Effects of balance training prior total knee replacement surgery: study protocol for a randomized controlled trial
José-María Blasco , Fernando Dominguez-Navarro Celedonia Igual-Camacho , Antonio Silvestre-Muñoz, ,Sergio Roig-Casasús
1 Department of Physiotherapy, University of Valencia, Valencia, Spain
2 Group of Physiotherapy in the Ageing Process, University of Valencia, Valencia, Spain
3 IRIMED Joint Research Unit La Fe Hospital - Universty of Valencia, Valencia, Spain
4 Hospital Clínico y Universitario de Valencia, Valencia, Spain
5 Department of Trauma and Orthopaedic Surgery, University of Valencia, Valencia, Spain
6 Hospital Universitario y Politécnico de La Fe, Valencia, Spain
INTRODUCTION
Many of the limitations found after an intervention of total knee arthroplasty are related to balance disorders, for instance difficulties in walking or altered moving patterns.1,2Therefore,the inclusion of specific balance and proprioception protocol in conventional physiotherapy care could have a potential clinical impact on both balance and functional capacities.
The effectiveness of sensorimotor trainings in subjects with knee osteoarthritis has been studied by several authors.3,4A recent review suggested the viability of the proposal for the rehabilitation of knee arthroplasty.5But also showed that literature is still scarce, especially in preoperative terms,highlighting the need for new research in order to clarify the effects and dose of exercise.6-10
This research aims to determine the early-postoperative effects of a preoperative muscle enhancement program that includes a specifically oriented protocol of balance and proprioception training in the methods. It is hypothesized that balance skills will be enhanced, which in turn will positively influence the patient functionality. This research will also appraise the cost-effectiveness of the proposal, based on data extracted from long-term evaluations.
METHODS/DESIGN
Design, setting and participants
This is a prospective three-arm, randomized controlled trial.The participants will be recruited from the Hospital Clínico y Universitario de Valencia, Spain and randomized to three groups: a control group, which performs conventional physiotherapy after surgery of total knee arthroplasty, an active comparator group, which additionally performs a muscle enhancement program preparatory for surgery, and an experimental group that performs the same intervention as the active comparator, but also includes a specifically oriented program to enhance balance and proprioception. Theflow chart of the study is shown in Figure 1.
Patients meeting the following criteria will be selected as study volunteers: (1) men and women aged between 60–80 years, (2) patients with severe knee osteoarthritis, (3) patients who will undergo theirfirst surgery for total arthroplasty, and(4) patients who present a low risk of falling with a score of over 40 on the Berg Balance Scale11and a moderate cognitive condition to adequately follow the interventions, with more than 20 points in the Spanish version of Lobo of the Mini-Mental State Examination.12Participants meeting one of the following criteria will be excluded: (1) central or vestibular affections that directly affect their balance or (2) postoperative complications as possible infections.
In thefirst instance, the surgeons choose the potential participants by means of examination and medical chart.The physical and cognitive evaluation in terms of the Berg Balance Scale and Lobo Cognitive Scale is performed by physiotherapists in the rehabilitation service. If the criteria are met, the potential participant is informed about the study and is invited to participate. If the potential participants agree to participate, has to sign an informed consent, and becomes part of the randomization process.
Randomization and blinding
The randomization is sequential. Once the surgery date is known, thefirst evaluation is carried out as well as the group allocation, depending on the output of a program that generates random numbers (Matlab®). An external advisor, who is blinded to intervention groups, informs rehabilitator responsible of the participant allocation by means of a numerical code. The patient is informed of physiotherapy sessions by phone. Four physiotherapists in the rehabilitation service with more than 15 years of experience are responsible for physiotherapeutic interventions. The physiotherapists are not blinded to the interventions, because they know the programs and have actively participated in its implementation. The blinding of participants is not ensured, as they are informed about the project due to strict regulation. An independent evaluator,blinded to the interventions, is responsible for the assessment of the participants. The external advisor will be responsible for the statistical processing of data.
