2017 Chinese expert consensus on the clinical application of serum marker for thyroid cancer
Ming Gao, Minghua Ge, Qinghai Ji, Ruochuan Cheng, Hankui Lu, Haixia Guan, Wei Cui, Li Gao, Zairong Gao, Lin Guo0, Zhuming Guo, Tao Huang, Xiaoming Huang, Yansong Lin, Qinjiang Liu, Xin Ni, Jianwu Qin, Li Ren, Zhongyan Shan, Hui Sun, Xudong Wang, Zhengang Xu0, Yang Yu, Bin Zhang, Daiwei Zhao, Ying Zheng, Jingqiang Zhu, Xiangqian Zheng, Chinese Association of Thyroid Oncology (CATO),China Anti-Cancer Association
1Department of Head and Neck Tumor, Tianjin Medical University Cancer Institute and Hospital; National Clinical Research Center for Cancer, Key Laboratory of Cancer Prevention and Therapy, Tianjin; Tianjin’s Clinical Research Center for Cancer,Tianjin 300060, China; 2Department of Head and Neck, Zhejiang Cancer Hospital, Hangzhou 310022, China; 3Department of Head and Neck Tumor, Fudan University Shanghai Cancer Center, Shanghai 200433, China; 4Department of General Surgery,First Affiliated Hospital of Kunming Medical University, Kunming 650032, China; 5Department of Nuclear Medicine, The Sixth Affiliated Hospital of Shanghai Jiao Tong University, Shanghai 200025, China; 6Department of Endocrinology, The First Hospital of China Medical University, Shenyang 110001, China; 7Department of Clinical Laboratory, Cancer Hospital Chinese Academy of Medical Science, Beijing 100021, China; 8Department of Head and Neck, Sir Run Run Shaw Hospital, Zhejiang University School of Medicine, Hangzhou 310020, China; 9Department of Nuclear Medicine, Union Hospital Tongji Medical College Huazhong University of Science and Technology, Wuhan 430030, China; 10Department of Clinical Laboratory, Fudan University Shanghai Cancer Center, Shanghai 200433, China; 11Sun Yat-sen University Cancer Center, Guangzhou 510060,China; 12Department of Thyroid and Breast, Union Hospital Tongji Medical College Huazhong University of Science and Technology, Wuhan 430030, China; 13Department of Otolaryngology, Sun Yat-sen Memorial Hospital, Sun Yat-sen University, Guangzhou 510120, China; 14Department of Nuclear Medicine, Peking Union Medical College Hospital, Beijing 100730, China; 15Department of Head and Neck, Gansu Provincial Cancer Hospital, Lanzhou 730050, China; 16Department of Head and Neck, Beijing Children’s Hospital, Capital Medical University, Beijing 100045, China; 17Department of Thyroid, Head and Neck, Henan Cancer Hospital, Zhengzhou 450008, China; 18Department of Clinical Laboratory, Tianjin Medical University Cancer Institute and Hospital; National Clinical Research Center for Cancer, Key Laboratory of Cancer Prevention and Therapy, Tianjin; Tianjin’s Clinical Research Center for Cancer, Tianjin 300060, China; 19Department of Thyroid, Sino Japanese Union Hospital of Jilin University, Changchun 130033, China; 20Department of Head and Neck, Cancer Hospital Chinese Academy of Medical Sciences, Beijing 100021, China; 21Department of Head and Neck, Peking Union Medical College Hospital, Beijing 100730, China; 22Department of General Surgery, The Second Affiliated Hospital of Guizhou Medical University, Kaili 556099, China; 23Department of Head and Neck, Jilin Tumor Hospital, Changchun 130012, China;24Department of Thyroid and Breast, West China School of Medicine, West China Hospital, Sichuan University, Chengdu 610047, China
In recent years, the clinical incidence of thyroid cancer has been increasing year by year, and its risk assessment and clinical management methods have also been accordingly modified and constantly improved. There are great differences between the clinical diagnostic and therapeutic modes and disease management of thyroid cancer employed by various medical institutions in China, particularly with regard to the clinical application of serum marker of thyroid cancer. To this end, the China Anti-Cancer Association Thyroid Cancer Specialized Committee Chinese Association of Thyroid Oncology organized this compilation of Expert Consensus on Clinical Application of Serum Marker of Thyroid Cancer to help and impel relevant clinical institutions and professionals to standardize clinical diagnosis, treatment, and long-term management of thyroid cancer, and to properly utilize the serum marker for scientific auxiliary clinical diagnosis and assessment of thyroid cancer before and after operation. A total of 14 recommendations have been put forward in this consensus for measuring the levels of serum marker of thyroid cancer. In view of the limited references,especially regarding the perspective data currently available at home and abroad, omissions are inevitable. Moreover, we also hope that the professionals can give more valuable suggestions for regular revision in the future (see categories of recommendations in Table 1 and detailed recommendations in Table 2).
