Family functioning integrated with diabetes self-management: a concept analysis
Rin Ai Pmungks*, Knitth Chmroonswsi, Prnee Vtnsomboon
aDepartment of Family Health, Mahidol University, Bangkok 10400, Thailand
bDepartment of Nursing, College of Health, Bina Generasi, Polewali 91315, Indonesia
cDepartment of Nursing, College of Health, Marendeng Majene 91411, Indonesia
dDepartment of Health Education and Behavioral Science, Mahidol University, Bangkok 10400, Thailand
Abstract: Although the concept of family functioning has gained recent popularity, the terms “family functioning” and “family resilience” are sometimes confused and used interchangeably. The aim of this concept analysis was to clarify what is meant by family functioning in the context of diabetes self-management by assessing specific attributes, antecedents, and consequences. A concept analysis model by Walker and Avant was applied. The identified attributes of family functioning in a diabetes self-management context included problem-solving, communication, roles, affective responsiveness, affective involvement, and behavioral control. Antecedents included family structure, socioeconomic status, family functioning relationships, family stage, and life events. Consequences included family satisfaction, family cohesion, and family relationships. This analysis provided a deeper understanding of a family functioning concept within a diabetes self-management context. It is recommended that health care providers should be aware of antecedent factors that could inhibit outcome improvement. Further research is needed to explain family functioning attributes in relation to antecedents and potential consequences.
Keywords: family functioning · concept analysis · diabetes · self-management
1. Introduction
Diabetes mellitus (DM) is a significant public health problem worldwide. The World Health Organization(WHO) predicts that 422 million people are currently living with DM.1Several complications are associated with DM, including diabetic retinopathy, nephropathy,neuropathy, cardiovascular disease, amputations, and premature death.2
Diabetes self-management is relatively complex given that individuals have to attend medical appointments regularly, adhere to several different medications,control their symptoms through physical activity, blood glucose monitoring, and foot care, and negotiate barriers to management and psychosocial problems.3
Family members are a potentially useful support system for diabetes self-management. Much diabetes management takes place within a close social environment.4Therefore, addressing family functioning within diabetes self-management is important, as disease management is mostly facilitated within a family context. However, family functioning contexts are currently unclear and difficult to differentiate from family resilience when a chronic illness is present.5
The terms “family functioning” and “family resilience” are sometimes confused and used interchangeably; this is because both terms are related to a family’s adaptation and dynamic processes when confronted with stress emanating from a chronic illness. A better understanding of family functioning could clarify ways to help the family and patient maintain balance and functioning when providing diabetes care.Conceptualizing family functioning with regard to diabetes care provides an essential foundation for developing effective and sensitive interventions that promote growth among individual family members and the family unit as a whole.
Concept analyses provide precise operational definitions, refine ambiguous concepts within a theory, and provide a more basic and deeper understanding of underlying attributes within a concept. Eight steps, first identified by Walker and Avant, are conducted: (a) select a concept, (b) determine the purpose of the analysis,(c) identify all uses of the concept, (d) determine the defining attributes, (e) construct a model case,(f) identify antecedents, (g) identify consequences, and(h) define empirical referents.6
2. Methods
This initial review included articles that shared relevance with a standard literature review. For initial strategies,“family functioning,” “self-management,” and “type 2 diabetes” (T2DM) were the main search terms, and these terms needed to be observed either in the abstract or in the title of the study.
2.1. Eligibility criteria
To describe family functioning within diabetes selfmanagement among T2DM patients, the researchers used the following article inclusion criteria. Specifically,descriptive articles of how a family integrated with diabetes self-management were included. Design types included descriptive studies, qualitative studies, and intervention studies that focused on diabetes prevention and diabetes self-management.
2.2. Search strategy
The researcher used PubMed, Scopus, and Google Scholar to find the relevant articles related to family functioning integrated with diabetes self-management for T2DM patients. The search strategy used in this review included “family functioning,” “self-management,”and “type 2 diabetes.”