Sample size
Sample size and power calculation were based on the primary outcome the Berg Balance scale at 6 weeks. Based on the results of a previous work that evaluated the effectiveness of a postoperative balance training for total knee replacement,13and in which the difference between groups was above the minimum detectable change of 5 points in the primary outcomefor α=0.05 and β=0.02, an estimate was made with the tool G*Power3.1.14We considered that the experimental group will be above the control group in such scale by 5 points. Therefore, it is estimated that a sample size of 21 participants per group will be required to provide a power over 80%. Considering a 20 %dropout rate during the study, a minimum of 78 total participants is needed to reach the target 26 participants per group.
Interventions
The supervised preoperative muscle strengthening intervention(MSI) has been designed as an active comparator. A traditional training program for conditioning and muscular enhancementis based on progressive resistive loads according to the technique of DeLorme and Watkins.15This lasts for 4 weeks or 12 sessions of approximately 45 minutes, on alternate days. In the warm-up phase, the muscles of the lower limbs are prepared.The exercises are performed in 3 sets of 10 repetitions with loads of half of the 10 repetition maximum (RM).15In the work phase, aimed at the enhancement of the quadriceps, hamstrings,abductors and adductors, the loads become 10 RM. The loads are adapted to the possibilities of the participants looking for a maximum performance, but also try to avoid fatigue. In the cooling phase static cycling, stretching and cryotherapy are performed.
Strengths and limitations
The supervised preoperative experimental hospital balance and proprioceptive intervention (BPI) consists of different exercises developed over the course of the 12 sessions on alternate days, divided in 4 weeks of training. Each session includes a total of 4 to 5 exercises performed over a period of 20 minutes. The training has been based on the Fitzgerald principles to train proprioception in total knee replacement,but also on previous of our works and on the team clinical experience.13,16Thefirst two weeks are oriented to enhance balance and proprioception with the side, treadmill, cross, and tandem walk exercises. These exercises are excluded in weeks 2 and 3, and multiple changes of direction, foam activities and balance work with the Bohler plate are performed instead. Also 5 minutes training of weight bearing and testing the limits of stability are performed during the last 4 sessions, due to the good results achieved in the previous works.13Progression in the exercises is implemented as tolerated, always trying to avoid fatigue.
The procedures were standardized and pilot tested to ensure participant recruitment, outcome evaluation, data handling and management, and safety. A verification of the procedures is planned for periods of 6 months, through observation and meetings to ensure the reproducibility of the protocols and their consistency.
Outcomes
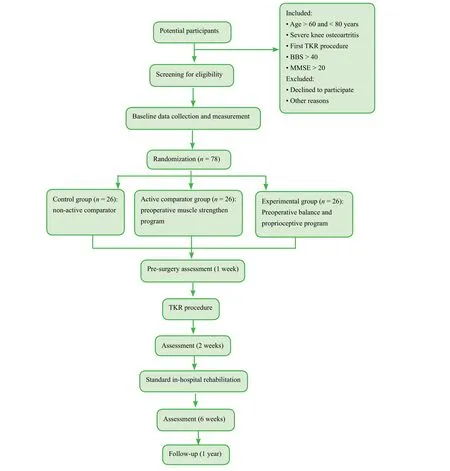
Figure 1: Flow diagram of this study.
First sample descriptors, possible predictors such as preoperative pain, anxiety, function or body mass,17and the baseline characterization in terms of the demographic and biomedical characteristics are extracted. Baseline data collection will be performed between 10 and 4 weeks before surgery. Outcomes will be measured at 1 week before surgery. After the total knee replacement procedure, outcomes will be assessed at 2 weeks and 6 weeks. Follow-up will be assessed at 1 year after surgery.Detailed information is shown in Figure 1.
Primary outcomes
Two outcomes have been prioritized. The overall state of balance as measured with the Berg Balance Scale,11and the self-reported functionality in terms of the joint and diseasespecific Knee Injury Osteoarthritis Outcome Function Score(KOOS) questionnaire,18as measured with the subscale function in daily living. The primary outcomes will be assessed at 6 weeks after surgery.
