The status quo and influence of self-management behaviors in convalescent stroke patients†
Original article
Feng-Guang Guana, Mei Wangb,*, Xiao-Qin Liana
aNursing Department, The Second Affiliated People’s Hospital, Fujian University of Traditional Chinese Medicine, Fuzhou, Fujian 350003, China
bSchool of Nursing, Fujian University of Traditional Chinese Medicine, Fuzhou, Fujian 350122, China
Abstract: Objective: The aims of this study were to investigate the status quo of self-management behaviors in stroke patients at the recovery stage and to explore its influencing factors.Methods: A total of 440 hospitalized convalescent stroke patients were recruited and investigated using the Basic Situation Questionnaire,Self-management Behavior Scale of Stroke, Stroke Prevention Knowledge Questionnaire and Social Support Rating Scale.Results: The mean self-management behavior score was (151.95±23.58), and dimensions in descending order were as follows:dietary management, drug safety management, social function and interpersonal relationships, life management, emotion management,rehabilitation exercise management and disease management. Five regional self-management behavior scores were statistically significant, and the scores from Minnan and Minzhong of the Fujian province, China, were higher than the others. Gender, age, family income and self-management behavior were significantly correlated (P<0.05); educational level, stroke knowledge level, social support level and self-management behavior were positively correlated, and the difference was statistically significant (P<0.01).Conclusions: The overall self-management level of convalescent stroke patients should be improved to strengthen health education;focus on the educational level, which is relatively low; strengthen the social support system of patients; stimulate the enthusiasm and initiative of self-management disease patients to promote disease rehabilitation and improve the quality of life.
Keywords: stroke • self-management • behavior • root cause analysis© Shanxi Medical Periodical Press.
1. Introduction
Stroke is the second leading cause of death in the world,according to the survey of the American Heart Association in 2015.1In the analysis of the Chinese stroke prevention and control report (2015), stroke is the leading cause of death in China, and its economic burden is as high as 40 billion yuan per year.2The high morbidity,high fatality rate, high disability rate, high recurrence rate, complications and long course of the disease seriously reduce the quality of life for stroke patients and put great pressure on the family and society.3The rehabilitation of stroke patients is multifaceted, among which rehabilitation management is an extremely important link.4Self-management is the monitoring and management of disease through proactive health behaviors,which reduce the effects of disease through treatment,disease maintenance and health promotion.5Studies6-8have shown that the self-management ability and quality of life of stroke patients are positively related and that good self-management behavior is essential for patients in stroke recovery to maximize the recovery of bodily functions, promote healthy behaviors, reduce recurrence and improve long-term survival. The purposesof this study were to investigate the self-management behaviors of stroke recovery patients through a questionnaire survey and to analyze their in fl uencing factors to provide references and ideas for building self-management skills in convalescent stroke patients.
2. Objects and methods
2.1. Study subjects
A total of 450 stroke recovery patients from nine hospitals of the Fujian province were selected. The inclusion criteria were cerebrovascular disease diagnosis of the fourth diagnostic criteria by brain computed tomography(CT) or magnetic resonance imaging (MRI) in stroke patients; the period of stable disease, with “restore”being the guiding principle of clinical research on new drugs of traditional Chinese medicine treatment for stroke in the recovery period, 15 days–6 months after the onset of stroke; clear consciousness; ability to use text or language communication; Barthel Index (BI)score >20; absence of swallowing dysfunction; and the ability to participate voluntarily. The exclusion criteria were the mental scale assessment for dementia or mental illness; association with other serious diseases, such as heart, kidney and liver insufficiency; and the complete loss of activity ability. The sample size of this study was eight times the number of items in the survey tool,“stroke self-management behavior scale”, considering a 10% falling rate, with the final sample of 450 cases.
