Therapeutic observation of acupuncture plus tuina for cervical vertigo
He Yong-song (何永松), Ma Ling-yun (马凌云)
1 Lujiazui Community Health Service Center of Pudong New Area, Shanghai, Shanghai 200120, China
2 Quyang Hospital of Shanghai, Shanghai 200092, China
Abstract
Keywords: Acupuncture Therapy; Tuina; Massage; Points, Head & Neck; Vertigo; Cervical Spondylosis; Vertebrobasilar Insufficiency
Cervical vertigo (CV) is also known as vertebral artery compression syndrome, posterior cervical sympathetic syndrome, or vertebral insufficiency syndrome[1].Vertigo or dizziness is its major symptom, and it is usually caused by vertebrobasilar insufficiency (VBI)secondary to compression or stimulation to vertebral artery or sympathetic nerve due to cervical intervertebral disc degeneration, hyperosteogeny, tension or spasm of cervical soft tissues, or loss of stability in cervical structure, etc[2].Its clinical manifestations include dizziness, headache, cataplexy and visual dysfunction, coupled with tinnitus, nausea and vomiting[3].Here, dizziness is often associated with the neck movement; cervical imaging test may find hyperosteogeny, intervertebral disc herniation, abnormal cervical curvature or unstable vertebral body[4].The incidence of CV has been accelerating during the recent years.It greatly affects the daily life, health, work and study of the patients.Among those over 40 years old,the incidence was between 3.8% and 17.6%[5].Currently,CV is usually treated with conservative therapies, mainly including acupuncture-moxibustion, tuina, acupotomy,physiotherapy and Chinese medication[6-9].We adopted acupuncture plus tuina to treat CV and took acupuncture alone as the control to compare the therapeutic efficacy.The report is given as follows.
1 Clinical Materials
1.1 Diagnostic criteria
The diagnostic criteria were made based on theCriteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine[10]: with headache, dizziness, tinnitus, hearing loss and blurred vision as the main symptoms; with a history of postural cataplexy, and lateral or backward extension of the neck can aggravate the symptoms; X-ray revealed cervical vertebral degeneration and asymmetrical C1lateral mass; CT examination discovered asymmetrical transverse foramina, with narrowing on one side.
1.2 Inclusion criteria
Conforming to the above diagnostic criteria; aged between 18 and 65 years old; with dizziness as the main symptom and transcranial cerebral Doppler (TCD)showed VBI; participated voluntarily and signed the informed consent form; able to collaborate in clinical data collection.
1.3 Exclusion criteria
Cervical fracture, tuberculosis, tumor or infection;vertigo caused by cardiovascular diseases or endocrine and metabolic disorders; ocular vertigo and aural vertigo; pregnant or breast-feeding women; coupled with severe heart, brain, liver or kidney disease; mental disorders.
1.4 Statistical methods
All data were processed by using SPSS version 18.0.Measurement data which conformed to a normal distribution were expressed as mean ± standard deviation (), and the intra-group comparisons were analyzed by pairedt-test while the between-group comparisons were analyzed by independent two-samplet-test.Between-group comparisons of ranked data were performed by using Kruskal-Wallis test.P<0.05 was taken to indicate statistical significance.
1.5 General data
One hundred CV patients were recruited from the Cervical Spondylosis Department of our hospitals.The patients were allocated to an observation group and an acupuncture group by using the random number table,with 50 cases in each group.There were no dropouts during the whole study.The between-group differences in the data of gender, age and disease duration were statistically insignificant (allP>0.05), indicating the comparability (Table 1).
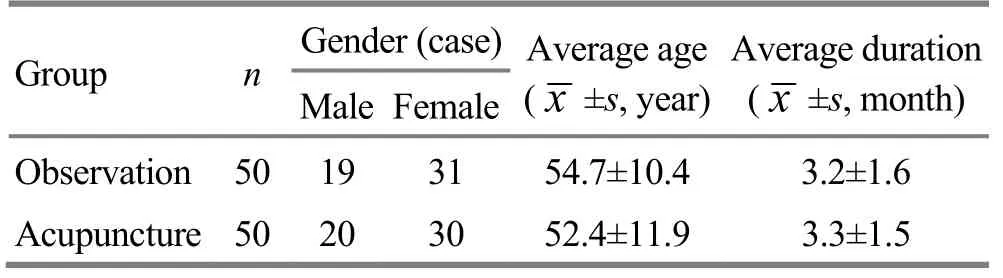
Table 1.Comparison of the general data
2 Treatment Methods
2.1 Acupuncture group
Acupoints: Xiang Ba Zhen (eight acupoints on the nape), i.e.the Ashi points below the spinous process of C2, C4and C6, 2 cun away, Yamen (GV 15) and Dazhui(GV 14).