Secondary outcomes
Complementary balance evaluations will be performed in order to determine balance abilities in dynamic terms, as measured with the Timed Up & Go Test,19as well as static terms, as measured with the Single Leg Standing Balance Test, andfinally in terms of stability, as measured with the Functional Reach Test.20
The knee function will be assessed with traditional objective clinician-reported outcomes in total knee replacement,including the range of movement and the isometric muscular strength, using a dynamometer Manual Muscle Tester 01165 Lafayette Instrument®and a goniometer.
KOOS is a self-reported questionnaire developed as an instrument to assess the patient’s opinion about their knee and associated problems. Only the function in daily living subscale will be used as primary outcome. Even though the pain, other symptoms, function in daily living, and knee-related quality of life will be included in the assessments. Function in sport and recreation will not be evaluated.
Quality of life will be assessed the Euro Quality of Life Five Dimensions health-related questionnaire.21This will be used to undertake the cost-effectiveness analysis.
Assessment of outcomes
Outcomes will be assessed by a blinded physiotherapist according to the schedule shown in Table 1.
Data analysis
The baseline characteristics of the sample and the implementation of protocols will be presented with descriptive statistics. A comparison of the baseline condition with the t tests that will be parametric or not depending on the results of the tests of Wilcoxon and Shapiro-Wilk. The main hypothesis is that participants in the experimental group and active comparator will demonstrate better balance abilities and physical function than participants in the control group,but also that the experimental group may demonstrate even higher performances than the active comparator. Analysis will be performed for primary and secondary outcomes based on linear mixed models and controlling for baseline scores, looking for time, group, and time per group interactions. Special attention will be given to early postoperative outcomes (6 weeks) and long-term follow-up (1 year). Intention to treat principle will be applied. Post-hoc analyses will be performed accordingly. Confidence intervals will be set at 95%.
A qualitative analysis will be carried out in which it will be estimated if the obtained progressions measured as the mean values of the difference between the basal andfinal values for each variable at each time point reach the minimum established according to the psychometric properties referring to the minimum clinical importance difference or minimum detectable change with a confidence interval of 95%, based on the suggested minimum value when reported more than once.
