Solitaire支架血管内机械取栓治疗急性大脑中动脉闭塞效果分析
陈晓辉 钟孟飞 杨志杰 吕在刚 刘梦蕙 李海停 陈秀菊 高宗恩
·急性缺血性卒中血管内治疗·
Solitaire支架血管内机械取栓治疗急性大脑中动脉闭塞效果分析
陈晓辉 钟孟飞 杨志杰 吕在刚 刘梦蕙 李海停 陈秀菊 高宗恩
目的探讨Solitaire支架血管内机械取栓治疗急性大脑中动脉闭塞致缺血性卒中的有效性和安全性,并筛查影响预后的相关因素。方法共25例急性大脑中动脉M1段闭塞致缺血性卒中患者均采用Solitaire支架血管内机械取栓,记录发病至股动脉穿刺时间、股动脉穿刺至血管再通时间、血管内机械取栓次数、取栓前是否静脉溶栓、是否行球囊扩张术和(或)支架植入术、取栓后是否动脉溶栓、术后是否应用替罗非班;术后即刻采用脑梗死溶栓血流分级(TICI)评价血管再通情况,术后24 h采用美国国立卫生研究院卒中量表(NIHSS)评价神经功能,术后90 d采用改良Rankin量表(mRS)评价临床预后;记录术后24 h症状性颅内出血发生率和术后90 d内病死率。结果25例患者发病至股动脉穿刺中位时间5.00(4.00,6.30)h,股动脉穿刺至血管再通中位时间2.00(2.00,2.50)h,血管内机械取栓次数2(2,2)次,7例(28%)先行静脉溶栓再桥接血管内机械取栓,6例(24%)行单纯球囊扩张术,3例(12%)行单纯支架植入术,4例(16%)行球囊扩张术和支架植入术,4例(16%)取栓后行动脉溶栓,11例(44%)术后应用替罗非班;20例(80%)血管再通(TICI分级2b~3级);术后24 h NIHSS评分低于入院时[8(4,12)分对14(11,17)分;Z=-3.532,P=0.000],3例(12%)发生症状性颅内出血;术后90 d 15例(60%)预后良好(mRS评分≤2分),2例(8%)死亡。单因素和多因素前进法Logistic回归分析显示,TICI分级2b~3级是血管内机械取栓预后良好的独立因素(OR=0.316,95%CI:0.102~0.982;P=0.046)。结论Solitair支架血管内机械取栓治疗急性大脑中动脉闭塞致缺血性卒中安全、有效,且大脑中动脉再通级别越高、预后越佳。
卒中; 脑缺血; 大脑中动脉; 血栓切除术; 支架; 血管造影术,数字减影
大脑中动脉(MCA)是颈内动脉(ICA)的直接延续,供血范围包括大脑半球外侧面大部和额顶叶深部结构,主干急性闭塞可以导致对侧肢体瘫痪、感觉障碍等,优势半球受累可以出现失语,严重者发生脑水肿致意识障碍甚至死亡[1]。快速、有效恢复脑组织灌注即血管再通,对预后起决定作用[2]。循证医学证据证实,发病4.50 h内采用重组组织型纤溶酶原激活物(rt-PA)静脉溶栓是治疗急性缺血性卒中的首选方法,但治疗时间窗较窄,且大血管闭塞的再通率较低,如大脑中动脉M1段血管再通率仅为30%[3-4]。越来越多的研究显示,动脉溶栓和血管内机械取栓可以显著提高血管再通率,由静脉溶栓的30%提高至80%~90%,从而改善预后,同时相对延长治疗时间窗[5]。本研究回顾分析25例急性大脑中动脉闭塞致缺血性卒中患者的临床资料,探讨Solitaire支架血管内机械取栓治疗急性大脑中动脉闭塞致缺血性卒中的有效性和安全性,并筛查影响预后的相关因素。
资料与方法
一、临床资料
1.纳入标准 (1)缺血性卒中的诊断符合《中国急性缺血性脑卒中诊治指南2014》[3]。(2)经CTA、MRA和(或)数字减影血管造影术(DSA)证实为大脑中动脉闭塞(MCAO)。(3)年龄>18岁。(4)发病至入院时间<6 h。(5)入院时美国国立卫生研究院卒中量表(NIHSS)评分≥6分。(6)本研究经胜利油田中心医院道德伦理委员会审核批准,所有患者或其家属均知情同意并签署知情同意书。