2.3. Synthesis of results
Results of this review are explained narratively. The descriptions of results include the following: (1) definition of family functioning; (2) defining attributes of family functioning integrated with diabetes self-management;(3) model case on applying family functioning integrated with diabetes self-management, antecedents, consequences, and empirical referents.
At first Mustapha refused, saying that he had been blindfolded22; but when the robber gave him another piece of gold he began to think he might remember the turnings if blindfolded as before
3. Defining family functioning
Family functioning is defined as the process by which the family system completes a series of tasks, including basic tasks (e.g., managing individual needs such as food and clothing living line, and money management),developmental tasks (e.g., adapting and promoting the growth and development of members), and crisis tasks(e.g., dealing with all kinds of family emergencies).7
4. Defining attributes
Attributes are defined as characteristics that appear repeatedly with reference to the concept. These defining attributes assist the researcher in differentiating similar concept definitions.6Defined attributes were as follows: (a) problem-solving, (b) communication, (c) roles,(d) affective responsiveness, (d) affective involvement,and (e) behavioral control (Table 1).
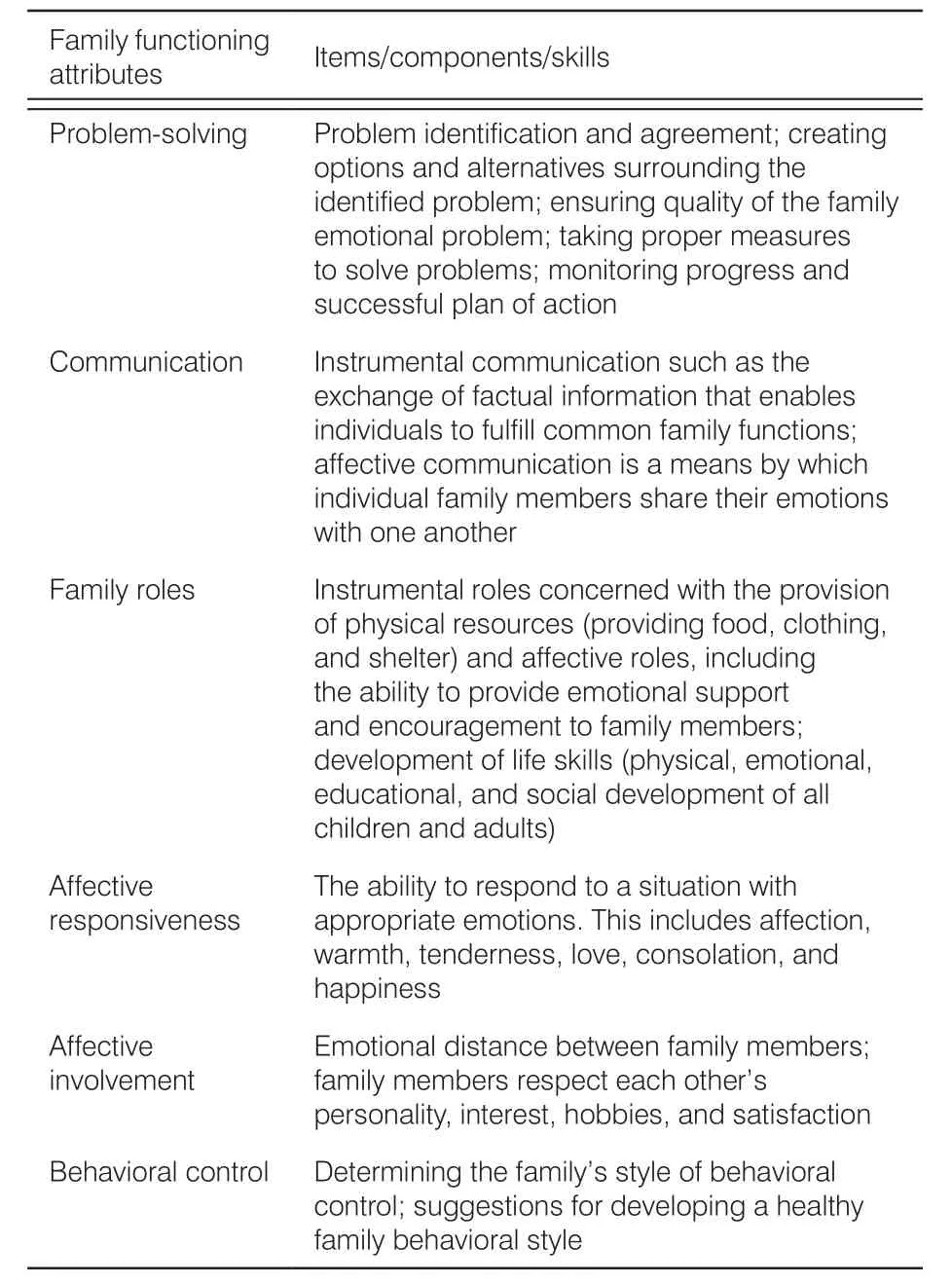
Table 1. Family functioning items, components, and skills.