Criteria for setting of recommendation grade
The recommendations on the clinical application of serum marker of thyroid cancer in Expert Consensus are based on evidence-based medicine and expert opinions, and the categories of recommendations are as follows:
For the clinical laboratory test of serum marker of thyroid cancer, immunological test methods are more commonly used at present, including methods used for estimating levels of thyroglobulin (Tg) and calcitonin (Ctn). Ctn is the serum marker of medullary thyroid carcinoma (MTC), and Tg can be used as the serum marker of differentiated thyroid carcinoma (DTC). Anti-thyroglobulin antibody (TgAb) is the autoimmune antibody generated against Tg, and the existence of serum TgAb and the quantitative changes associated with it have a direct impact on the measurement of the serum Tg value. The carcinoembryonic antigen (CEA)is associated with diagnosis and clinical progress in some patients with MTC, and it can be used as a serum marker for MTC along with Ctn.
DTC
Preoperative serological test and assessment of DTC
Recommendation 1: For all patients with thyroid cancer considered for operative treatment, thyroid function including serum thyroid-stimulating hormone level shall be tested before the operation (grade of recommendation: A).For all patients with thyroid tumor considered for operative treatment, thyroid function, including the level of thyroidstimulating hormone (TSH), shall be tested. Assessing thyroid function can help surgeons and anesthetists to judge the safety in operative treatment of patients, and preoperative thyroid function shall be routinely tested. For patients with abnormal thyroid function, medical treatment shall be appropriately performed to ensure that the thyroid function is within the acceptable range for surgery. A previous study1showed that the incidence of malignant nodules in patients with thyroid tumor and TSH level below the normal range is lower than that in patients with normal or elevated TSH level. Therefore, to some extent, TSH level serves as a meaningful reference for malignant tumor assessment, and it is routinely recommended to measure it.
Recommendation 2: It is not recommended to use Tg for diagnosis and differentiation of benign and malignant thyroid tumor (grade of recommendation: E).
Tg is the specific protein generated by thyroid and secreted by the thyroid follicular epithelial cells. Many thyroid diseases can cause the elevation of serum Tg level, including DTC, goiter, thyroiditis, thyroid injury, hyperthyroidism, etc.At present, the detection reagents are unable to distinguish“tumor-induced” Tg from the “normal tissue-derived.”Therefore, serum Tg cannot be used to distinguish the difference between benign and malignant thyroid tumor2-4.
Recommendation 3: Tg and TgAb levels can be tested routinely before operation of thyroid cancer, and it is recommended to simultaneously test both for assessment of the initial clinical state and serological index baseline(grade of recommendation: A).
High level of preoperative serum Tg suggests its better sensitivity in postoperative monitoring, and preoperative measurements of Tg and TgAb baseline values can theoretically assess the reliability of Tg and TgAb tests in postoperative assessment. Trumboli et al.5conducted a largesample analysis on serum Tg levels in patients with thyroid nodules and indicated that the preoperative serum Tg level can be taken as an index for assessment of the initial clinical state of thyroid cancer and should be routinely tested before operation. The expert group recommends that a simultaneous test of Tg and TgAb levels should be conducted for an assessment of the initial clinical state and serological index baseline.

Table 1 Categories of recommendations

Table 2 Recommendations
Marker measurements in washout fluid from preoperative fine needle aspiration (FNA) of lymph nodes of DTC
Recommendation 4: If suspected metastatic lymph nodes are observed in preoperative neck examination of DTC,measurement of Tg level in FNA washout fluid can be optionally used as an auxiliary method to evaluate metastatic lymph nodes (grade of recommendation: B).