2.2. Research tools
2.2.1. The basic situation questionnaire
According to our research purpose and the stroke characteristics of patients, a total of 14 items were included:gender, age, educational level, marital status, occupation, family income, medical payment, accompanying relatives and friends, visit type, frequency, treatment time, hospitalization time, complications, disease knowledge acquisition approaches and evaluation of the rehabilitative effect of others.
2.2.2. Self-management behavior scale of stroke patients
The self-management behavior scale of stroke patients,developed by Wang9in 2009, is used to re flect the change in self-management behaviors in stroke patients and consists of seven dimensions and 51 items, with good reliability and validity; Cronbach’s α coefficient was 0.835. This scale comprised specific content of disease management (11 items), drug safety management( five items), catering management (nine items), daily life management (eight items), emotion management ( five items), social function and interpersonal management(six items) and rehabilitation management (11 items).With the 5-point Likert scoring method, the total score was 50–250, and the higher the score, the better the self-management behavior of patients.
2.2.3. Stroke prevention knowledge questionnaire
The stroke prevention knowledge questionnaire was designed by Zhang10and covers daily life, exercise,diet, medication, blood pressure monitoring, risk factors,stroke symptoms and stroke treatment in eight dimensions, for a total of 36 items. In this scale, Cronbach’s α coefficient was 0.812 and there was good reliability and validity. Each entry option was “know” or “do not know”,with know=1 and do not know=0; the higher the score,the higher the level of stroke knowledge.
2.2.4. Social Support Rating Scale (SSRS)
The SSRS11consists of three dimensions composed of 10 items, including objective support (three items),subjective support (four items) and the degree of social support (three items). Four or more scores were used,and the sum of the 10 items was the total score of social support. In items 1–4 and 8–10, each patient made only one selection from A to D, scoring 1–4 points; for the fifth question, each patient selected from A to E, for a total score of 5 points. Each item was 1–4 points from “no” to “full support”; for the sixth and seventh questions, if the answer was “no source”, then the score was 0 point, and then, the following source was answered by selecting the source number. The higher the score, the higher the level of social support received by participants.
2.3. Survey methodology
A questionnaire was distributed after a unifi ed training study to meet the inclusion criteria for stroke recovery inpatients and to obtain informed consent. The patient was told how to fill out the survey, and if in doubt, a unified survey language was used to explain it. The patient himself or herself filled out the questionnaire on the spot,and if the patient could not fill it out alone, the researcher assisted the patient and avoided introducing words during this period. After being completed, the questionnaire was recovered on the spot to ensure the integrity of the data. A total of 450 questionnaires were issued and recovered, among which 440 were valid; thus, the effective participation rate was 97.78%.
2.4. Statistical methods
Data collection was conducted with an Excel database,using IBM SPSS Statistics 20.0 statistical software for the descriptive statistics of general demographic data; data were counted as percentage (%), data were measured as mean and standard deviation (descriptive) and comparison between groups were carried out using at-test and single factor analysis of variance (P<0.05). The knowledge score for stroke prevention and treatment was graded according to score: >80% as good, 60%–80% as medium and <60% as not good. Pearson correlation analysis and multiple linear regression analysis were used to evaluate self-management in stroke patients and recovery factors;P<0.01 was considered as statistically significant.
3. Results
3.1. Self-management level of patients with stroke convalescence
The self-management behavior score in the stroke recovery stage ranged from 75 to 211, with a mean of 151.95±23.58. The seven latitudes were sorted according to the scoring index from high to low: dietary management, safe medication management, social functioning and interpersonal relationships, daily life management, emotion management, rehabilitation exercise management and disease management.For the Fujian province, the five regions of the selfmanagement of patients with the stroke recovery score were statistically significant (P=0.000,P<0.05); there were significant differences in the four latitudes: disease management, medication management, food safety management and rehabilitation management.See Tables 1 and 2 for details.
3.2. Single-factor analysis of selfmanagement and demographic data with stroke convalescence
There was a significant effect (P<0.05) found for stroke recovery score of self-management behavior differences in the single-factor analysis of self-management level by age, gender, educational level and family income per month; no statistically significant differences were foundfor the scores of other projects (P>0.05). The scores are presented in Table 3.