4.1. Problem-solving
Problem-solving can be defined as the family’s capacity to solve problems to maintain effective family functioning. This is similar to notions of finding a solution to avoid threatening the integrity and functioning of the family’s capacity.8The family members who successfully resolve problems are capable of dealing with both instrumental and emotional issues. In a diabetes context, problem-solving skills are required to manage behavioral issues, including how to manage a healthy diet, increase physical activity, and monitor blood glucose and psychological problems (e.g., feelings of denial, negative responses to diabetes selfmanagement, and depression).9-11Problem-solving also requires addressing whether an intervention is of sufficient potency and intensity in terms of treatment dose and duration for effective self-management.12Family members emphasize effective feedback concerning negative perceptions to reduce care resistance and build a patient’s self-efficacy.13
4.2. Communication
Communication is defined as the process by which information is exchanged within a family. Family members need to communicate and coordinate to address thought and feeling patterns that emerge during diabetes care.14Within the communication concept, emotional expressions could promote the role of family members in helping the patient with problem-solving and supporting self-management.15
With regard to diabetes care, open and supportive communication among patients and family members is important.16For instance, patients often express a willingness to educate family members regarding increased T2DM risk and primary prevention.17Communication also influences emotional support and the ability to obtain valuable information and increase family cohesion.18This is performed to manage diabetes behaviors, promote effective day-to-day coping, reduce care resistance, and enhance self-efficacy.13One study suggested that augmenting communication skills during diabetes management helps with problem-solving and behavior change to achieve goals relevant to tailored interventions. Overall, this can improve communication skills during discussion tasks, goal setting, and problem-solving.19
4.3. Roles
Roles are patterns underlying a family’s behavior which are established by family members to complete effective functioning.20To achieve the certain social and family expectations in DMSM practice, patients themselves and their family members should fulfil those roles. In this article, the family role is subdivided into instrumental and affective types. Instrumental roles include money management or deciding on diabetes treatment. Affective roles focus on the feelings and emotional experiences related to implementing diabetes self-management. Family member roles include facilitating, accommodating, reminding, and motivating patients to complete self-management tasks, help with decision-making and problem-solving, connect to outside resources, provide emotional support, and facilitate patient–provider communication.21
4.4. Affective responsiveness
Affective responsiveness can be defined as family members’ ability to respond to outside stimuli with appropriate feelings. This could facilitate various aspects related to task accomplishment and successful role integration.15
Being able to positively respond to other family members with a wide range of emotions is key to successful family functioning. Specific family members are some of the best sources of support for diabetes self-management. To respond with appropriate emotions, several affective responsiveness skills are needed, and they include the following:staying tuned to what is going on in the lives of other family members, being empathic within a given situation, appropriately control and express anger, and verbally express love and appreciation for other family members as well as joy in other members’accomplishments.14
4.5. Affective involvement
Affective involvement is the degree of concern and attention that family members give to activities among each other. This could help or hinder task accomplishment within the family20and influence the ability of a family member to meet emotional barriers and security needs as well as the flexibility to provide support.15
One study conducted with elderly patients whose spouses were involved with care observed positive effects regarding adherence to diabetes management,higher self-esteem, enhanced ability to address barriers,and the development of supportive relationships among family members as compared with those patients lacking such support.22