Method: After standard sterilization, disposable filiform needles of 0.3 mm in diameter and 40 mm in length were used to puncture the Ashi points described as above.The needles were inserted obliquely at 45° for 0.5-0.8 cun with the needle tip reaching the transverse process.Then, Dazhui (GV 14) and Yamen (GV 15) were punctured perpendicularly for 0.5-0.8 cun.When needling qi was achieved, even reinforcing-reducing manipulation was applied.The needles were retained for 20 min, during which TDP infrared lamp was used for the area from Yamen (GV 15) to Dazhui (GV 14), 15 cm away from the skin, and the temperature should be warm-hot and tolerable.The treatment was given once every other day, 10 sessions as a course of treatment,for 1 course in total.
2.2 Observation group
The observation group received the same acupuncture treatment as the acupuncture group,followed by tuina treatment introduced below.
Manipulation for neck-shoulder relaxation: The patient took a sitting position while the doctor was standing next to the patient.First, one-thumb Tui-pushing manipulation was used to relax the neck.Gun-rolling, Na-grasping and Rou-kneading manipulations were then applied to the shoulder and back.Finally, bilateral Jianjing (GB 21) were treated with digital An-pressing with the thumbs, followed by Na-grasping and Tan-plucking manipulations to thoroughly relax the whole back (Figure 1).
Pulling-rotating manipulation of the neck: The patient took a sitting position while the doctor was standing behind with the thumbs pressing Fengchi (GB 20) on each side, the rest fingers and palms supporting the chin, and the two forearms placing on the patient’s shoulder with the ulnar side.The forearms and hands exerted an opposing force to stretch the cervical vertebrae, during which, the neck was also flexed forward, extended backward and turned left and right(Figure 2).

Figure 1.Manipulation for neck-shoulder relaxation

Figure 2.Pulling-rotating manipulation of the neck
Manipulation for the head and face: The patient took a sitting position while the doctor was standing behind.Digital Zhen-vibrating was applied to Baihui (GV 20) for 1 min, followed by digital An-pressing with the thumb,index finger, middle finger and ring finger simultaneously at Sishencong (EX-HN 1) for 30 s.Then,Rou-kneading with the major thenar was applied to Baihui (GV 20) and Sishencong (EX-HN 1) and digital Rou-kneading was used for bilateral Taiyang (EX-HN 5)for 1 min (Figure 3).

Figure 3.Manipulation for head and face
Digital needle-like tuina from Fengchi (GB 20)towards Jingming (BL 1): After the above tuina manipulations, the doctor pressed Fengchi (GB 20) on one side with one thumb and pressed the contralateral Jingming (BL) with the middle finger of the other hand.The two fingers exerted forces simultaneously towards each other and the force and lasting time should depend on whether the patient got a distending, sour and warm feeling in the treated eye.The operation repeated 3 times, which lasted for about 1 min (Figure 4).
Ending manipulation: At the end, the manipulation of Na-grasping the five meridians was performed to relax the head, which was the last step of the treatment(Figure 5).
The tuina treatment lasted for 15 min each session and was performed once every other day, 10 sessions as a course of treatment, for one course in total.
Figure 4.Digital needle-like tuina from Fengchi (GB 20) towards Jingming (BL 1)

Figure 5.Na-grasing the five meridians
3 Therapeutic Observation
3.1 Observation items
The two groups of patients received TCD before and after the treatment to observe the mean velocity (Vm)of bilateral vertebral artery (VA) and basilar artery (BA).
3.2 Criteria of therapeutic efficacy
The criteria of therapeutic efficacy were made by referring to theCriteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine[10].
Cured: Vertigo, headache and neck-shoulder pain were gone.
Improved: Vertigo, headache and neck-shoulder pain showed improvement.
Invalid: Vertigo, headache and neck-shoulder pain showed no improvement.
3.3 Results
3.3.1 Comparison of Vm
There was no significant difference in Vm between the two groups before the treatment (P>0.05).After the treatment, the Vm of VA and BA increased significantly in both groups (allP<0.001), indicating that acupuncture alone and acupuncture plus tuina were both effective for CV; there were significant differences in the Vm of VA and Ba between the two groups after the treatment (bothP<0.05), suggesting that the observation group had a more significant efficacy than the acupuncture group (Table 2).
Table 2.Comparison of Vm (, cm/s)
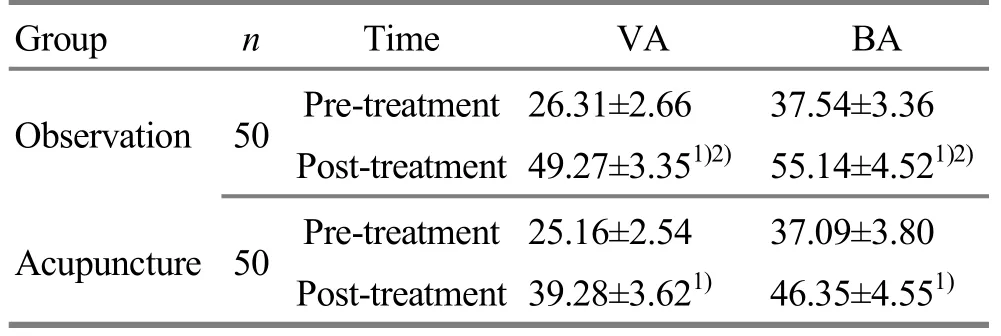
Table 2.Comparison of Vm (, cm/s)
Note: Compared with the same group before the treatment, 1)P<0.001; compared with the acupuncture group after the treatment,2) P<0.05
Group n Time VA BA Observation 50 Pre-treatment 26.31±2.66 37.54±3.36 Post-treatment 49.27±3.351)2) 55.14±4.521)2)Acupuncture 50 Pre-treatment 25.16±2.54 37.09±3.80 Post-treatment 39.28±3.621) 46.35±4.551)
3.3.2 Comparison of the therapeutic efficacy
After the treatment, there was a significant difference in the therapeutic efficacy between the two groups(P<0.01), suggesting that the observation group produced a more significant therapeutic efficacy than the acupuncture group (Table 3).