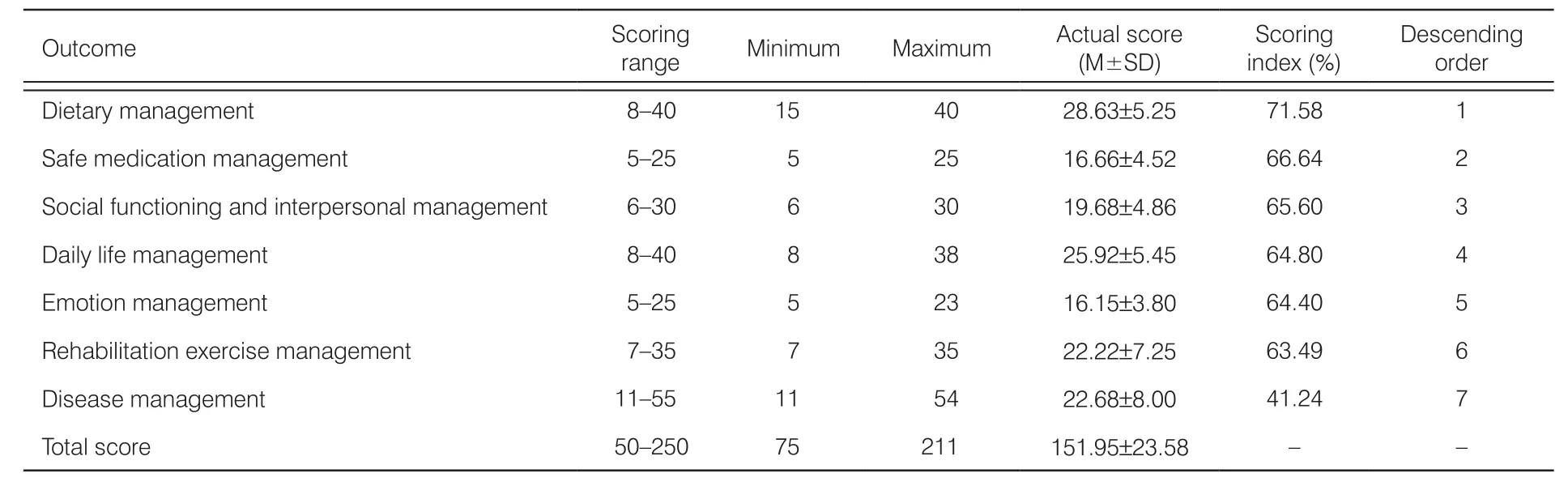
Table 1. Scores of self-management dimensions in the stroke recovery stage (n=440).