However, some conflicts often occur within the family since lifestyle changes are required for optimal diabetes self-management.23Family members also can disrupt or undercut self-care efforts (e.g., planning healthy meals or question medication adherence).24Therefore, diabetes self-management should focus on the family as an intervention target to better equip the family with the ability to provide support and care.25
4.6. Behavioral control
Behavioral control is key to successful family functioning; it is often defined as the pattern a family adopts for handling specific behaviors.20In this process, the family members should be capable of maintaining ongoing functioning as well as should adapt to shifting task demands. Family behaviors are important for patients with T2DM which require consistent and active selfmanagement. This often involves changes to daily routines, including changes in eating patterns, physical activity, and regular self-testing for blood glucose,cholesterol, blood pressure, etc.26Family system theory emphasizes positive family functioning influencing individual functioning by facilitating interconnectedness for managing diabetes.27
One study reported that families who are able to adapt to specific situations are better able to solve problems. Thus, a flexible behavioral control style could improve a family’s ability to overcome challenges through a family contract system.14Hence, families can identify interests and concerns that may need to be changed, including family-style behaviors.
5. Model case
Walker and Avant described a model case that demonstrates “all defining attributes of the concept.” The example case is provided as follows:
A 60-year-old man with a 6-year history of type 2 diabetes mellitus. Although he was diagnosed in 2011,he had symptoms 3 years before diagnosis. The HbA1c records indicated values of 8%, which was categorized as poor glycemic control. He had poor eating habits and was not exercising. He really loved to eat large pastas and sweet foods. At the time of initial diagnosis, he was advised to lose weight, but no further action was taken.Referred by his family physician, he was required to decrease his weight and control his blood glucose. He has been trying to lose weight and increase his exercise for the past 6 months without success. He started with glyburide, 2.5 mg, every morning but had stopped taking it because of dizziness, often accompanied by sweating and a feeling of mild agitation. He stopped these supplements when he did not see any positive results. He does not test his blood glucose levels at home and expresses doubt that this procedure would help him improve his diabetes control. The patient was required to do multiple tasks for self-management, including attending a regular medical appointment each month, adhere to medication regimens, and engage in self-care behaviors (i.e.,at-home blood glucose monitoring, control his diet, and increase physical activity). However, it is often difficult for him to consistently engage in these health behaviors that are necessary for good glycemic control. Common barriers include competing daily demands, frustration,other emotional distress, low self-commitment, lack of knowledge, low levels of self-efficacy to successfully complete an activity, and insufficient social support from family members. To change and maintain positive selfmanagement behaviors, family members were tasked with helping the patient with strategic planning and goal setting. Effective feedback concerning negative diabetes perceptions and good communication was also used for exchanging health information, reducing care resistance, and building self-efficacy emphasized by family members. Additionally, during diabetes treatment, family members emphasized cultural beliefs and values to help support dietary change, physical activity, and blood glucose monitoring. This was done in order to help the patient feel appreciated. Regarding emotional supportive behaviors, family members assessed psychosocial problems. A patient can express negative responses to diabetes self-management, a seasonal mood disorder,and/or the presence of depression due to the illness or retirement during treatment. However, family members are on his side in order to provide emotional support,as well as help with problem-solving. This strategy can boost adherence to medication regimens, encourage a healthy diet, and maintain exercise behaviors. The patient-family relationship, cohesion, and patient-family member communication were achieved.
