Acute intra-operative brain swelling managed effectively with emergency basal cisternostomy: A case report
Muthanna Noman Abdulqader, Ahmed Hamid Al-Tameemi, Hayder Salih, Samer S. Hoz,Abdullah H. Al Ramadan, Luis Rafael Moscote Salazar
1Department of Neurosurgery, Neurosurgery Teaching Hospital, Baghdad, Iraq
2Department of Neurosurgery, King Faisal Specialist Hospital and Research Centre, Riyadh, Saudi Arabia
3Department of Neurosurgery, Red-Latino-Colombia
1. Introduction
Cisternostomy, a novel technique that incorporates the knowledge of skull base and microvascular surgery, has been recently proposed, and was found to decrease brain swelling, mortality, and morbidity[1,2]. Recently basal cisternostomy has been introduced for management of ICP in TBI with acceptable success rate[3].
We would like to present a case of intra-operative brain swelling during craniotomy for spontaneous intracerebral hemorrhage(ICH) evacuation managed effectively by the implication of basal cisternostomy.
2. Case report
A 56 year old man was found by his wife unconscious in his backyard 30 min after dining together. He was presented after 1 h to the Emergency Department of Neurosurgery Teaching Hospital,Baghdad, Iraq with Glasgow Coma Scale score of 8 (E2M4V2)(Eye response to pain, Motor response is withdrawal and Verbal response is moaning only) and left side weakness (MRC power grade 2 for both upper and lower limbs. His pupils were unequal in size (the right pupil measured 5 mm and the left pupil 3 mm) and were reactive to light.
Initial evaluation was done in the emergency department. His family denied any history of trauma, hypertension or diabetes mellitus and mentioned that he is a right handed person. His blood pressure was extremely high. Blood sample was taken for basic investigations simultaneously and brain CT scan was performed(Figure 1) and revealed sizable right putamenal hemorrhage about 60 mL extending to about 1 cm beneath the cerebral cortex with surrounding edema causing significant midline shift to the left and compresses the ipsilateral lateral ventricle. Effacement of sulci and absence of basal cisterns was noticed. There was no intraventricular extension.
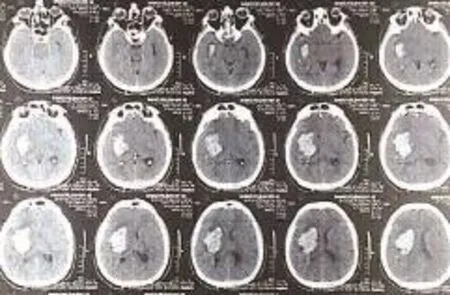
Figure 1. Admission axial brain CT scan shows right putamenal hemorrhage with surrounding edema causing midline shift to the left and compressing the ipsilateral lateral ventricle.Effacement of sulci and compression of basal cisterns was noted with no intraventricular extension.
The surgical decision made to perform hematoma evacuation via craniotomy based on his age, short period of onset, hematoma characteristics (non-dominant hemisphere, significant midline shift, sizable and accessible), progressive symptoms and absence of comorbid diseases. The indications, surgical risks and the expected outcome with and without surgery were discussed with the family and then their consent was taken.
Craniotomy for evacuation of the ICH commenced, dura was opened, cortical incision was made and subtotal hematoma evacuation was done to keep the tamponade effect of the small multiple bleeding sources as expected in such lesion. Meanwhile, the brain started to swell in a rapid fashion and checking the hematoma site did not address a visible cause. Brain relaxation maneuvers were employed such as head elevation, checking the anesthesia parameters and including endotracheal tube kinking, hyperventilation and intravenous mannitol rapid bolus infusion but still, the progressive brain swelling was encountered. Ventricular tap was not possible because the ventricles were already compressed in the pre-operative CT scan.