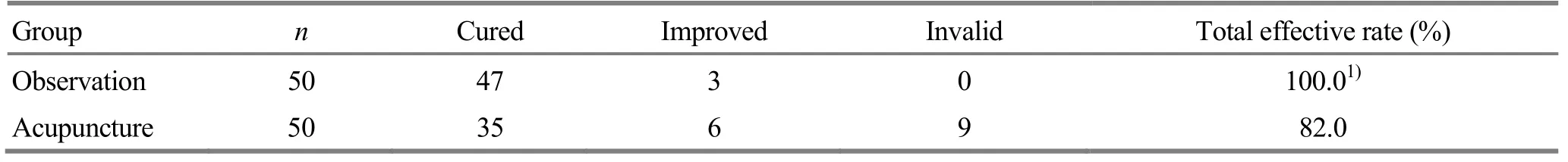
Table 3.Comparison of the clinical efficacy (case)
4 Discussion
CV belongs to the scope of vertigo or bone Bi-impediment syndrome in traditional Chinese medicine (TCM) and most commonly affects the elderly people[11].TCM holds that the head is the affected location while the liver, spleen and kidney are involved in this disease[12].
According to Western medicine, CV is caused by VBI and mainly manifests as dizziness, headache and blurred vision, or even cataplexy, vomiting, palpitations and chest tightness in some severe cases[13].Although there are several theories about the pathogenesis of CV,most of the domestic researchers agree that CV is a syndrome featured by dizziness and caused by vertebrobasilar artery blood flow dysfunction resulting from the influence on extracranial vertebral artery cervical diseases.It’s often triggered by the flexion,extension or turning of the neck and only lasts for a short time.The symptoms can be alleviated by the reposition of the neck[14].Modern clinical research has showed that cervical vertebral degeneration is the precondition of CV.Cervical vertebral degeneration further induces the degeneration of soft tissues and calcification of ligament, which will then compress or stimulate vertebral artery, leading to VBI and causing a series of symptoms including dizziness, headache,tinnitus and blurred vision[15-16].So far, acupuncture and tuina have been proved effective in treating cervical spondylosis.Acupoints in head and neck areas are often selected for acupuncture, since they can improve the blood supply to vertebral artery and then improve the related symptoms.TCD can sensitively reflect the cerebral blood flow velocity, pointing out abnormal blood flow, vasospasm and vascular sclerosis.It has been considered as an effective clinical measure in the evaluation of vertebral artery blood flow state.Of its parameters, since Vm is merely influenced by cardiovascular factors such as heart rate, cardiac contraction rate, peripheral resistance or aortic compliance, it’s become a significant indicator in clinical practice.Therefore, TCD was used as an objective therapeutic measure in this study[17].Acupuncture therapy can activate the flow of meridian qi and blood.Tuina can relax the spastic muscles, change the morphology and elasticity of topical vessels and muscular tension, speed up the local blood circulation,evoke the physiological regulation[18], improve the cervical microcirculation and the hypoxia-ischemic state,and rebuild the biomechanical balance of cervical vertebrae.The combination of the two methods can superimpose the therapeutic efficacy[19-21]via maximizing the vertebrobasilar artery blood flow velocity and attenuating the vertigo symptom.
 Journal of Acupuncture and Tuina Science2018年5期
Journal of Acupuncture and Tuina Science2018年5期
- Journal of Acupuncture and Tuina Science的其它文章
- Clinical observation of Zhen’ai needling method in Nei Jing (Classic of Internal Medicine) on improving quality of life in patients with allergic rhinitis
- Effect of acupoint massage plus acupoint sticking therapy for the stress reaction during postoperative anesthesia recovery period in patients undergoing nasal endoscopic surgery
- Effect of modified Qing Long Bai Wei needling on the levels of IL-1β, IL-6 and INF-α in synovial fluid of knee osteoarthritis patients
- Clinical observation of sinew-regulating and bone-setting manipulation combined with functional exercise to treat rotator cuff injury
- Clinical experience of Xiangxi Liu’s infantile tuina for exogenous fever in children
- Experimental study on the influence of pressing force and time on thermal effect of An-pressing manipulation