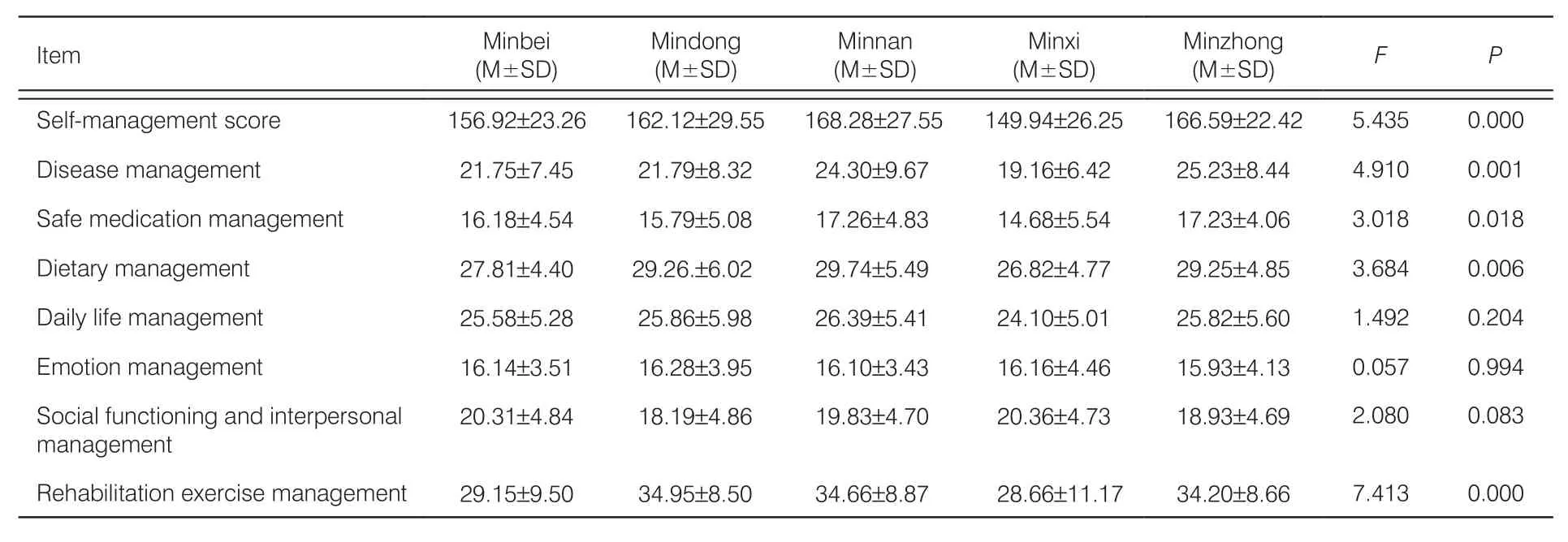
Table 2. Self-management behavior scores of Mindong, Minxi, Minnan, Minbei, and Minzhong, Fujian province (n=440).
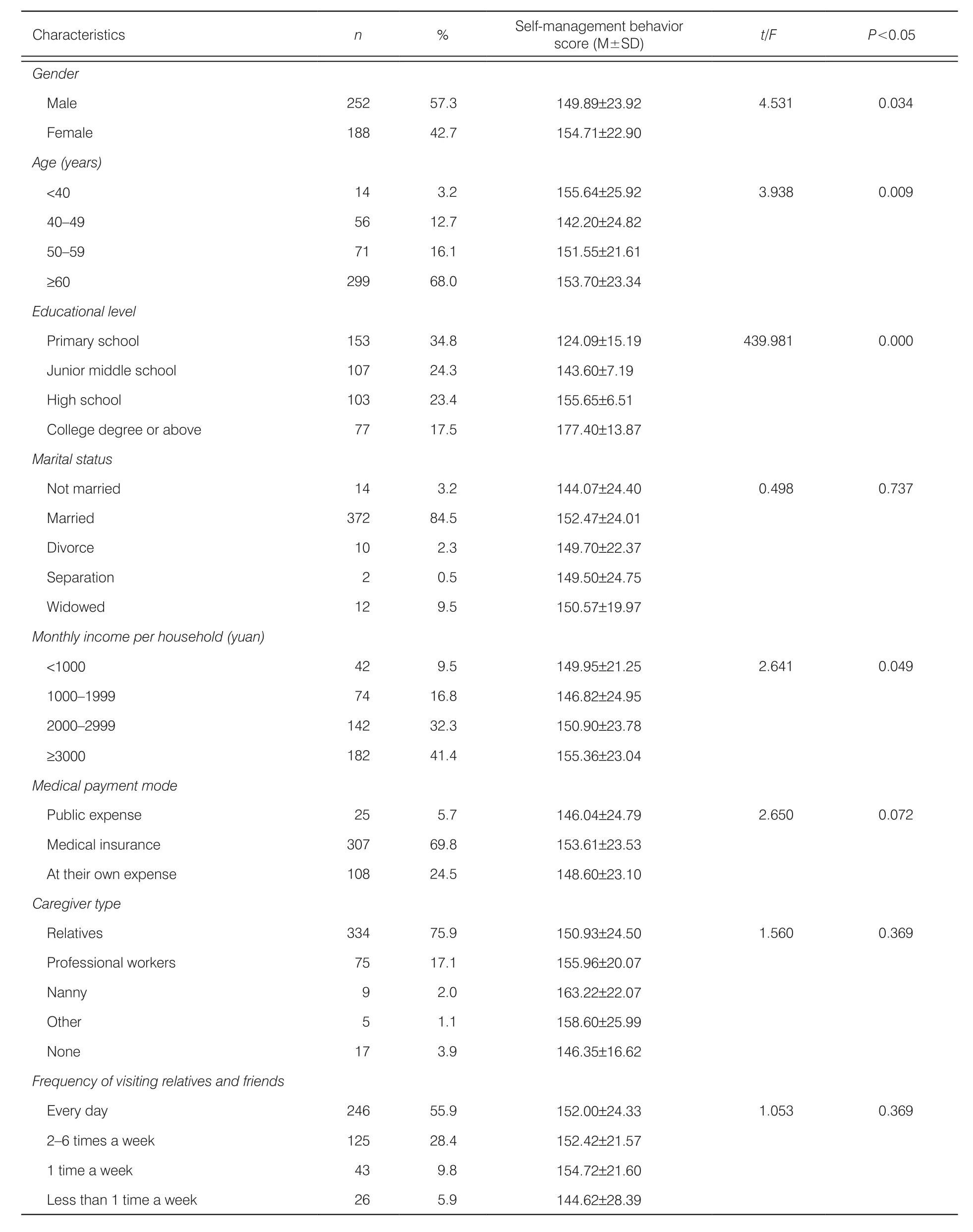
Table 3. Single-factor analysis of demographic data of patients in the stroke recovery stage (n=440).
3.3. Stroke knowledge level
The score for prevention and control knowledge of stroke recovery patients was (26.80±7.78), and the overall score of patients was medium, among which stroke treatment and risk factors were the lowest. The scores from diet, daily life, exercise, blood pressure monitoring, stroke symptoms, medication, risk factors,and stroke treatment followed from high to low. See Table 4 for details.
