Observation on clinical effect of tuina plus Western medication for functional dyspepsia due to liver qi stagnation and spleen deficiency
Ning Jiong-jie (宁炯杰), Yu Jun (于隽), Li Wu (李武), Li Jiang-shan (李江山)
Hunan University of Chinese Medicine, Changsha 410007, China
Functional dyspepsia (FD) is a common pattern in dyspepsia, accounting for over 70% of the patients with dyspepsia by endoscopic examination[1]. The incidence rate of FD is quite high, accounting for 20%-40% of the diseases in the gastroenterological outpatients[2]. FD has a high relapse rate and can greatly affect the patient’s life. Currently, FD is mainly treated by promoting the gastrointestinal dynamics. But, in the concept of brain-intestine axis, most scholars find out that the mental and psychological factors are closely related to the occurrence and development of FD. From March of 2016 to March of 2017, we treated 40 FD patients due to liver qi stagnation and spleen deficiency with manual techniques to soothe the liver and circulate qi, and regulate the mind and relieve depression in combination with mosapride citrate dispersible tablets.Now, the report is given as follows.
1 Data and Methods
1.1 Diagnostic criteria
The diagnostic criteria for FD in Western medicine were stipulated in reference to the relevant diagnostic criteria in Roma III[3]. The diagnostic criteria in traditional Chinese medicine were formulated based uponA Consensus on the Diagnosis and Treatment of Functional Dyspepsia by Chinese and Western Medicine(2011)[4].
1.2 Inclusion criteria
In conformity with the above diagnostic criteria; aged from 20 to 60 years old; without organic lesions in the stomach, intestines, liver, gallbladder, spleen and pancreas; having signed the informed consent.
1.3 Exclusion criteria
Those not in conformity with the above diagnostic criteria; those accompanied by other serious diseases of multiple systems or mental disorders; with a history of abdominal operation; under oral administration of other prokinetic agents in recent one week before this experimental treatment.
1.4 Statistical methods
The SPSS 20.0 version statistical software was used for statistical analysis. Chi-square test was used for the non-hierarchical enumeration data. The measurement data were expressed by mean ± standard deviation. The comparison before and after the treatment was processed by pairedt-test, and the comparison between the groups was processed by independent samplet-test. The hierarchical enumeration data were processed by rank-sum test.P<0.05 indicated a statistically significant difference.
1.5 General data
A total of 72 patients in conformity with the diagnostic criteria of FD due to liver qi stagnation and spleen deficiency were recruited from the Second Affiliated Hospital of Hunan University of Chinese Medicine and were divided randomly into an observation group and a control group based upon the random number table, 36 cases in each group. By statistical analysis, the differences in the general data between the two groups were not statistically significant (P>0.05), indicating that the two groups were comparable.

Table 1. Comparison of general data between the two groups
2 Therapeutic Methods
2.1 Observation group
2.1.1 Western medicine
Mosapride citrate dispersible tablets (lot number:160110; specification: 5 mg/tablet, Chengdu Kanghong Pharmaceutical Group Co., Ltd., China), oral administration of 5 mg before meal each time, three times per day, totally for four weeks.
2.1.2 Tuina
Therapeutic principle: Soothing liver to regulate qi and regulating spirit to relieve depression.
Methods: The detailed manipulations were stipulated based upon the relevant literature[5]. After the patient took a supine position, the medical therapist stood at the left side of the patient, and first applied the palm An-pressing manipulation to Zhongwan (CV 12), Qihai(CV 6) and Guanyuan (CV 4), to certain depth, till the patient felt soreness or distension in the back, abdomen and two lower limbs, and then lifted the hand slowly with the patient’s inspiration, for 1-3 min each acupoint(Figure 1). Afterward, applied palm Yun-circular pushing manipulation to Shenque (CV 8) for 3-5 min (Figure 2),and applied finger Tui-pushing manipulation to the line from Juque (CV 14) to Shenque (CV 8) for 3-5 min(Figure 3). After the patient took a prone position, the medical therapist sit at the right side of the patient and Rou-kneaded Ganshu (BL 18) and Danshu (BL 19) with both hands, for 1-3 min each point (Figure 4). Finally,the medical therapist stood at the left side of the patient and applied thumb Tui-pushing manipulation to Baihui (GV 20) and Fengchi (GB 20), for 1-3 min each point (Figure 5). The above manipulations were used alternatively for about 40 min in total. The treatment was given once every other day, for totally four weeks.

