain; Nursing effect
产后乳房胀痛是产妇分娩后1周内常发生的现象,多表现为乳房胀满、疼痛和硬结等现象,原因是乳腺淋巴潴留、静脉充盈、间质水肿及导管未完全通畅等[1]。随着哺乳时间渐长,乳胀问题通常会自动缓解。但部分产妇的乳胀现象持续时间较长,乳房胀痛影响了产妇进行母乳喂养的信心和成功率,需要及时进行干预[2]。产后护理在指导产妇母乳喂养方面可扮演重要角色,能够减轻相关乳房症状,增强产妇进行母乳喂养的信心,并提高母乳喂养的成功率。但常规护理措施由于缺乏系统性,护理效果有限,并不能很好的解决产妇产后乳胀等问题[3],综合护理措施是综合应用多种护理手段提高患者康复效果的举措。本研究选取在我院分娩的62例产妇作为研究对象,结合我院实际情况,旨在探讨综合护理措施干预相比常规产后护理对产妇产后乳胀和乳房疼痛的影响,现报道如下。
1资料与方法
1.1一般资料
选取2018年1~12月在我院分娩的62例产妇作为研究对象。纳入标准:①产妇产后出现乳胀现象;②产妇依从性好,可配合护理干预。③在入组前,产妇及家属均知晓本研究情况并签署知情同意书。排除标准:①其他病理因素导致的乳者;②合并其它乳腺疾病者;③不能配合、依从性差的产妇。
最终纳入62例产妇,根据随机数字表法将其分为对照组和观察组,每组各31例。对照组产妇,年龄20~38岁,平均(27.63±5.11)岁;孕龄37~41周,平均(39.32±1.25)周;体重50~70 kg,平均(63.57±4.50)kg。观察组产妇,年龄19~36岁,平均(28.53±4.60)岁;孕龄37~42周,平均(39.97±1.32)周;体重51~70 kg,平均(65.27±4.23)kg。两组产妇的年龄、孕龄和体重等一般资料比较,差异无统计学意义(P>0.05),具有可比性。本研究符合临床研究伦理准则,并获得医院医学伦理委员会的许可。
1.2研究方法
对照组产妇接受常规产后护理,包括指导产妇尽早进行母乳喂养和按需哺乳等。
观察组产妇在对照组基础上应用综合护理措施干预,具体如下:①心理护理。产妇对于分娩过程容易产生焦虑、紧张的心理,这种情绪延续到产后就会影响产妇进行母乳喂养的信心。助产士和其它护理人员在产前和产后通过交流沟通的方式了解产妇的心理动态,让她们正确的认识母乳喂养,了解母乳喂养的过程和益处。对于负性情绪较重的产妇给予积极的心理疏导,帮助她们建立母乳喂养的习惯。②全程母乳喂养指导。产后24 h内,由经验丰富的高年资助产士一对一的对产妇进行母乳喂养指导,并在床旁指导评估乳房和新生儿吮吸情况,如有异常,现场进行指导和纠正。出院后,在门诊和电话进行随访,提供延续性喂养指导。③乳房按摩。在孕妇生产前教会孕妇掌握乳房按摩方法,按摩前,于乳晕周围均匀涂抹润肤油,用手掌鱼际肌轻轻按摩乳房皮肤,避开乳头,从乳房根部顺乳管方向按摩,每天3次,每次5 min左右,保持乳管通畅。