Cervical lymph node metastasis is commonly observed in DTC. Ultrasonography and CT are commonly used to assess the cervical lymph node metastasis, but they have limitations.For a few suspicious metastatic lymph nodes undetermined in imaging examination, ultrasound-guided FNA pathology diagnosis and/or Tg measurement in washout fluid can be used as auxiliary diagnostic methods6-7. If the evidence for assessment of lymph node cytology is insufficient or if the cytological findings are not in consensus with the imaging findings, measurement of Tg values in washout fluid must be performed. A study showed that the sensitivity, specificity,and accuracy of FNA combined with Tg measurement in washout fluid were 87.0%, 100%, and 92.2%, respectively8-10.Therefore, the measurement of Tg value in FNA washout fluid can be used as an auxiliary method to determine the lymphatic metastasis. However, a minority of false-positive results may occur, particularly during evaluation of central compartment lymph nodes in the presence of thyroid11-12.
As normal saline does not contain Tg and is the most commonly used solution in clinical practice, puncture needles must be washed with normal saline and dilute into washout fluid. A study showed that the FNA-Tg levels in serum separation tubes (pro-coagulation tubes) and heparin anti-coagulation tubes significantly decreased compared with those in common serum tubes. Therefore, a common serum tube is recommended to be used in the collection of FNA washout fluid. The requirements for lymph node FNA-Tg detection reagents are in accordance with those for serum Tg detection reagent. Meanwhile, reagents with high sensitivity shall be used to ensure that the little amount of Tg in washout fluid can be detected.
Serological test in DTC postoperative assessment and follow-up
Recommendation 5: Tg and TgAb should be routinely tested after total thyroidectomy of DTC, using the same manufacturer’s reagents, and should be evaluated serially over time at various time points during follow-up for continuous assessment of postoperative recurrence risk and treatment response (grade of recommendation: A).
Serum Tg can be a tumor maker of DTC after total thyroidectomy (particularly after the treatment with radioactive iodine ablation), and its level has a positive correlation with tumor burden in DTC patients, which can be used as a clinical marker for assessment of tumor recurrence and metastasis. However, as the serological Tg test is affected by TgAb level in the body, clinical studies in different populations and with test assays showed that positive TgAb can be found in 25%–30% of DTC patients in the first diagnosis13. To accurately evaluate, TgAb shall be routinely measured along with serum Tg. The fist measurement shall be generally conducted within 3–4 weeks after operation or ablation, and the expert group recommends to continuously measure Tg and TgAb for assessment of postoperative recurrence risk and treatment response based on the trend in changing values.
DTC treatment responses are as follows: 1) excellent response: no disease-related evidence, including no clinical and biochemical indexes or structural-related evidence; 2)biochemical incomplete response: continuous elevation of serum Tg or TgAb, without evidence of local lesion; 3)structural incomplete response: continuous or new local/distant metastasis; 4) indeterminate response: no specific biochemical or structural abnormality or unable to confirm whether the lesion is benign or malignant. Patients may have stable or decreased TgAb value, without relevant evidence to prove the existence of the lesion.
Recurrence risk of DTC and disease-related mortality can change at any time under the impact of clinical disease course and treatment response. Therefore, the initial recurrence risk stratification cannot remain stubbornly unchanged and shall be continuously amended during follow-up14. See Tables 3 and 4 for the summary for dynamic risk stratification with total thyroidectomy15.
Recommendation 6: Unstimulated Tg and TgAb test results can be taken as the baseline values for treatment response assessment after thyroid lobectomy of DTC, and further examination shall be performed to confirm whether there is recurrence and metastasis if Tg level continuously elevates (grade of recommendation: B).
After thyroid lobectomy of DTC, accurately assessing the cutoff value of serum Tg level for treatment response has no clear definition. However, the results of unstimulated serum Tg test performed 1 month after operation can be considered as the baseline Tg value for long-term follow-up anddynamic risk assessment of patients according to the present available data16,17. For patients with continuous elevation in unstimulated serum Tg level, clinically visible lesions mostly exist, and further imaging examination is recommended to confirm lesions18. A stable or declined unstimulated serum Tg value is a good predictive index for “disease-free status”with a predicating accuracy up to above 80%19. See Table 5 for the dynamic risk stratification with thyroid lobectomy of DTC15.