Figure 1. An-pressing abdominal points with the palm

Figure 2. Yun-circular pushing Shenque (CV 8) with the palm

Figure 3. Tui-pushing abdominal points with fingers

Figure 4. Rou-kneading points on the back

Figure 5. One-thumb Tui-pushing the points of the head
2.2 Control group
3 Observation of Therapeutic Effects
3.1 Observed items
3.1.1 Score of FD symptoms
The assessment was processed based upon the grading criteria of FD symptoms inA Consensus on the Diagnosis and Treatment of Functional Dyspepsia by Chinese and Western Medicine(2011)[4]. Grade 0, I, II and III were respectively recorded as 0, 3, 5 and 7 points.The higher the point, the severer the symptom.
3.1.2 Score of Chinese version of quality of life questionnaire for functional digestive disorders(Chin-FDDQL)[6]
The quality of the life (QOL) of FD patients was assessed based upon Chin-FDDQL. The total score of Chin-FDDQL was 100 points. The higher the score, the better the patient’s QOL.
3.1.3 Score of Hamilton depression rating scale(HAMD)[7]
Depression severity was assessed by HAMD. The total HAMD score were 76 points. The higher the score, the more serious the patient’s depression.
3.2 Criteria of the therapeutic effects
The criteria were formulated in reference toA Consensus on the Diagnosis and Treatment of Functional Dyspepsia by Chinese and Western Medicine(2011)[4]. The therapeutic effect was evaluated by the above symptoms scores.
Index of the therapeutic effect = (Total scores of the symptoms before the treatment – Total scores of the symptoms after the treatment) ÷ Total scores of the symptoms before the treatment × 100%.
Clinical cure: Symptoms and signs basically disappeared, with the index of the therapeutic effect≥90%, and with no recurrence for over two months.
Remarkable effect: Symptoms and signs were obviously alleviated or relieved by at least 2 grades, or the index of the therapeutic effect was ≥70%, but <90%.
Improvement: Symptoms and signs were alleviated or relieved by at least 1 grade, or the index of the therapeutic effect was ≥30%, but <70%.
Failure: No improvements in the symptoms and signs,and the index of the therapeutic effect was <30%.
3.3 Results
3.3.1 Comparison of clinical effect between the two groups
The total effective rate at the follow-up was 91.7% in the observation group and 75.0% in the control group,without a statistically significant difference between the two groups (P>0.05). The rate of clinical cure and remarkable effect was 66.7% in the observation group,higher than 41.7% in the control group, with a statistical significance in the difference between the two groups(P<0.05), (Table 2).
3.3.2 Comparison of FD symptom score
After the treatment and at the follow-up, the scores of FD symptoms were lower than those before the treatment in both groups, and the intra-group differences were statistically significant in the two groups (allP<0.05). After the treatment and at the follow-up, the scores of FD symptoms were lower in the observation group than those in the control group, and the inter-group differences were statistically significant(allP<0.05), (Table 3).
3.3.3 Comparison of Chin-FDDQL score
After the treatment and at the follow-up, Chin-FDDQL scores were higher than those before the treatment in both groups, and the intra-group differences were statistically significant in the two groups (allP<0.05).After the treatment and at the follow-up, Chin-FDDQL scores were higher in the observation group than those in the control group, and the inter-group differences were statistically significant (allP<0.05), (Table 4).
3.3.4 Comparison of HAMD score
After the treatment and at the follow-up, HAMD scores were lower than those before the treatment in both groups, and the intra-group differences were statistically significant in the two groups (allP<0.05).After the treatment and at the follow-up, HAMD scores were all lower in the observation group than those in the control group, and the inter-group differences were statistically significant (allP<0.05), (Table 5).