3.4. Correlation analysis of self-management behaviors and stroke knowledge level,social support level and education level
Because the variables were continuous and continued to have a normal distribution, Pearson’s correlation analysis was performed The results showed that the level of stroke knowledge, social support and educational level were positively related to self-managementbehaviors, and the correlation coefficients werer=0.252,r=0.193 andr=0.863, respectively. The difference was statistically significant,P<0.01.
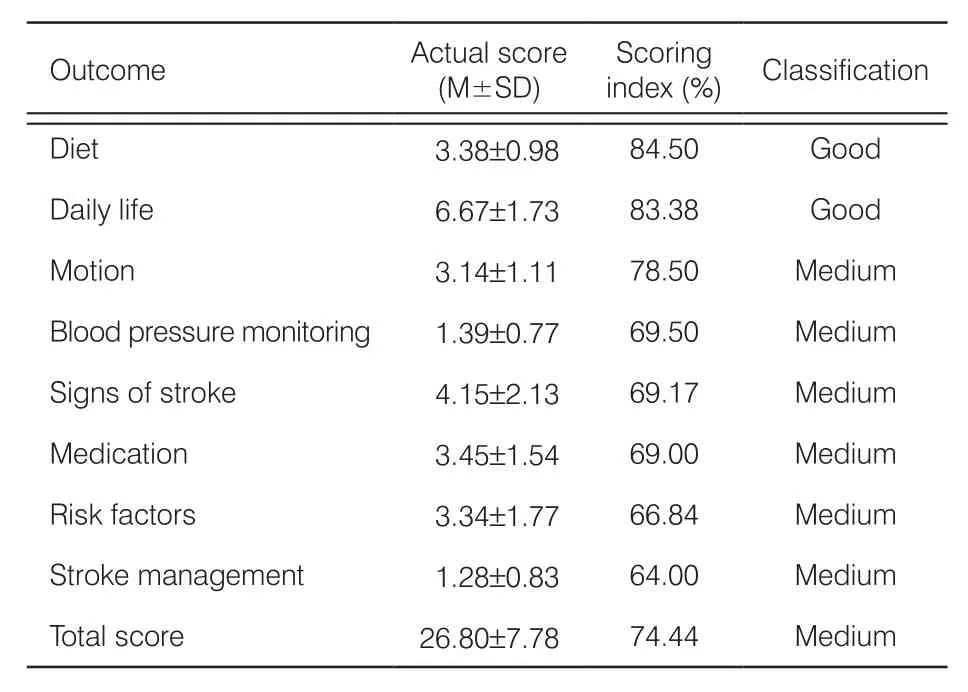
Table 4. Stroke prevention and treatment knowledge score in the stroke recovery stage (n=440).