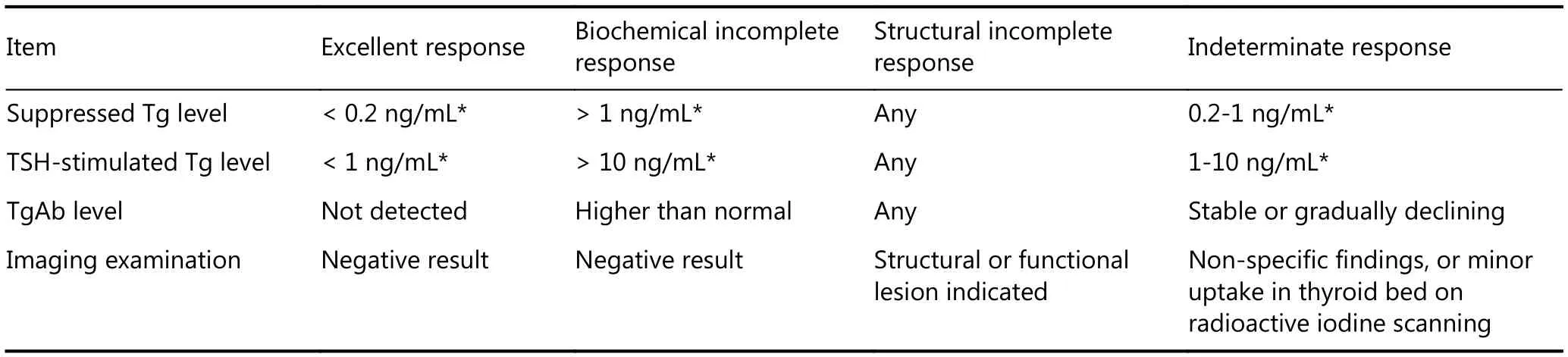
Table 3 Dynamic risk stratification in DTC patients with total thyroidectomy and radioiodine remnant ablation15
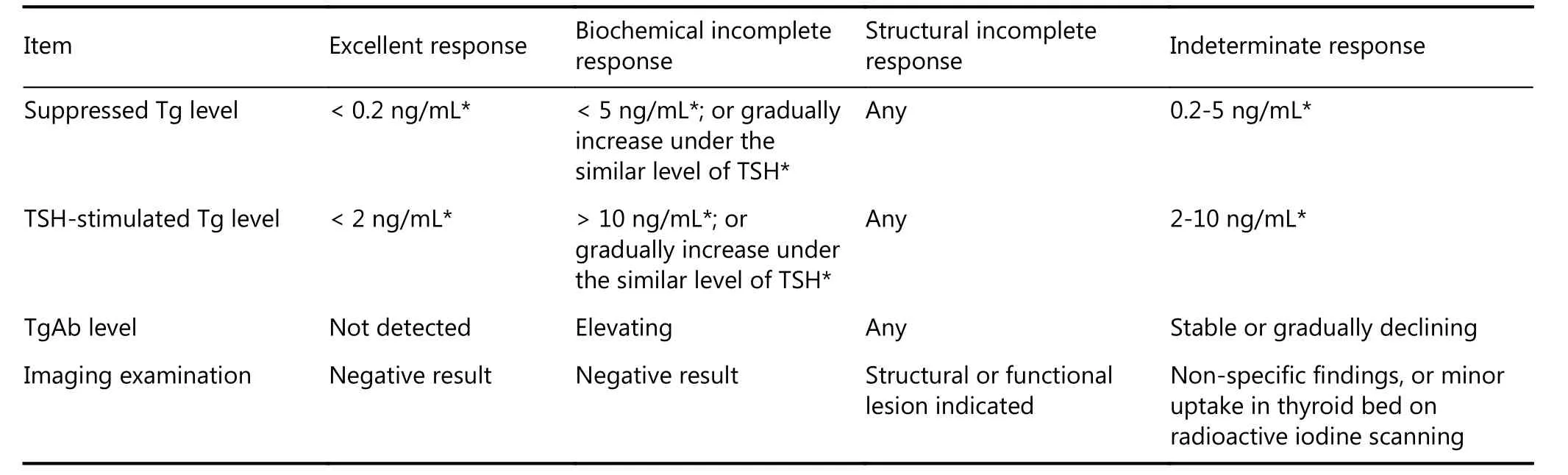
Table 4 Dynamic risk stratification in DTC patients with total thyroidectomy only15
Along with the update on Tg detection reagents20, the detection sensitivity, and sensitivity and precision in low concentration range of highly sensitive Tg (functional sensitivity less than 0.1 ng/mL) have greatly improved. With the emergence of highly sensitive Tg test, the “TSH-stimulated Tg level” might no longer be used for routine assessment of “excellent response” in DTC patients who underwent total thyroidectomy. Suppressed Tg level test is effective in monitoring the postoperative remission of diseases16.