We decided to perform basal cisternostomy to stop the brain herniation through craniotomy site. Using a surgical loupe (Zeiss 4.3) (usually used in the non-elective setting rather than microscope in our institute), we did cisternostomy of the carotid, inter-optic and proximal sylvian cistern. CSF egress from cistern maintained till the brain became relaxed (the external herniation stopped and the swelling regress over the next 15 min). At this point we continued the procedure as usual with bone flap re-placed again in its primary position after watertight dural closure over non tight brain.
The postoperative course was impressive and the patient consciousness improved over the next few days. Initial postoperative images (Figure 2) showed subtotal hematoma evacuation with reversal of the midline shift. Few days later, the patient discharged home. He was conscious with minimal improvement in the left side power. One year after the surgery, the patient was independent with minimal weakness in his left upper limb and he was already starting a new job as a cashier man in a local restaurant.
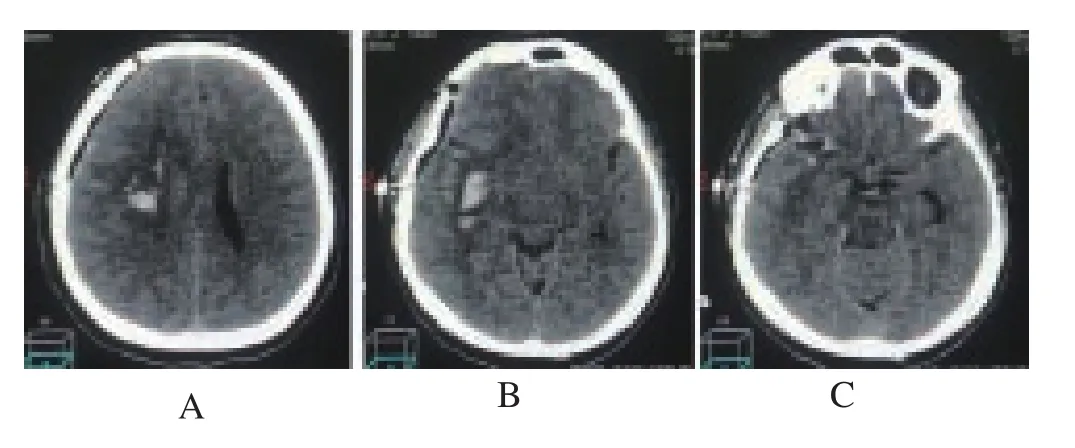
Figure 2. Post-operative brain axial CT scan.Figures 2A and 2B show subtotal hematoma evacuation with reversal of midline shift and bone flap placement in its primary position over a non-tense cortex. Figure 2C shows multiple airoceles in the basal cistern representing the cisternostomy.
3. Conclusion
Taking this case as an example, we can conclude that the cisternostomy alone is one of the effective measures to decrease the intracerebral pressure while facing severe intraoperative brain swelling. As an alternative to the operating microscope, a surgical loupe with optimum magnification and efficient light source can facilitate the procedure and save a very important time in such critical situations. This case demonstrates how intra-operative brain swelling during spontaneous intracerebral hemorrhage evacuation managed effectively with basal cisternostomy.
Conflict of interest statement
The authors declare that they have no conflict of interest.
[1] Cherian I, Bernardo A, Grasso G. Cisternostomy for traumatic brain injury: Pathophysiological mechanisms and surgical technical notes.World Neurosurg2016; 29: 51-57.
[2] Grasso G. Surgical treatment for traumatic brain injury: Is it time for reappraisal?World Neurosurg2015; 84: 594.
[3] Cherian I, Yi G, Munakomi S. Cisternostomy: Replacing the age old decompressive hemicraniectomy?Asian J Neurosurg2013; 8: 132-138.
 Journal of Acute Disease2018年1期
Journal of Acute Disease2018年1期
- Journal of Acute Disease的其它文章
- A case report of acute pulmonary vein stenosis
- Diminazene aceturate modified nanocomposite for improved efficacy in acute trypanosome infection
- Role of first day levels and subsequent trends of serum proteins in acute burns
- Progress in the surgery of rectal cancer
- The laparoscopic approach in emergency surgery: A review of the literature
- Acute myocardial infarction and Yin Yang imbalance