Table 2. Comparison of clinical effect between the two groups (case)
Table 3. Comparison of FD symptom score between the two groups

Table 3. Comparison of FD symptom score between the two groups
Note: Ⅰntra-group comparison, 1) P<0.05; inter-group comparison at the same time point, 2) P<0.05
Table 4. Comparison of Chin-FDDQL score between the two groups
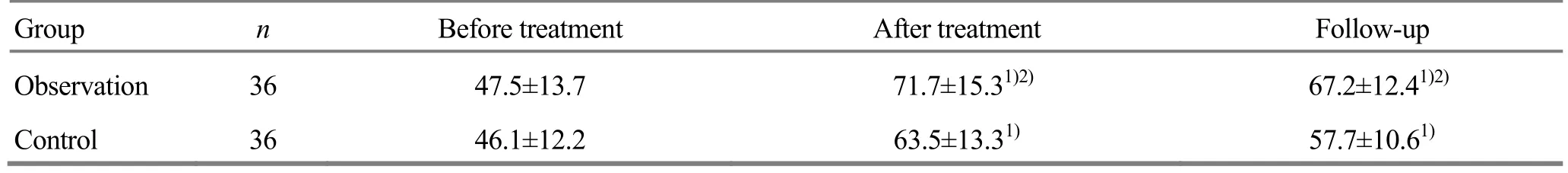
Table 4. Comparison of Chin-FDDQL score between the two groups
Note: Ⅰntra-group comparison, 1) P<0.05; inter-group comparison at the same time point, 2) P<0.05
Table 5. Comparison of HAMD score between the two groups
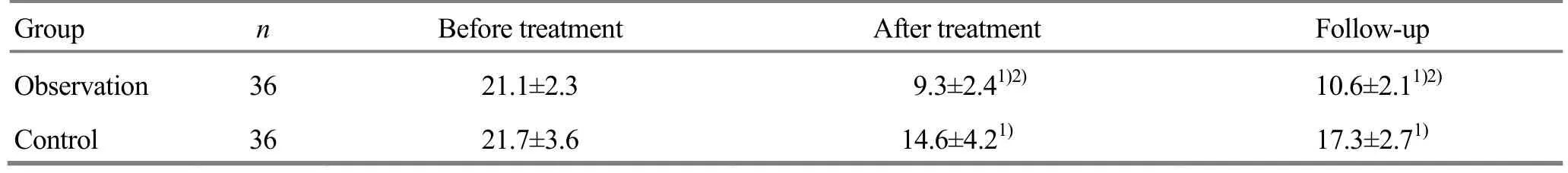
Table 5. Comparison of HAMD score between the two groups
Note: Ⅰntra-group comparison, 1) P<0.05; inter-group comparison at the same time point, 2) P<0.05
4 Discussion
The nerve-endocrine network bridging the enteric nervous system, autonomic nervous system and central nervous system with the stomach and intestine is termed brain-intestine axis. With the brain-gut peptide as messenger, this network serves to regulate the mental status and gastrointestinal motion of the human body in two ways. The dysfunction of brain-intestine axis is currently believed as a core mechanism in the incidence of FD[8]. As a typical somatopsychic disease,its sufferers would be mostly accompanied by mental disorder of anxiety and depression, with the scores of anxiety and depression obviously higher than those of the normal adults[9], and in FD patients complicated with irritable bowel syndrome (IBS), their scores of anxiety and depression are all higher than those of FD patients[10]. Liu HY,et al[11]pointed out that the mental factors of anxiety and depression induced the dysfunction of vegetative nervous system, inhibited the excitement of the sympathetic nerve and vagus nerve,further causing abnormality in the gastrointestinal dynamics.
The pathological position of FD is in the stomach, but it is closely related to the liver and spleen and its pathogenesis is mainly attributed to liver qi stagnation and spleen deficiency[12-13]. Namely, the liver qi stagnation would induce the disorder in the ascending and descending ability of the spleen and stomach, and would further cause discomfort in the stomach and intestines, presenting the relevant gastrointestinal diseases. Therefore, the satisfactory therapeutic effects can be achieved by regulating the mind and emotion of the human body as a supplementary treatment of FD due to liver qi stagnation and spleen deficiency.