This model case illustrates successful achievement of all family functioning attributes for effective diabetes self-management. This model also provides information regarding family functioning and means for supporting patients with specific self-management tasks, such as healthy eating habits, selecting appropriate physical activity, blood glucose monitoring, foot care, and stress management. Effective feedback and exchanging health information reflect good communication, emphasizing cultural beliefs and values for generating supportive behaviors as part of family functioning. This includes affective involvement, emotional support, and instrumental support for diabetes care. Outcomes include effective responses from family members, and problemsolving was emphasized when the patient showed negative responses to self-management, depression, and retirement during long-term treatment. From this model case, it is understood that effectiveness of family functioning could influence relationship roles, family cohesion, and family communication for managing patients’behavior.
6. Antecedents
Walker and Avant defined antecedents as events that must occur prior to the emerging concept. The factors considered as antecedents for implementing family functioning for supporting care include family structure,socioeconomic status, family functioning relationships,family stage, and life events that could impact outcomes.7Managing these factors could influence basic family functioning to provide appropriate environmental conditions for members to complete a series of tasks,including basic tasks (e.g., managing the material needs of the individual such as food and clothing living line),developmental tasks (e.g., adapting and promoting the growth and development of each member), and crisis tasks (e.g., dealing with all kinds of family emergencies).8
The review also revealed relationships between the highest levels of family functioning styles with family values and resource mobilization for patients with T2DM.28Other factors influencing family functioning include parental age, socioeconomic level,29educational attainment, and sibling relationships.30In addition, higher income was positively correlated with better physical and mental health, greater longevity, fewer stressful life events, and greater successes.29,31
7. Consequences
Walker and Avant defined consequences as events that occur as a result of the emerging concept. Consequences of family functioning have been demonstrated by research related to diabetes management. Family functioning significantly influences a sense of satisfaction and family cohesion.32In addition, family functioning is positively affected by diabetes management, illustrating the protective nature of a positive family environment in relation to achieving the most favorable health outcomes.33At this point, family functioning may be very helpful in moving the family toward a better level of diabetic control. It is generally accepted that a lack of family functioning leads to declines in diabetic control and can even negatively affect a child’s functioning in areas such as personality, physical well-being, and activity participation.34
8. Empirical referents
Empirical referents are defined as classes or categories of actual phenomena that, by their existence or presence, demonstrate the emergence of a concept.Some instruments are identified for measuring family functioning within the area of chronic disease, including the Family Assessment Device (FAD) survey,8Family Functioning Index (FFI),37Family Adaptability,Partnership, Growth, Affection, and Resolve Index(AFGAR),38Family Assessment Measure (FAM),15and the Chinese version of the Survey of Family Environment (SFE).39
Epstein et al.8used a 60-item instrument that listed family functioning to identify families experiencing problems, highlighting specific domains and assessing change following treatment. This instrument had seven categories, including problem-solving, communication, role function, affective responsiveness, affective involvement, behavioral control, and overall functioning.The FAD is composed of four statement responses1-4for each subscale, and the individual scale scores range from 1.0 (best functioning) to 4.0 (worst functioning).This instrument is considered with high internal consistency (Cronbach’s α = 0.74–0.92).
Satterwhite et al.37created the FFI to reflect dynamics within family interactions, an important intervening variable in terms of social and medical outcomes when providing care for a chronic physical disorder. The FFI appears to be a reliable and valid instrument with test–retest correlation scores between 0.74 and 0.83. A total of 15 self-reported dyadic and whole family questions(yes/no on a 5-point rating scale) are grouped into five functions: marital satisfaction, frequency of divergence,communication, problem-solving, happiness, and intimacy.37The scores range from 0.07 to 0.96 for fathers and 2.1 to 0.95 for mothers.