Recommendation 7: It is recommended to frequently measure serum Tg and TgAb after surgery and assess the dynamic risk stratification to guide the adjustment of DTC follow-up scheme and treatment decisions (grade of recommendation: A).
After total thyroidectomy, Tg level in most patients with DTC reaches the lowest concentration 1 month after operation20-21. As the postoperative early assessment indexes and important predictive factors, serum Tg and TgAb values can be used to guide the selection of clinical treatment regimen. The major guidance is listed below:
1) Excellent response: The follow-up intensity and frequency shall be decreased, and the goal of TSH suppressive treatment shall be broadened (lower limit of normal: 2.0 mU/L). Definition of low-risk patients with treatment of total thyroidectomy is to have a postoperative stimulated or suppressed Tg of less than 1 ng/mL, whose prognosis is reliable. Intermediate-risk patients are to have postoperative Tg of less than 1 ng/mL, whose prognosis is reliable with a possibility of micrometastasis. For low-risk and intermediaterisk patients without radioactive iodine treatment,postoperative unstimulated Tg of less than 1 ng/mL indicates favorable treatment response, and the recurrence risk is less than 1%22.
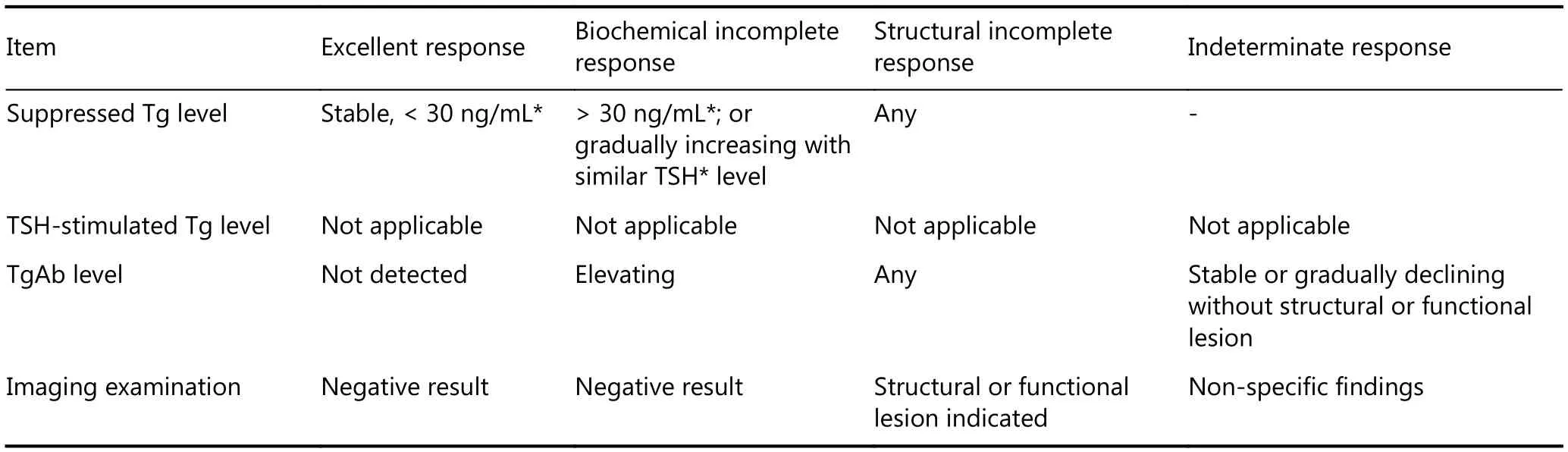
Table 5 Dynamic risk stratification in DTC patients with thyroid lobectomy only15
2) Biochemical incomplete response: If Tg value is stable or gradually declining, most patients can be continuously observed on the premise of constant TSH suppressive treatment (lower limit of normal: 0.1 mU/L), and it is not recommended to immediately perform exploratory/preventive operation or radioactive iodine treatment. An elevated Tg or TgAb level is associated with risk for recurrence; because of this, the follow-up frequency might increase, other examinations might be conducted, or other possible treatments might be given. After total thyroidectomy, suppressed or stimulated Tg of 5–10 ng/mL23-26indicates a higher probability of positive imaging on radioactive iodine scan and confirmation of local or distant metastasis. If postoperative Tg is more than 10 ng/mL, other assessments and treatments are probably required. However, Tg may also be very low or undetectable once the tumor becomes undifferentiated or dedifferentiated.