④婴儿吮吸护理。指导产妇与婴儿早接触、早吸吮,帮助新生儿吸吮乳头,时间超过半小时,提高母乳喂养成功率。在分娩后30 min助产士帮助婴儿正确含接乳头,每侧乳头吸吮约15 min,2 h重复1次,并让产妇和婴儿多接触,指导产妇正确的喂养方式和技巧,使婴儿和母亲达到胸贴胸、腹贴腹、下额贴乳房的哺乳姿势,同时根据婴儿需要及时喂奶,避免婴儿熟睡3 h以上仍拒绝喂奶导致乳汁淤积。另外注意夜间坚持哺乳,夜间泌乳素分泌量是白天的数十倍,因此产后早期多次吸吮可减轻胀奶的发生。⑤乳房理疗。应用产后康复综合治疗仪(北京拓殖置业科技有限公司,型号TZ-CH300)进行产后乳房理疗,产妇取平卧位,治疗电极片分别置于产妇双侧乳房上,程序选择乳腺管不通程序,刺激强度根据产妇的耐受情况确定,每天2次理疗,每次20 min左右。
两组护理周期均为产后1周。
1.3观察指标及评价标准
观察并比较两组产妇不同时间点的泌乳量、乳房硬度分级和乳房胀痛评分。
①两组产妇泌乳量的比较。观察产妇产后第1、3、7天的泌乳量。②两组产妇乳房硬度分级情况的比较。分别于产后第1、3、7天评价产妇的乳房硬度,共分为3级,分别为:Ⅰ度——触之如嘴唇,为正常或轻度乳胀;Ⅱ度——触之如鼻尖,为中度乳胀;Ⅲ度——触之如额头,为重度乳胀。③两组产妇乳房疼痛程度的比较。分别于产后第1、3、7天应用视觉模拟量表(VAS)评定产妇的乳房疼痛程度,分值为0~10分,分值越高,代表产妇的乳房痛感越强。
1.4统计学方法
采用SPSS 25.0统计学软件进行数据分析,计量资料用均数±标准差(x±s)表示,两组间比较采用t检验,组内不同时间两两比较采用t检验;计数资料采用率表示,组间比较采用χ2检验;等级资料采用秩和检验;以P<0.05为差异有統计学意义。
2结果
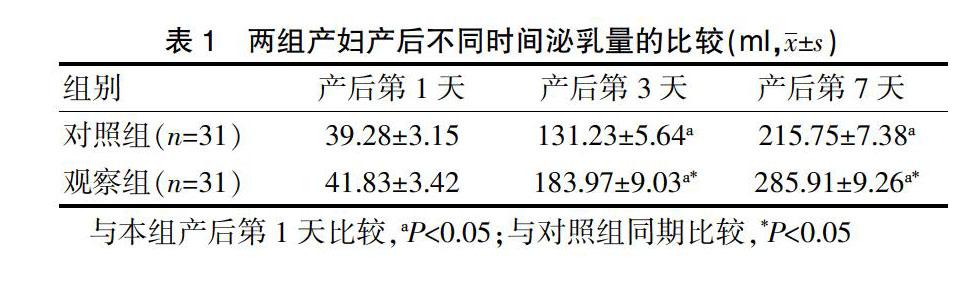
2.1两组产妇产后不同时间泌乳量的比较
护理后,两组产妇产后第1天的泌乳量比较,差异无统计学意义(P>0.05)。两组产妇产后第3、7天的泌乳量均多于本组产后第1天,差异有统计学意义(P<0.05)。观察组产妇产后第3、7天的泌乳量均多于对照组,差异有统计学意义(P<0.05)(表1)。
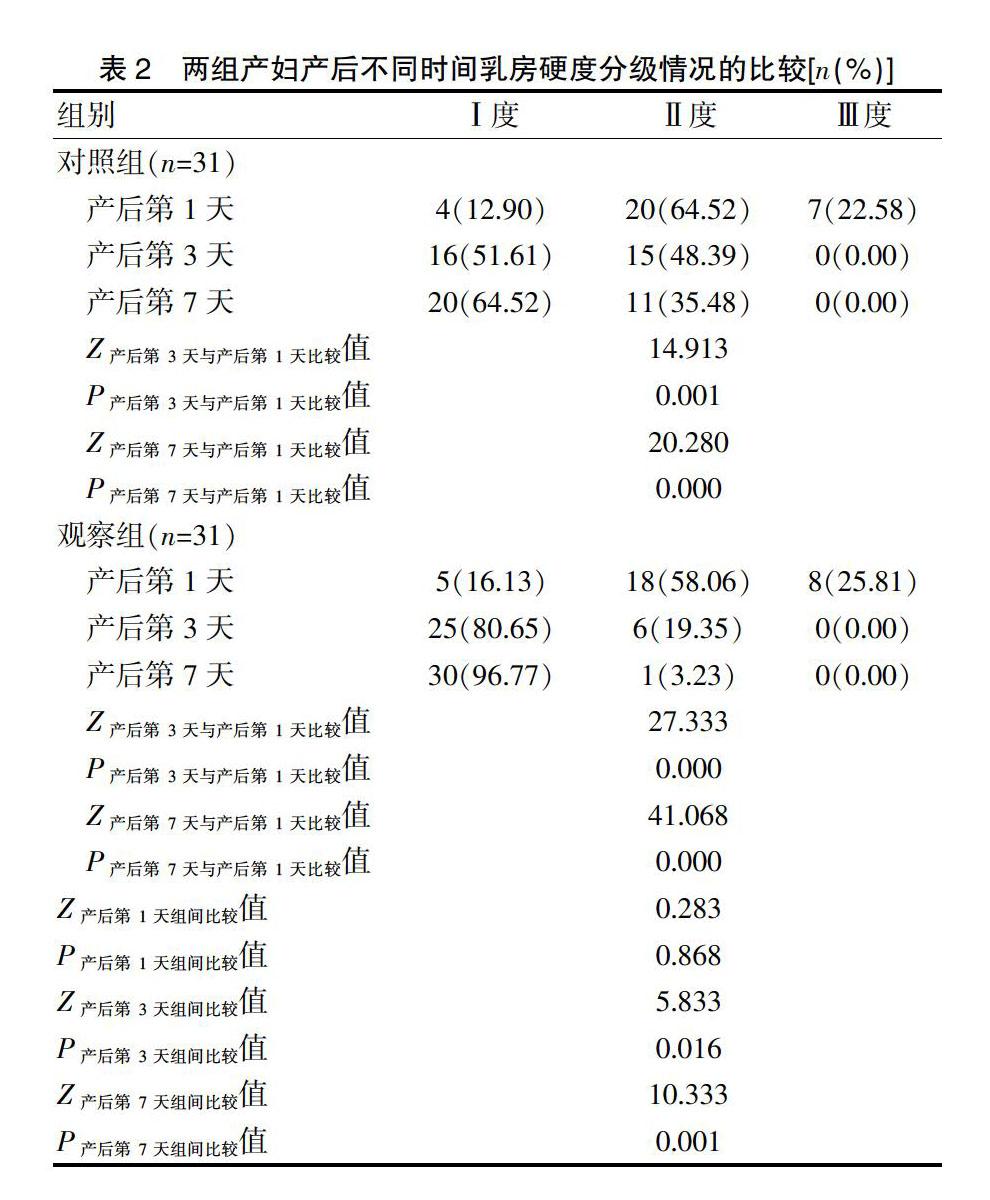
2.2两组产妇产后不同时间乳房硬度分级情况的比较
护理后,两组产妇产后第1天的乳房硬度分级情况比较,差异无统计学意义(P>0.05)。两组产妇产后第3、7天的乳房硬度分级情况均优于本组产后第1天,差异有统计学意义(P<0.05)。观察组产妇产后第3、7天的乳房硬度分级情况均优于对照组,差异有统计学意义(P<0.05)(表2)。