AFGAR is used to assess a family member’s perception of family functioning by examining patient’s satisfaction with family relationships. The measure consists of five family functioning parameters: adaptability,partnership, growth, affection, and resolve. The scale is measured on a 5-point scale ranging from 0 “never” to 4“always.” The largest possible score is 20; a score of £9 is considered dysfunctional; 10–12 is moderate family dysfunction; 13–16 points are mild family dysfunction;and 17–20 points are good functionality. The AFGAR is a reliable instrument with good internal consistency(Cronbach’s α = 0.80–0.85) and item-to-total correlations ranging from 0.50 to 0.65. Initial validity was also established with a correlation of 0.80 (the latter = 0.64).38
Skinner et al.15developed the FAM based on the process model of family functioning. This model described seven key dimensions: task accomplishment, role performance, communication, affective expression, involvement, control, and values and norms. Fourteen items are scored on a 4-point Likert scale ranging from “strongly agree” to “strongly disagree.” The FAM is measured at three levels, including the whole family system (general scale, 50 items), various dyadic relationships (dyadic scale, 42 items), and individual functioning (self-rated scale, 42 items). The FAM appears to be a reliable and valid instrument with coefficient alphas ranging from 0.60 to 0.80. The overall FAM ratings yield substantial alpha coefficients: adults = 0.93 general scale, 0.95 dyadic relationships, 0.89 self-rating; children = 0.94 general scale,0.94 dyadic relationships, and 0.86 self-rating (Table 2).
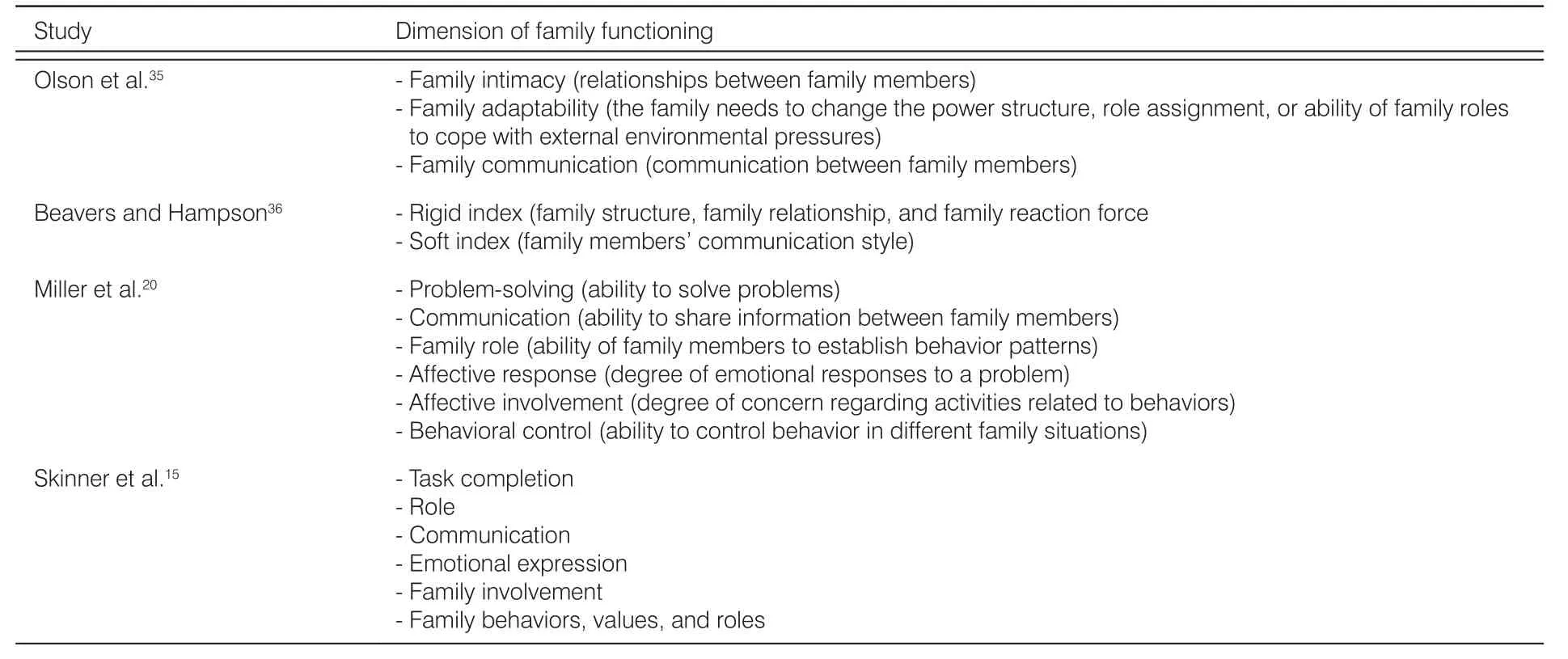
Table 2. Dimensions of family functioning.