3.5. Multiple regression analysis on influencing factors of self-management behaviors in the stroke recovery stage
According to the results of the single-factor analysis, we selected educational level, stroke knowledge level, and social support level as independent variables and selfmanagement score as the dependent variable for use in the multiple linear stepwise regression analysis. The collinearity diagnostic tolerance of the regression equation was 0.953–0.976 (>0.1), and the variance inflation factor (VIF) was 1.024–1.049 (<10). It can be considered that there was no multicollinearity between the three independent variables, which accords with basic multiple linear regression assumptions. The results show that the education level, stroke knowledge level,and social support level are the factors that influence the self-management behaviors of stroke patients in recovery. Three of the total load contributions of size are as follows: educational level, social support level,stroke knowledge level, and a common interpretation of self-management behavior level. The variance is 75.8%(Table 5).
4. Discussion
4.1. Status quo of self-management behavior in the stroke recovery stage
In this group of patients in stroke recovery, the total mean score of patient self-management was 151.95±23.58, higher than that of Mu et al.,12and this group is included in the study on the recovery of stroke patients, self-cognition and behavior for knowledge management attention; this score is higher than in the group of first-stroke patients. Self-management hasseven dimensions according to the score, from high to low: dietary management, drug safety management,social functioning and interpersonal relationships, life management, emotion management, and rehabilitation of disease management. The highest scores for patients were for dietary management and drug safety management, because the subjects of this study was in the period of hospitalization, health care provider continue to provide health education to patients with disease, and are in compliance during hospitalization regarding good medication and diet, which influence, to a certain extent,the two latitude scores. Patients with poor performance in rehabilitation exercise management and disease management behavior had the worst disease management behavior, which is consistent with the studies of Wang et al.13and Liu et al.14who analyzed a number of factors that may be related to disease rehabilitation in the long term: lack of perseverance, imperfect rehabilitation equipment, lack of knowledge and skills for rehabilitation, medical expenses, etc.; the authors suggest strengthening the rehabilitation training of patients with guidance and helping patients build self-confidence with disease monitoring.
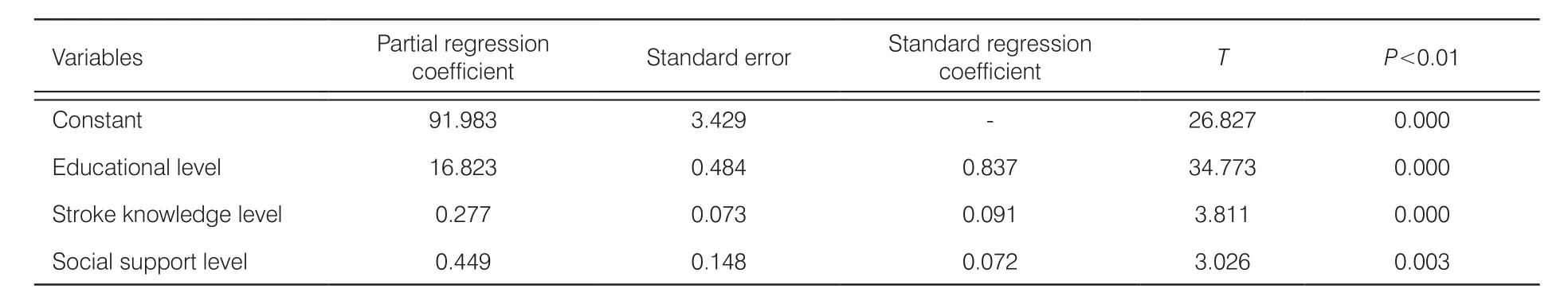
Table 5. In fluencing factors of self-management in the stroke recovery stage (n=440).