Inclusion criteria are broad. It is likely that biomedical and psychosocial baseline characteristics influences treatment results. Depending on whether a participant achieves a progression superior to the minimum detectable change in one of the primary outcomes, participants will be binary classified. Logistic regression model will be conducted in order to extract predictors.
A post-hoc power analysis and an estimate of the effect size will be implemented with the tool G*Power,14based on Cohen’s d and considering a low, medium or high effect as a function of the result.
Dropouts and missing data
Descriptive statistics will summarize the compliance with protocols and dropout rates. The incidence of adverse effects at 6 weeks and 1 year will be evaluated, and classified and related, likely related or none related to the interventions.Every effort will be made to reduce sample loss, particu-larly with regard to long-term monitoring. In the event that a participant cannot or decides not to attend the follow-up evaluation, it is proposed to resolve the self-reported surveys at home and forward them via email, or the possibility of the evaluator's displacement is also granted. To deal with missing data, we will extract the reasons in order to choose adequate data analysis, to apply the intention to treat principle, and estimate the possible impact on the results.22
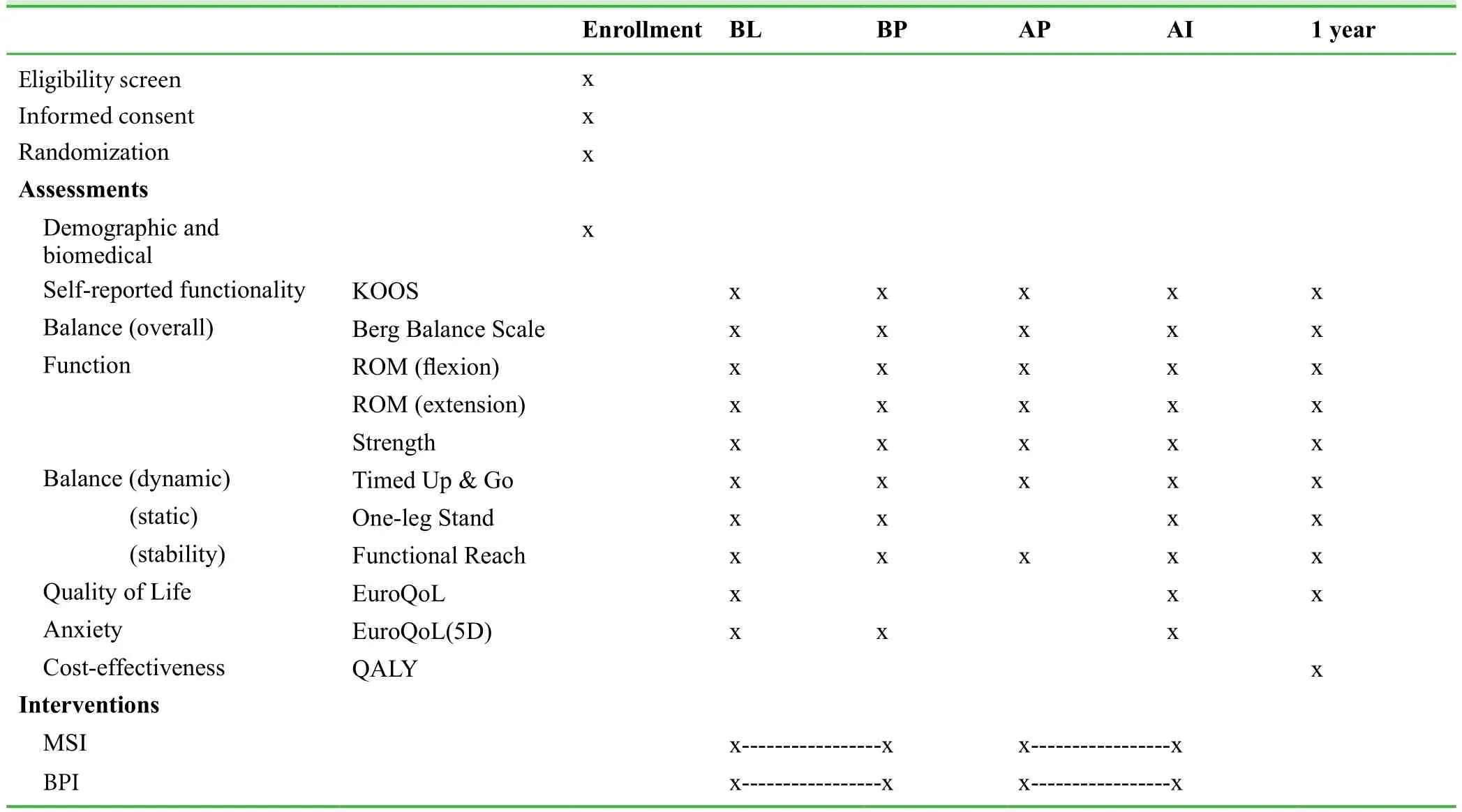
Table 1: Detail of variables and times for evaluation of outcomes
Cost-effectiveness analysis
Incremental costs will be compared with incremental quality adjusted life years gained (QALY) at 12 month postoperative.The measure of effectiveness will be based on the results of the EuroQoL-5D. QALY will be estimated with the Spanish intervention rate using unit cost estimates from national tariffs, and associated with the time trade-off method. Costs and QALY will be adjusted for stratification variables and baseline utility by means of regression methods. Groups will be compared in order to determine the more effective and less costly arm. The arm with these characteristics will be considered the most cost-effective. We will plot effects in cost-effectiveness planes and acceptability curves to consider uncertainty around the adoption decision. Finally a sensitivity analysis will allow knowing the robustness.