The SFE consists of 30 items that examine family functioning and family support needs which consist of 5 structures including supra-system, macro-system,micro-system, family internal environment system, and chrono-system. All items are scored on a 5-point Likert scale (1 = “dissatisfied/unimportant,” 5 = “satisfied/important”) with scores ranging from 1 to 25 points.Internal consistency is high (0.92). In a test–retest study of 33 families, the correlation coefficient was 0.93, indicating the high test–retest reliability. The instrument consists of three dimensions: relationships between family members, relationship between the family and subsystem, and relationship between the family and society.39(Table 3)
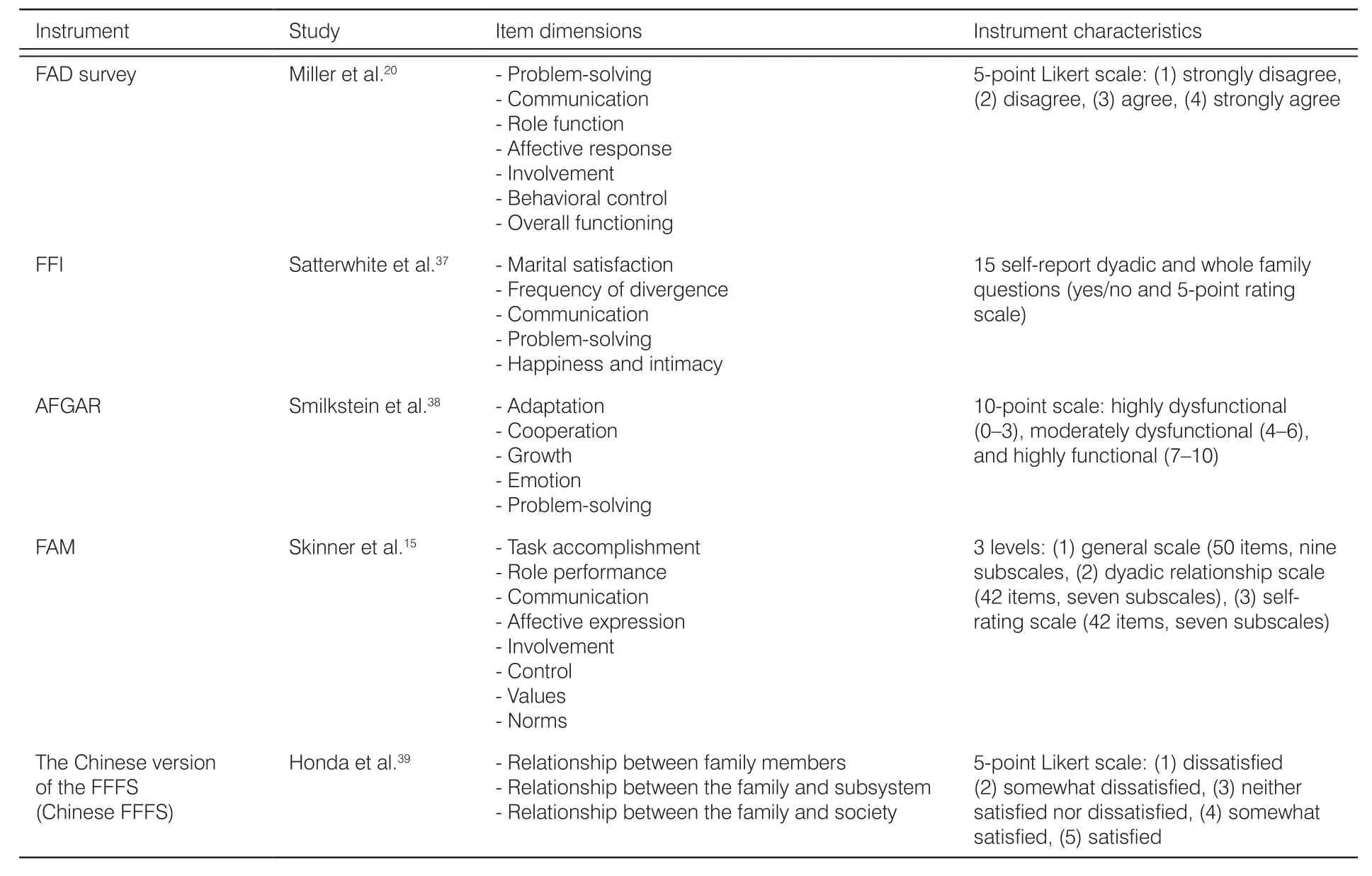
Table 3. Instrument measures for family functioning.
AFGAR, Family Concern Index Questionnaire;FAD, Family Assessment Device; FAM, Family Assessment Measure; FFI, Family Functioning Index; FFFS,Feetham Family Functioning Survey.
The differences between the five instruments are the dimensions measured and settings to which each scale is applied. However, different attributes have been identified in this concept analysis, and unique aspects of the reviewed concept lead to some divergence. Thus, specific instruments could be modified based on the specific family functioning definitions.
9. Conclusions
The main findings suggest a clarification of defining attributes, antecedents, consequences, and empirical referents related to family functioning in diabetes selfmanagement. The concept of family functioning is made up of several dimensions, including problem-solving,communication, family roles, affective responsiveness,affective involvement, and behavioral control. These attributes are associated with factors known to serve as antecedents, including family structure, socioeconomic status, family functioning relationship, family stage, and life events. The goal of better understanding of family functioning is to