Tuina manipulations to soothe the liver, circulate qi,regulate the mind and relieve depression are inherited and created by Prof. Sun Qing from Tianjin University of Traditional Chinese Medicine, based upon the experience of the forefathers, with the five layers of qi and four types of guiding therapies as the theoretic core(Namely, in accordance with the pathologic situation and body constitution of the patients, the manual techniques for reinforcing or reducing purpose are applied in different layers, and the abdomen of the human body is divided into five layers of qi from the shallow position to deep position, and the four types of guiding therapies of attacking, dispersing, lifting and leading skills are formulated based upon the priority of the manual techniques), in combination with multiple manual techniques for the head and abdomen, so as to deal with the causative factor by soothing the liver and circulating qi and to treat the symptoms by regulating the mind and relieving depression, for the clinical treatment of mental disorders[5,14]. In comparison with the traditional manipulations, Prof. Sun Qing’s manipulations are mainly applied to the abdomen and the selected acupoints (mostly locate on the abdomen and back). Shangwan (CV 13), Zhongwan (CV 12),Xiawan (CV 10), Guanyuan (CV 4) and Qihai (CV 6) can be used to regulate qi activity of the middle jiao and strengthen the gastrointestinal dynamics. It has been pointed out in the clinical study that the therapeutic effects are satisfactory in the treatment of FD by tuina on the abdomen, better than Western medicine[15-17],and its mechanism is supposed to relax the abdominal muscles, dilate the intestines and enlarge the intestinal volume for promoting the gastrointestinal peristalsis and digestive secretion of FD patients, and further promote digestion and absorption of food stuffs and excretion[18]. Ganshu (BL 18) and Danshu (BL 19) can soothe the liver, circulate qi and relieve depression.Tuina on Baihui (GV 20) and Fengfu (GV 16) can regulate the mind and improve the spiritual status. It has been indicated by the experiments that acupuncture at the points on the head of the rat can enhance the expression level of the brain-derived neurotrophic factor (BDNF) in the frontal cortex and hippocampus, so as to produce the antidepressant effect[19]. Therefore,tuina on the abdomen in predominance, in combination with tuina on the head, can regulate the gastrointestinal functions and also regulate the central nervous system,more beneficial to the restoration of the normal brain-intestine interactional function.
In this study, the symptoms scores and HAMD scores decreased after the treatment in FD patients of the two groups, all lower than the scores of the same group before the treatment, and Chin-FDDQL scores increased,all higher than the scores of the same group before the treatment, indicating that both of the two therapies can improve the symptoms of indigestion in the patients,relieve the depression and elevate QOL. Moreover, FD symptoms scores, Chin-FDDQL scores and HAMD scores are improved better in the observation group than in the control group, indicating that tuina to soothe the liver, circulate qi, regulate the mind and relieve depression can enhance the therapeutic effect of mosapride citrate dispersible tablets due to a cooperative effect. At the follow-up, the symptom scores and HAMD scores of FD increased somewhat and Chin-FDDQL scores decreased in the two groups, with less change in the observation group than in the control group, indicating that this Tuina method has the effect to stabilize the therapeutic effect of mosapride citrate dispersible tablets. Mosapride citrate dispersible tablets is a typical medication in the treatment of gastrointestinal diseases, but FD is long in its duration and easy to reoccur and is related to the somatopsychic status. Thus, the use of Western medication alone is limited in the therapeutic effect[20]. Therefore, we applied tuina method of ‘soothing liver to regulate qi and regulating spirit to relieve depression’ to treat FD,and the findings indicate that this tuina method plus mosapride citrate dispersible tablet can effectively alleviate the clinical symptoms, enhance QOL and relieve depression of FD patients, and is stable and persistent in the therapeutic effect.
Conflict of Interest
The authors declared that there was no potential conflict of interest in this article.
This work was supported by Science Research Foundation of Hunan Province Education Office (湖南省教育厅科学研究项目,No.15C1056).
Statement of Informed Consent
Ⅰnformed consent was obtained from the patients in this study.
[1] Wang LD, Mao LF, Du XJ, Zhang J, Wu XW. Research progress on functional dyspepsia. Shijie Huaren Xiaohua Zazhi, 2017, 25(1): 84-90.
[2] Ohara S, Kawano T, Kusano M, Kouzu T. Survey on the prevalence of GERD and FD based on the Montreal definition and the Rome Ⅲ criteria among patients presenting with epigastric symptoms in Japan. J Gastroenterol, 2011, 46(5): 603-611.
[3] Tack J, Talley NJ. Functional dyspepsia: symptoms,definitions and validity of the Rome Ⅲ criteria. Nat Rev Gastroenterol Hepatol, 2013, 10(3): 134-141.
[4] Professional Committee on Digestive Diseases, China Society of Ⅰntegrated Traditional Chinese and Western Medicine. A consensus on the diagnosis and treatment of functional dyspepsia by Chinese and Western medicine(2011). Zhongguo Zhongxiyi Jiehe Zazhi, 2011, 31(11):1545-1549.
[5] Xu XY, Sun Q, Zhang W. Professor Sun Qing’s clinical experience of using ‘soothing liver regulating qi and regulating spirit and relieving depression’ of abdominal massage therapy in treating generalized anxiety disorder.Liaoning Zhongyi Zazhi, 2015, 42(7): 1200-1202.