3) Structural incomplete response: Imaging examination shows that the diseases persistently exist or recur with Tg of more than 10–30 ng/mL after total thyroidectomy, which mostly occurs in patients with failed initial ablation who have local or distant metastasis. Incomplete structure response can cause an increase in mortality27-28. Therefore,multidisciplinary diagnosis and treatment shall be recommended.
4) Indeterminate response: The goal of TSH suppressive treatment is slightly broadened (lower limit of normal: 1.0 mU/L), and treatment response classification can be reassessed based on the results of imaging examinations and serum Tg/TgAb tests. The initial examination frequency of imaging and serum Tg/TgAb is 1–2 times per year, and the interval can be appropriately prolonged if the condition is stable.
Recommendation 8: For DTC patients with positive TgAb, postoperative disease states shall be continuously assessed by measuring the variation tendency of serum TgAb levels (grade of recommendation: C).
Positive TgAb on immunological detection usually means that serum TgAb value is greater than the upper limit of normal reference range of population. However, for postoperative patients with DTC, some scholars think that it is more appropriate to select the lower limit of detection of TgAb as the positive cutoff value of interfering TgAb29-30. For DTC patients who are TgAb positive preoperatively, TgAb value must be monitored during follow-up. As a surrogate indicator, the trend of TgAb is more important than the numerical value. Decreasing serum TgAb level indicates that the disease remits. Conversely, disease recurrence shall be suspected with a continuous increase in serum TgAb levels.Patients with stable serum TgAb shall be diagnosed as indetermination. For follow-up recommendations on DTC patients with positive TgAb after total thyroidectomy, see Figure 130.
MTC
Postoperative serological test and assessment of MTC
Recommendation 9: For patients suspected of malignant thyroid tumor, serum Ctn shall be routinely tested before operation to identify and screen for MTC. For patients with elevated Ctn or considered for MTC, CEA shall also be tested (grade of recommendation: B).
A series of prospective non-randomized studies have assessed the utility of Ctn and proved that routine serum Ctn screening can discover early C-cell hyperplasia and MTC, so as to improve the detectable rate and overall survival rate of MTC31-35. The American Thyroid Association maintains a neutral attitude to Ctn screening28but still accepts that Ctn screening is of significant value in some patient subgroups.The consensus recommends that preoperative Ctn test should be routinely performed on patients suspected of having malignant thyroid tumor.
Meanwhile, the expert group suggests that basal values of serum Ctn and CEA should be simultaneously tested if MTC is considered clinically. The serum Ctn value in a few MTC patients may be in normal range, and significant elevation in serum CEA but relative reduction in Ctn may occur in some patients with advanced MTC; some scholars think that patients with poorly differentiated MTC may either have normal serum Ctn and CEA levels or experience a simultaneous decline in serum Ctn and CEA levels36.Therefore, for judgment and assessment of MTC, clinicians should fully analyze the clinical and pathological results in addition to serum Ctn and CEA as reference.
Recommendation 10: Elevated serum Ctn value can reflect tumor burden in patients with MTC and can be taken as a strong evidence to guide clinical assessment of MTC (grade of recommendation: A).