ultimately improve health outcomes, family satisfaction, family cohesion, and family relationships.Thus, fully elucidating the concept of family functioning in diabetes self-management could improve health outcomes and provide provisions for health care providers to more appropriately engage services among diabetes patients and their family members. Hence, this review recommends that health care providers become aware of, and consider, the antecedents underlying family functioning concepts for promoting positive health outcomes.
Acknowledgments
The authors would like to thank Mahidol University for facilitating the database search necessary for this review. The authors would like to give special thanks also to the Indonesia Endowment Fund for Education(Lembaga Pengelolah Dana Pendidikan [LPDP] scholarship) and Ministry of Higher Education and Research for grant support.
Compliance with ethical standard
The Endowment Fund for Education provided a grant funding for this review (S-3937/LPDP.3/2016). The funding sponsors also had no role in the writing of the manuscript or any decision to publish this manuscript.
Conflicts of interest
All contributing authors declare no conflicts of interest.
- Frontiers of Nursing的其它文章
- Family characteristics on self-reported toothache among Indonesian children aged 12–14 years
- Beneficial effects of auricular acupressure on preventing constipation in breast cancer patients undergoing chemotherapy: evidence from systematic review and meta-analysis
- A systematic review of the effect of mobile health on cardiac rehabilitation among coronary heart disease patients
- Effects of parental involvement in infant care in neonatal intensive care units: a meta-analysis
- Bibliometric analysis of literature regarding ostomy research based on the Web of Science database†
- Peer educator training program for enhancing knowledge on issues in the growth and development of adolescents and risk behavior problems in Indonesian context†