Ethics and dissemination
The study protocol follows the Standard Protocol Items: Recommendations for InterventionalTrials (SPIRIT) guidance for protocol reporting (Additionalfile 1). The procedures have been approved by the Ethics Committee and by the Scientific Committee of the Clinical and University Hospital of Valencia (approval No. 26052016) and conform to the Declarationof Helsinki. It was registered prospectively in January 2017 (ClinicalTrials.gov identifier NCT02995668).All patients will sign the written informedconsent prior to enrolment. The authors of the current protocol article will also be co-authors on publications derived from this study relative to their specific contributions. We will publish thefindings in national and international peer-reviewed journals,and present these at national and international conferences.
DISCUSSION
Osteoarthritis is the most frequent cause of pain in the knee in adults older than 50 years.23Due to the population ageing and high prevalence, this condition may be considered as a real public health problem.24Thefigures are above 30% in adults older than 65 years, afigure that increases linearly with age.25In the advanced stages, the solution involves the replacement of the joint by a prosthesis, a process known as total knee arthroplasty.
As has been argued, in functional terms the main limitations presented by subjects are usually related to balance skills.However, this aspect is not usually approached in a specific way, but rather some oriented elements are usually introduced in the programs. Taking into account the importance of the recovery of the balance, and taking into account its correlation with functionality, the research on the intervention proposal is interesting and justified.
The optimization of early post-surgical results is achieved with an adequate physiotherapeutic treatment. After surgery,rehabilitation is usually conducted in hospitals, being the length of stay variable. The programs are adjusted to achieve greater autonomy and dependence, in the shortest possible time, and at the lowest cost. In addition, a muscle conditioning program is always recommended before surgery.26Despite this, the evidence remains inconclusive, especially in terms of those trainings specifically oriented to the enhancement of balance and proprioception. Previously, a training based on balance and proprioception exercises was evaluated, and the study suggested that the approach could potentially prevent future modified patterns in walking.7However, some of the appraised aspects were not fully clarified. Other authors evaluated a similar preoperative proposal, based on a neuromuscular training program. Hubber et al.8dis not achieved conclusive results, while Villadsen et al.9suggested earlier onset of postoperative recovery, based on the short-term benefits achieved in terms of performance of the activities of daily living and pain reduction. All of them concluded that further research was necessary in order to give consistency to thefindings.
Focusing of the design of the trial and with respect to the inclusion criteria, these are broad, and do not exclude a large number of subjects with depressive symptoms, with poor motivation, or with a broad spectrum of comorbidities that are common in the targeted population. Nor considered other risk factors which are typical of the condition, such as body mass or advanced age. Therefore, the criteria have not been designed to achieve good scientific results, but to critically appraise the outcomes by considering a sample whose characteristics are representative and as close as possible to the clinic reality.
The interventions are pragmatic and realistic. The clinical experience of professionals with long experience in knee replacement rehabilitation was essential to complete the design, along with the results of previous research and updated literature. Protocols have not been designed to be complex and barely applicable. Neither to be long, since more than 4 weeks prior surgery is hardly assumed in hospital setting, and imply many resources as well as little practical applicability.With respect to the design of the interventions, the control group does not perform preoperative training. The active comparator performs a basic work of muscle enhancement.Additionally, the experimental group includes specific training of balance and proprioception. The design with three groups certainly makes the work more tedious. But it is also true that previous similar studies lack a third interventional group, suggesting this fact as a limitation, or proposing its inclusion in future research. In this way, the inclusion of active comparator and non-active control group will make possible to demonstrate the real effects of the experimental proposal.We cannot forget that the costs associated with an additional preoperative program are high, especially if they are carried out in hospital setting. The benefits have to be justified in economic terms. For this reason, not only the early postoperative effects will be evaluated, but also the long-term effects. Considering costs and the actual limitation of resources, the search for both effective and efficient strategies in order to optimize surgical results is essential. It is expected that the results will conclude the cost-effectiveness of the proposal, determining the prag-matism and applicability in clinical practice.
