Applicability of the PRECISE-DAPT score in elderly patients with myocardial infarction
Carme Guerrero, Albert Ariza-Solé, Francesc Formiga, Manuel Martínez-Sellés, María T Vidán,Jaime Aboal
1Department of Cardiology, Hospital Universitari de Bellvitge, L’Hospitalet de Llobregat, Barcelona
2Geriatrics Medicine Unit, Internal Medicine Department, Hospital Universitari de Bellvitge, L’Hospitalet de Llobregat, Barcelona
3Department of Cardiology, Hospital General Universitario Gregorio Marañón, Madrid
4Geriatrics Medicine Department, Hospital General Universitario Gregorio Marañón, Madrid
5Department of Cardiology, Hospital Universitari Josep Trueta, Girona
Abstract Background Elderly patients with acute coronary syndromes (ACS) are at higher risk both for ischemic and bleeding complications.Current guidelines recommend the PRECISE-DAPT score for bleeding risk stratification in this setting, but no study assessed its applicability in elderly patients. This study aimed to assess the performance of the PRECISE-DAPT score in a series of non-selected elderly patients with ACS from routine clinical practice. Methods The IFFANIAM registry included prospectively patients aged ≥ 75 years with ST segment elevation myocardial infarction (STEMI). Main outcome measured was the incidence of relevant bleeding after discharge (bleeding leading to hospital readmission, need for transfusion, intervention, stop of antithrombotic drugs or death). Bleeding risk was classified: (A) according to PRECISE-DAPT values above or not the recommended cut-off point (≥ 25); and (B) according to the quartiles of PRECISE-DAPT values observed in the IFFANIAM series (Q1: < 30; Q2: 30-35; Q3: 36-44; Q4: ≥ 45). Results A total of 208 patients were included. Mean age was 81.9 ± 4.5 years. Most patients (92.6%) had a PRECISE-DAPT value > 25. A total of 25 patients (12.0%) had bleeding events and 49 patients (23.6%) died. No significant differences regarding the incidence of bleeding were observed according to the recommended cutt of point ≥ 25. However, a progressive increase in the incidence of bleeding was observed across PRECISE-DAPT quartiles observed in this series (P = 0.038). Conclusions The vast majority of elderly patients have PRECISE-DAPT values above the recommended cut-off point for bleeding risk. Using different cut-off points could be a more rational approach for predicting bleeding risk in these complex patients.
J Geriatr Cardiol 2018; 15: 713-717. doi:10.11909/j.issn.1671-5411.2018.12.003
Keywords: Acute coronary syndromes; Bleeding; Prognosis; The elderly
1 Introduction
The ageing of population is leading to a progressive increase in the number of elderly patents admitted with acute coronary syndromes (ACS).[1]These patients are at higher risk both for ischemic and bleeding complications, mortality and consumption of healthcare resources.[2]Therefore, the care of patients with ACS at older ages is becoming a major healthcare problem.[3]
On the other hand, there is strong evidence about the association between bleeding complications and increased mortality in this scenario.[4]Post-discharge bleeding episodes in patients with ACS have also been associated to poorer outcomes.[5]Bleeding risk is one of the main limiting factors for the choice of antithrombotic therapy in these patients.[6]
Current guidelines[7]recommend the use of the PRECISE-DAPT score[8]for bleeding risk stratification in this setting, suggesting a more conservative antithrombotic approach in patients with a PRECISE-DAPT value ≥ 25. Age accounts for a significant proportion of points of this score,and elderly patients have commonly high score values. To our knowledge, no study assessed the applicability of the PRECISE-DAPT score in patients at older ages. Therefore,the aim of this study was to assess the performance of the PRECISE-DAPT score in a series of non-selected elderly patients with ACS from routine clinical practice.
2 Methods
The IFFANIAM registry[9]included prospectively pa-tients aged 75 years or older with ST segment elevation myocardial infarction (STEMI) undergoing primary percutaneous coronary intervention. A comprehensive geriatric assessment was performed during the admission, assessing clinical outcomes at mid-term follow up.
For the purpose of this subject analysis, we assessed 208 consecutive patients from this registry admitted in a tertiary care hospital and surviving after the admission. We registered baseline clinical characteristics, biochemistry, echocardiographic and angiographic data. PRECISE-DAPT score value was calculated for each patient.