[6] Hou ZK, Mi H, Liu FB, Chen ZQ, Chen XL, Wu YH, Che XL. Ⅰnterpreting the Chinese version of quality of life questionnaire for functional digestive disorders. J Gastroenterol Hepatol, 2017 [doi: 10.1111/jgh.14025, Epub ahead of print].
[7] Liu FY, Zhu LM, Fang XC, Chang M, Chen W, Wang ZF,Shi LL, Xu T. Assessment of anxiety and depression by three psychological screening scales in functional dyspepsia patients. Wei Chang Bing Xue, 2012, 17(2):106-109.
[8] Mao LF, Wang LD, Zhang HW, Liu JH, Du XJ, Peng ZH.Functional dyspepsia and brain-gut peptides. Shijie Huaren Xiaohua Zazhi, 2015, 23(4): 570-576.
[9] Meng M, Liu SN, Zhou B, Wu HM, Liu HM. The relevant research on traditional Chinese medicine patterns of functional dyspepsia with depression and anxiety. Beijing Zhongyiyao, 2011, 30(12): 928-930.
[10] Fan LH, Lin ZZ, Liang PY. The state of anxiety and depression in the patients with functional dyspepsia.Zhongguo Shiyong Yikan, 2013, 40(5): 42-45.
[11] Liu HY, Li ZT. The relationship between anxiety and depression in patients with functional dyspepsia and expression of antrum GAS and SS. Shandong Yiyao, 2016,56(18): 57-58.
[12] Liu JH, Wang LD. Research idea on functional dyspepsia due to liver qi stagnation and spleen deficiency by brain-intestine axis. Zhongguo Zhongxiyi Jiehe Zazhi,2015, 35(6): 755-757.
[13] Zhu LL, Zhao XF, Guo H, Liu Z, Ma SJ. Clinical effect of Jia Wei San Xiang Tang for functional dyspepsia due to liver qi stagnation and spleen deficiency and its influence on anxiety and depression of patient. Zhongyaocai, 2015,38(11): 2442-2444.
[14] Sun Q, Dong H. Theoretical research on generalized anxiety disorder treated by ‘soothing the liver, regulating the spirit and alleviation of mental depression’ abdominal massage method. Tianjin Zhongyiyao Daxue Xuebao, 2011,30(3): 134-136.
[15] Ye FW, Song JL, Lin LQ. Exploration of clinical effectiveness of abdominal tuina in treatment of functional dyspepsia. Shoudu Shipin Yu Yiyao, 2015, 8(16): 86-87.
[16] Zhang DS, Xue WG, Li JH. Clinical observation of abdominal tuina for functional dyspepsia. Beijing Zhongyiyao, 2010, 29(8): 619-621.
[17] Ji SL. Analysis on clinical value of abdominal tuina for functional dyspepsia. Zhongxiyi Jiehe Xinxueguanbing Dianzi Zazhi, 2016, 4(16): 159.
[18] Wu G. Research summary on supplementary tuina therapy for functional dyspepsia. Zhongguo Minzu Minjian Yiyao,2014, 2014, 23(4): 23-24.
[19] Liang J, Lu J, Cui SF, Wang JR, Tu Y. Effect of acupuncture on expression of brain-derived neurotrophic factor gene and protein in frontal cortex and hippocampus of depression rats. Zhen Ci Yan Jiu, 2012, 37(1): 20-24.
[20] Dong ZC, Wang YX, Qi HY. Observation on clinical effect of mosapride citrate dispersible tablets plus Shu Gan Jie Yu capsule and application of medication alone for functional dyspepsia. Xiandai Yufang Yixue, 2012, 39(7): 1848-1850.
 Journal of Acupuncture and Tuina Science2018年2期
Journal of Acupuncture and Tuina Science2018年2期
- Journal of Acupuncture and Tuina Science的其它文章
- Analysis of point-selection pattern in acupuncture-moxibustion treatment of amblyopia
- Clinical observation on cervical chiropractic for cervical spondylosis of vertebral artery type
- Yi Jin Jing (Sinew-transforming Qigong Exercises) for primary osteoporosis in the elderly: a clinical trial
- Effect of acupuncture plus Tai Ji Quan on the recovery of neurological function and depression state in post-stroke depression patients
- Effect of An-pressing manipulation on the serum levels of T-AOC and CK-MM in volunteers with delayed onset muscle soreness in biceps brachii
- Effect of acupuncture in intervening heroin-induced brain damage via regulating ubiquitin-proteasome pathway