Figure 1 Treatment and follow-up flow chart of patients with differentiated thyroid cancer who have positive TgAb WBS: whole body scintiscanning; LT4: levothyroxine; TSH: thyroid stimulating hormone; FT3: free triiodothyronine; FT4: free thyroxine; TgAb: antithyroglobulin antibody; Tg: thyroglobulin; dxWBS: whole body imaging of diagnostic radioactive iodine; PET/CT: positron emission tomography/computed X-ray tomography.
MTC is characterized by high malignancy, commonly with lymph node metastasis and distant metastasis. Primary and metastatic tumor burden of MTC co-determine and is positively correlated with serum Ctn level. Clinicians can perform a clinical assessment of MTC based on the level of serum Ctn. A study showed that the risk of lymph node metastasis increased when serum Ctn value is more than 20 pg/mL, and the possibility of distant metastasis increased when serum Ctn value is more than 500 pg/mL37. For patients with preoperative serum Ctn value less than 10 pg/mL, “biochemical cure” can be achieved after treatment with complete lymphadenectomy, and postoperative 10-year survival rate is 97.7%38.
Recommendation 11: Patients diagnosed with MTC shall be mainly treated with total thyroidectomy, and cervical lymph node metastasis and extent of dissection shall be preliminarily evaluated using imaging studies and serum Ctn value (grade of recommendation: B).
The incidence of lymph node metastasis in MTC patients is high, about 70%–90%, and the lymph node metastasis’behavior is associated with the size and location of primary tumor39,40. Necessary lymph node dissection is required during initial thyroidectomy, and comprehensive assessment shall be conducted on the probability of cervical lymph node metastasis based on the location and size of primary MTC lesion and serum Ctn values. Imaging studies are routine methods employed to assess whether the lymph nodes have metastasis, and preoperative serum Ctn values can also effectively assist in determining the extent of lymph node metastasis. Previous studies showed41,42that it is generally indicated that suspicious lymph nodes had metastasized to the ipsilateral central zone and ipsilateral lateral neck zone,contralateral central zone, and contralateral lateral neck zone and superior mediastinum zone when the serum Ctn values are more than 50, 200, and 500 pg/mL, respectively.
Recommendation 12: For carriers with hereditary MTC(HMTC) family mutation gene, serum Ctn can be monitored regularly from infancy, which helps discover the changes in disease status early and determine whether operative treatment shall be performed discretionarily according to the patient’s condition (grade of recommendation: B).
At present, it is recommended in all guidelines at home and abroad that the carriers with HMTC family mutation genes should undergo total thyroidectomy. Due to limited knowledge, most of patients’ family members in China refuse to undergo preventive surgery, while the clinicians shall fully inform them of the serious condition, closely monitor with imaging, and follow up the changes in Ctn.
In principle, for patients with asymptomatic multiple endocrine neoplasia 2A and familial MTC above 5 years old,and patients with asymptomatic multiple endocrine neoplasia 2B above 1 year old, thorough operative treatment shall be carried out if basal serum Ctn value is more than 40 pg/mL. For adolescent HMTC patients with RET mutation genes and serum Ctn less than 30 pg/mL, preventive thyroidectomy shall be carried out. For patients with serum Ctn value higher than threshold value (10 pg/mL), close follow-up will be the best choice, and preventive thyroidectomy can also be considered43-44. It must be carefully decided whether young infants should undergo surgery or not because they can have elevated serum calcitonin levels and yet still normal for their age group45.
Intraoperative serological test in MTC
Recommendation 13: For patients with MTC, it is not recommended to test serum Ctn and CEA during operation to assess the thoroughness of excision (grade of recommendation: F).
Ctn and parathyroid hormone (PTH) co-participate in the regulation of calcium in the body and maintain stability of calcium metabolism. The half-life of Ctn is more than 1 h,mainly undergoing degradation and excretion from the kidney. However, the half-life of its precursor serum procalcitonin in human body is about 20–24 hours with good stability, continuously forming calcitonin. For patients with high level of preoperative Ctn, the intraoperative Ctn value after tumor resection cannot immediately reflect the thoroughness of operative excision. Similarly, serum CEA is mainly eliminated by Kupffer cells and liver cells with a halflife of 1–7 days. However, depending on liver function, the half-life of serum CEA is prolonged in cholestasis and hepatocellular diseases. Therefore, it is not recommended to routinely test serum Ctn and CEA levels after tumor resection during operation.