A clinical follow up was performed by phone contact or review of medical records. Main outcome measured was the incidence of clinically relevant bleeding episodes after discharge, defined as those bleeding episodes leading to hospital readmission, need for transfusion, intervention, stop of antithrombotic drugs or death. Patients were classified according to their bleeding risk: (A) according to if PRECISE-DAPT score values were or not above the recommended cut-off point (≥ 25); and (B) according to the quartiles of PRECISE-DAPT score values observed in the IFFANIAM series (Q1: < 30; Q2: 30-35; Q3: 36-44; Q4: ≥45).
The association between PRECISE-DAPT score (as a continuous variable) and the incidence of post-discharge bleeding was assessed by a Fine and Gray competing risks regression method, considering the incidence of clinically relevant bleeding as dependent variable and mortality not due to bleeding as competing event. The discriminative ability of the model was assessed by calculating Receiver Operating Chaacteristics (ROC) curves and their corresponding area under the curve (AUC).
An additional analysis was performed in order to explore the specific contribution of each of the components of the score to the incidence of post-discharge bleeding in patients form the IFFANIAM registry. This analysis was also performed by Fine and Gray competing risks regression method, considering the incidence of clinically relevant bleeding as dependent variable and mortality not due to bleeding as competing event. All the components of the PRECISEDAPT score (age, haemoglobin, creatinine clearance, white blood cell count and previous bleeding) were included in the model as independent variables. All analyses were performed by STATA 14.
3 Results
A total of 208 patients were included, of whom 115(55.3%) were male. Mean age was 81.9 ± 4.5 years. Mean PRECISE-DAPT score value was 38 (range 15-83). Clinical characteristics for the whole cohort are shown in Table 1.
Clinical follow up was performed in 200 patients(96.1%). Median follow up time was 861 days (interquartile range 743), a total of 25 patients (12.0%) had bleeding events and 49 patients (23.6%) died. Most common causes of death were of non-cardiac origin (34/49, 69.4%), especially infections (12, 35.3%) and malignancy (3, 8.8%).Median time to occurrence of bleeding was 231 days, and 24% of bleeding events occurred within the first three months.
Patients who suffered bleeding events had slightly higher PRECISE-DAPT score values, without significant differences regarding age, sex, clinical characteristcs or geriatric syndromes. No significant differences regarding the incidence of bleeding were observed according to the recommended cut of point PRECISE-DAPT ≥ 25. However, a progressive increase in the incidence of bleeding was observed across PRECISE-DAPT quartiles observed in this series (Figure 1).
The PRECISE-DAPT score as a continuous variable was significanty associated with a higher incidence of post discharge bleeding [Sub-hazard ratios (SHR) = 1.03, 95% CI:1.01-1.05; P = 0.049]. Overall, the discriminative ability of the model was modest (AUC = 0.621, 95% CI: 0.501-0.741;P = 0.062). Using the quartiles of PRECISE-DAPT significantly improved the predictive ability of the recommended cut-off point [net reclassification improvement (NRI) =0.174, index discrimination improvement (IDI) = 0.182; P =0.021].
The specific contribution of each of the components of the PRECISE-DAPT score for predicting bleeding in these patients is shown in Table 2. The only variable with a significant association with post discharge bleeding was baseline haemoglobin (SHR = 0.77, 95% CI: 0.71-0.83; P =0.001).
4 Discussion
Recommended bleeding risk scores in patients with ACS were developed from series with a low representation of patients at older ages.[10,11]This is probably one of the main reasons for the lower ability of these scores for predicting bleeding in elderly patients. Likewise, the PRECISE-DAPT score was developed in a series from 8 randomized clinical trials with a mean age about 60-65 years. Age is one of the main predictors of bleeding in the PRECISE-DAPT series,accounting for a significant proportion of the score. In fact,an age of 75 years is equal to 12 points of the score. Therefore, the vast majority of elderly patients will have PRECISE-DAPT score values above the recommended cut-offpoint ≥ 25. In fact, 92.6% of patients from this series had values ≥ 25), in contrast to the original PRECISE-DAPT series, in whom these patients were only about 25% of case.

Figure 1. Proportion of patients suffering post-discharge bleeding events. (A): According to PRECISE-DAPT values above or not the recommended cut-off point (≥ 25); and (B): according to the quartiles of PRECISE-DAPT values observed in the IFFANIAM series.