It is necessary to recognize limitations such as the fact that the follow-up is prolonged beyond usual in clinical practice, and that some of the measures are not always used by clinicians, although they are indeed used in research. This manuscript serves as a basis for reducing implementation bias. In case of substantial changes in the protocol, they will be duly reported with the reasons.
TRIAL STATUS
The trial started recruiting participants in January 2017. Recruitment status in October 2017 is below 50%. We expect tofinalize the enrolment by June 2018. Early postoperative outcomes will be available by November 2018. Follow-up will be likely completed one year later, by the end of 2019.
Additional file
Additionalfile 1: SPIRIT Checklist.
Author contributions
Conception: JMB, SRC, CIC. Design of the interventions: JMB, SRC,CIC, ASM, FDN. Literature search: JMB, FDN, ASM. Method, statistical and economic analysis advice: JMB. Drafting the article: JMB,FDN. Manuscript editing: FDN. Revising it critically for important intellectual content: CIC, SRC, ASM. All authors gavefinal approval of the version to be published.
Conflicts of interest
There are no competing interests or funding to declare.
Financial support
None.
Research ethics
The procedures have been approved by The trial was approved by the Ethics Committee and by the Scientific Committee of the Clinical and University Hospital of Valencia (approval No. 26052016) and conform to the principles of the Declaration of Helsinki.
Declaration of patient consent
The authors certify that they will obtain all appropriate patient consent forms. In the form the patients will give their consent for clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity.
Data sharing statement
Individual participant data that underlie the results reported in this article, after deidentification (text, tables,figures, and appendices)can be requested and shared on reasonable request, including documents, such as the informed consent form and the board approval. The data will be available immediately following publication and ending 36 months following article publication for those researchers who provide a methodologically sound proposal to achieve aims in such proposal. Proposals should be directed to jose.maria.basco@uv.es. To gain access, data requestors will need to sign a data access agreement.
Plagiarism check
Checked twice by iThenticate.
Peer review
Externally peer reviewed.
Open access statement
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-Shar eAlike 3.0 License,which allows others to remix, tweak, and build upon the work noncommercially, as long as the author is credited and the new creations are licensed under identical terms.
REFERENCES
1. Wada M, Kawahara H, Shimada S, Miyazaki T, Baba H. Joint pro prioception before and after total knee arthroplasty. Clin Orthop Relat Res. 2002;403:161-167.
2. Barrett DS, Cobb AG, Bentley G. Joint proprioception in normal,osteoarthritic and replaced knees. J Bone Joint Surg Br. 1991;73:53-56.
3. Ahmed AF. Effect of sensorimotor training on balance in elderly patients with knee osteoarthritis. J Adv Res. 2011;2:305-311.
4. Tsauo J, Cheng P, Yang R. The effects of sensorimotor training on knee proprioception and function for patients with knee osteoarthritis: A preliminary report. Clin Rehabil. 2008;22:448-457.
5. Moutzouri M, Gleeson N, Billis E, Panoutsopoulou I, Gliatis J. What is the effect of sensori-motor training on functional outcome and balance performance of patients’ undergoing TKR? A systematic review.Physiotherapy. 2016;102:136-144.
6. Pohl T, Brauner T, Wearing S, Stamer K, Horstmann T. Effects of sensorimotor training volume on recovery of sensorimotor function in patients following lower limb arthroplasty. BMC Musculoskelet Disord. 2015;16:195.
7. Gstoettner M, Raschner C, Dirnberger E, Leimser H, Krismer M.Preoperative proprioceptive training in patients with total knee arthroplasty. Knee. 2011;18:265-270.
8. Huber EO, Roos EM, Meichtry A, de Bie RA, Bischoff-Ferrari HA.Effect of preoperative neuromuscular training (NEMEX-TJR) on functional outcome after total knee replacement: An assessor-blinded randomized controlled trial. BMC Musculoskelet Disord. 2015;16:101.
9. Villadsen A, Overgaard S, Holsgaard-Larsen A, Christensen R,Roos EM. Postoperative effects of neuromuscular exercise prior to hip or knee arthroplasty: A randomised controlled trial. Ann Rheum Dis.2014;73:1130-1137.