Serology-assisted postoperative management of MTC
Recommendation 14: Ctn and CEA levels can be considered as important monitoring indexes of postoperative management and prognostic prediction of MTC (grade of recommendation: A).
Postoperative serum Ctn test can be used to assess the effect of operative treatment in MTC patients, and the normalization of postoperative serum Ctn usually indicates favorable outcome. A previous study showed that serum Ctn value would be even lower than the lower limit of detection after total resection of thyroid tissues46. In view of half-life of Ctn, regarding its metabolism and other factors, it is generally suggested that the optimal time for test of postoperative Ctn minimum value be 3 months after the operation47. However, considering the different tumor burden in various patients, the test time of postoperative serum Ctn and CEA can be 1 week, 1 month, 3 months, and half a year. Regular postoperative re-examination shall be carried out if test values are less than the lower limit of detection or the normal reference range. Initial reexamination period is half a year and can be gradually prolonged to once per year if the condition is stable.
A study of postoperative long-term observation and follow-up of MTC demonstrated that48the 3-year and 5-year survival rates were 94% and 90%, respectively, if postoperative serum Ctn value was less than 10 pg/mL.Moreover, the 3-year and 5-year survival rates were reduced to 78% and 61%, respectively, if postoperative serum Ctn value was more than 10 pg/mL. If patients exhibit abnormal postoperative basal serum Ctn values after total thyroidectomy, this might indicate the presence of residual lymph nodes or lesions, or that recurrence risk may exist,even if serum Ctn value is less than 150 pg/mL. Therefore,the expert group recommends that neck ultrasound examination shall be performed if postoperative serum Ctn level increases but is less than 150 pg/mL, and Ctn, CEA, and neck ultrasound shall be repeated semiannually for monitoring if test results are negative. If postoperative serum Ctn value is more than 150 pg/mL, neck ultrasound, chest and abdomen CT/MRI, and whole body bone examination must be carried out, and PET/CT examination should be performed when necessary, in order to discover the lesions early.
Prospect
Continuous exploration of new methods and new markers for laboratory diagnosis of thyroid cancer: We hope that more molecular makers are used for diagnosis, prognosis assessment, and confirmation of therapeutic targets.
How to use Tg to assess the treatment response in patients without total thyroidectomy: For patients without total thyroidectomy, serum Tg level is greatly affected and assessment of treatment response cannot entirely rely on it,and new markers or new methods might be used for followup in patients who did not undergo total thyroidectomy.
Exploration of serum Ctn value in evaluating efficacy of targeted drug treatment of MTC: Serum Ctn levels in MTC patients can greatly reduce after receiving some drug therapies, while those declines have no significant correlation with the changes in tumor size and regression; hence, further studies are needed to verify the feasibility of using serum Ctn as a reliable index for drug effect assessment.
Exploration of optimum clinical cutoff value of serum markers of thyroid cancer to achieve the optimal clinical specificity and sensitivity: Along with the continuous development of test methodology, the accuracy of reagents constantly improves, and more studies are needed to find the optimal cutoff value and apply that to clinical practice in future, so as to enhance the predictive value in the assessment of tumor stage and tumor recurrence.
Acknowledgements
This article was published originally in Chinese Journal of Clinical Oncology 2017; 48: 7-13 (in Chinese).
Conflict of interest statement
No potential conflicts of interest are disclosed.
 Cancer Biology & Medicine2018年4期
Cancer Biology & Medicine2018年4期
- Cancer Biology & Medicine的其它文章
- Multidisciplinary team for the diagnosis and treatment of 2 cases of primary intestinal yolk sac tumor
- Comparison of sentinel lymph node detection performances using blue dye in conjunction with indocyanine green or radioisotope in breast cancer patients: a prospective singlecenter randomized study
- Prognostic factors of refractory NSCLC patients receiving anlotinib hydrochloride as the third- or further-line treatment
- PD-L1 expression and its effect on clinical outcomes of EGFR-mutant NSCLC patients treated with EGFR-TKIs
- Five-CpG-based prognostic signature for predicting survival in hepatocellular carcinoma patients
- A new tumor-associated antigen prognostic scoring system for spontaneous ruptured hepatocellular carcinoma after partial hepatectomy