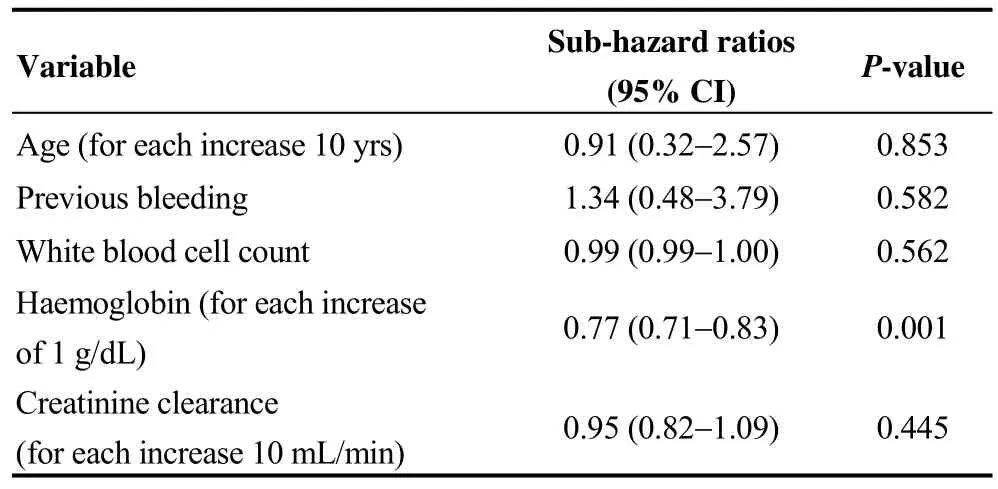
Table 2. Specific contribution of each of the components of the PRECISE-DAPT score for the prediction of clinically relevant bleeding in the IFFANIAM series.
The role of a comprehensive geriatric assessment for predicting bleeding in elderly patients with ACS remains poorly understood. While a significant association between frailty and in-hospital bleeding has been suggested,[12]other reports described a modest predictive role of ageing related variables, mainly driven by the effect of comorbidity.[13]No study assessed the role of frailty and other ageing variables for the prediction of post-discharge bleeding in patients with ACS. Data from our study revealed no significant association with bleeding for any of the different components of the geriatric assessment.
On the other hand, baseline haemoglobin was the only variable significantly associated with bleeding in our patients. The loss of effect of age might be due to the selection of patients aged 75 years or older, thus reducing the variability of patients values regarding this component of the score. This fact might have lead to a reduction of the overall predictive ability of the PRECISE-DAPT score in this setting. On the other hand, significant changes of the magnitude of the association between known risk factors and bleeding in elderly patients with ACS have been previously been described.[14]However, these data should be cautiously interpreted due to the low number of events observed in this study.
Current guidelines suggest a more conservative approach in patients with a PRECISE-DAPT score value ≥ 25. In our opinion, this may not be the optimal approach in elderly patients, which in turn have higher prevalence of diabetes mellitus, previous revascularization, and more extensive coronary artery disease or left main disease, and therefore are usually at higher risk for recurrent ischemic events.[15]Using different cut-off points in patients at older ages could probably be a more rational approach for predicting bleeding risk in these complex patients.
This study has some limitations, such as its moderate sample size, the relativey low number of events and the low utilisation of ticagrelor. In addition, information about the DAPT duration was not available, and the bleeding definition used was different form the TIMI bleding classification used in the original publication. Finally, these data come from a single center, so our findings should be validated in larger series with different clinical profile and management.
Despite these limitations, in our opinion these data reasonably show the need for adapting of the PRECISE-DAPT score in non-selected elderly patients with ACS from routine clinical practice. Optimizing risk sratification and clinical management in these age subgroup may lead to a more rational healthcare resources management.
Acknowledgments
All authors report no conflicts of interest.
 Journal of Geriatric Cardiology2018年12期
Journal of Geriatric Cardiology2018年12期
- Journal of Geriatric Cardiology的其它文章
- Heart failure mortality compared between elderly and non-elderly Thai patients
- Value of cystatin C in predicting atrial fibrillation recurrence after radiofrequency catheter ablation
- Perspective of delay in door-to-balloon time among Asian population
- Characterization of coronary atherosclerotic plaques in a homozygous familial hypercholesterolemia visualized by optical coherence tomography
- Contralateral pneumothorax in the subacute phase after pacemaker implantation: lead retention and follow-up
- Hypertension, abnormal blood pressure circadian pattern, and frailty:data from the literature