10. Ibrahim MS, Alazzawi S, Nizam I, Haddad FS. An evidence-based review of enhanced recovery interventions in knee replacement surgery. Ann R Coll Surg Engl.2013;95:386-389.
11. Berg KO, Wood-Dauphinee SL, Williams JI, Maki B. Measuring balance in the elderly: Validation of an instrument. Can J Public Health.1992;83 Suppl 2:S7-11.
12. Lobo A, Saz P, Marcos G, et al. Revalidación y normalización del mini-examen cognoscitivo (primera versión en castellano del minimental status examination) en la población general geriátrica. Med Clín. 1999;112:767-774.
13. Roig-Casasús S, Blasco JM, López-Bueno L, Blasco-Igual MC.Balance training with a dynamometric platform following total knee replacement: A randomized controlled trial. J Geriatr Phys Ther. 2017.doi: 10.1519/JPT.0000000000000121.
14. Faul F, Erdfelder E, Lang A, Buchner A. G* power 3: Aflexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175-191.
15. Todd JS, Shurley JP, Todd TC. Thomas L. DeLorme and the science of progressive resistance exercise. J Strength Cond Res. 2012;26:2913-2923.
16. Fitzgerald GK, Childs JD, Ridge TM, Irrgang JJ. Agility and perturbation training for a physically active individual with knee osteoarthritis.Phys Ther. 2002;82:372-382.
17. Judge A, Arden NK, Cooper C, et al. Predictors of outcomes of total knee replacement surgery. Rheumatology (Oxford). 2012;51(10):1804-1813.
18. Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee injury and osteoarthritis outcome score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther.1998;28:88-96.
19. Podsiadlo D, Richardson S. The timed “Up & go”: A test of basic functional mobility for frail elderly persons. J Am Geriatr Soc.1991;39:142-148.
20. Duncan PW, Weiner DK, Chandler J, Studenski S. Functional reach: A new clinical measure of balance. J Gerontol. 1990;45:M197.
21. Rabin R, de Charro F. EQ-5D: A measure of health status from the EuroQol group. Ann Med. 2001;33:337-343.
22. Friedman LM, Furberg C, DeMets DL, Reboussin DM, Granger CB.Fundamentals of Clinical Trials. Vol 3. Springer; 1998.
23. Heidari B. Knee osteoarthritis prevalence, risk factors, pathogenesis and features: Part I. Caspian J Intern Med. 2011;2:205-212.
24. Cross M, Smith E, Hoy D, et al. The global burden of hip and knee osteoarthritis: Estimates from the global burden of disease 2010 study.Ann Rheum Dis. 2014;73:1323-1330.
25. Seoane-Mato D, Sánchez-Piedra C, Silva-Fernández L, et al. Prevalence of rheumatic diseases in adult population in Spain (EPISER 2016 study): Aims and methodology. Reumatol Clin. 2017. pii: S1699-258X(17)30168-7.
26. Lowe CJM, Barker KL, Dewey M, Sackley CM. Effectiveness of physiotherapy exercise after knee arthroplasty for osteoarthritis: Systematic review and meta-analysis of randomised controlled trials. BMJ.2007;335:812.
 Clinical Trials in Orthopedic Disorder2018年1期
Clinical Trials in Orthopedic Disorder2018年1期
- Clinical Trials in Orthopedic Disorder的其它文章
- Information for Authors - Clinical Trials in Orthopedic Disorders (CTOD)
- A newfixation and reconstruction method versus arthroscopic reconstruction for treating avulsion fracture at the tibial insertion of the knee posterior cruciate ligament: study protocol for a nonrandomized controlled trial and preliminary results
- Total hip arthroplasty via the direct anterior approach versus lateral approach: study protocol for a randomized controlled trial
- Evaluation of a computer-assisted orthopedic training system for learning knee replacement surgery:a prospective randomized trial
- Functional outcomes and health-related quality of life after open repair of rotator cuff tears: a prospective cohort study