The self-management behavior scores for the five regions of the Fujian province were statistically signi ficant, and there were significant differences in disease management, safe medication management, dietary management and rehabilitation exercise management.The two regional scores for Minnan and Minzhong were higher than the others, and the analysts believed that this outcome was related to economic integration, as these areas represent the political, economic, cultural and scientific research centers of the Fujian province.
4.2. Analysis of the influencing factors of self-management behaviors in the stroke recovery stage
4.2.1. Educational level
Educational level is an important predictor of self-management behaviors of patients, since the higher the level of education, the higher the level of health selfmanagement, and these results were similar to those of Mu et al.12and Li et al.15Patients with a high educational level learn, understand and absorb knowledge and information more comprehensively and deeply and can obtain self-health care knowledge in more ways; they have better communication with medical staff; are more willing to adopt self-beneficial treatment, a rehabilitation plan and care and engage in more conscious and active learning and the implementation of effective disease self-management behaviors. Therefore, for patients, the medical staff should follow the principles of the person and take a path of culturally relevant health education.For patients with a low degree of culture, the medical staff should use understandable words and talk about,explain, and repeat the key disease self-management points many times. For highly educated patients, it is necessary to meet self-actualization (Tables 2 and 4).
4.2.2. Social support level
Social support can effectively help patients mobilize psychological resources to cope with negative emotions and meet their needs through the process of hardship and suffering together by providing material support and psychological support and by helping patients adapt to success. The findings of this study confirm that social support levels can influence self-management behaviors, which is consistent with the findings of previous studies.16,17Good social support can effectively promote physical and mental development in patients and improve self-management behavior. In clinical nursing,we should fully mobilize the social resources of patients,especially focusing on the good role of family function,and ensure the quality of social support.
4.2.3. Stroke knowledge level
This study shows that stroke knowledge level is an important factor in self-management behavior and that the cognitive level of stroke management and risk factors is low. Most patients do not know the prime window of opportunity for stroke treatment, often missing the best time to treat. Therefore, for these patients in stroke recovery, knowledge about the disease should be emphasized during self-management health education,especially the treatment and risk factors of stroke.
5. Conclusions
The overall level of the self-management of stroke patients needs to be improved and should be strengthened through health education by paying attention to lower cultural degree, by helping to mobilize patient social support systems and overall, by stimulating the enthusiasm and initiative of self-management disease patients to promote disease recovery and improve quality of life.
Conflicts of interest
All contributing authors declare no conflicts of interest.
- Frontiers of Nursing的其它文章
- Preoperative nutrition and postoperative liver function: a correlation study of pediatric living donor liver transplantation†
- Characteristics of and management strategies for 54 suicidal inpatients in a general hospital†
- Visualization analysis of the study of fund-sponsored clinical nursing papers†
- A systematic review of the effectiveness of clinical nurse specialist interventions in patients with chronic obstructive pulmonary disease (COPD)
- Prevalence of osteoarthritis and association between smoking patterns and osteoarthritis in China: a cross-sectional study†
- Development and application of a closed-loop medication administration system in University of Hongkong-Shenzhen Hospital†