2.排除标准 参照《中国急性缺血性脑卒中诊治指南2014》[3]中静脉溶栓禁忌证:(1)近3 个月有颅脑创伤史或脑卒中病史。(2)既往有颅内出血病史。(3)蛛网膜下隙出血(SAH)。(4)活动性内出血。(5)颅内肿瘤、颅内动-静脉畸形(AVM)和颅内动脉瘤。(6)近1周曾行不易压迫止血部位的动脉穿刺。(7)近期有颅内手术史或椎管内手术史。(8)血压升高:收缩压≥180 mm Hg(1 mm Hg=0.133 kPa)或者舒张压≥100 mm Hg。(9)有急性出血倾向,包括血小板计数<100×109/L或其他。(10)近48 h内接受肝素治疗[活化部分凝血活酶时间(APTT)超出正常参考值上限]。(11)已服用抗凝药的患者国际标准化比值(INR)>1.70或凝血酶原时间(PT)>15 s。(12)目前正在应用凝血酶抑制剂或凝血因子Xa抑制剂且实验室指标异常。(13)血糖<2.70 mmol/L。(14)头部CT检查显示多个脑叶梗死灶(超过大脑半球的1/3)。
3.一般资料 选择2014年1月-2017年6月在胜利油田中心医院神经内科采用Solitaire支架血管内机械取栓的急性大脑中动脉闭塞致缺血性卒中患者共25例,男性18例,女性7例;年龄37~81岁,平均(58.56±13.91)岁;既往高血压11例(44%),糖尿病4例(16%),心房颤动7例(28%);临床表现为意识障碍、言语障碍、偏瘫、偏身感觉障碍、面舌瘫等;DSA显示,单纯大脑中动脉M1段闭塞21例(84%)、大脑中动脉M1段闭塞合并颈内动脉颅内段串联闭塞4例(16%),左侧大脑中动脉闭塞14例(56%)、右侧闭塞11例(44%);入院时NIHSS评分为9~24分,中位评分14(11,17)分。
二、研究方法
1.Solitaire支架血管内机械取栓 患者仰卧位,于气管插管全身麻醉或质量分数为2%的利多卡因5 ml局部麻醉下,经股动脉穿刺置入8F动脉鞘(美国Medtronic公司),术中DSA明确病变血管并评价侧支代偿情况;再将6F或8F导引导管(美国Medtronic公司)置入颈内动脉C1段,经导引导管注射生理盐水500 ml+肝素1000 U;在微导丝引导下,将Rebar18或Rebar27微导管(美国Medtronic公司)置于大脑中动脉闭塞段远端,经微导管置入Solitaire AB支架或Solitaire FR支架(4~6 mm×15~20 mm,美国Medtronic公司),并于释放支架后静置5 min,与微导管一起回撤,取栓后即刻行DSA检查以观察血管再通情况,必要时可行多次取栓。若取栓后DSA显示血管狭窄率仍≥70%,则行球囊扩张术;若扩张后狭窄段回缩明显或动脉夹层形成,则行支架植入术;若取栓后出现血管再闭塞或血管壁毛糙,则经微导管注入替罗非班或尿激酶动脉溶栓,再行DSA显示血流通畅后方结束手术。如果操作时间>3 h仍未实现血管再通,则终止手术。
2.静脉溶栓 对于发病4.50 h内且符合静脉溶栓指征的患者,先予rt-PA 0.90 mg/kg静脉溶栓治疗,10%rt-PA经静脉注射,余90%于1 h内经静脉滴注,再桥接血管内机械取栓治疗。
3.药物治疗 术后根据血管再通情况酌情静脉泵入替罗非班300 ~ 400 μg/h,维持治疗24 h,复查CT无颅内出血;再予双联抗血小板治疗(阿司匹林100 mg/d和氯吡格雷75 mg/d),连续3个月后改为阿司匹林100 mg/d,长期服用。术后控制收缩压于110~140 mm Hg,入液量维持于2000~3000 ml/d;静脉滴注依达拉奉30 mg/次、2次/d清除自由基,连续治疗10 d。
4.疗效和安全性评价 (1)疗效评价:记录发病至股动脉穿刺时间、股动脉穿刺至血管再通时间、血管内机械取栓次数、取栓前是否静脉溶栓、是否行球囊扩张术和(或)支架植入术、取栓后是否动脉溶栓、术后是否应用替罗非班。术后即刻采用脑梗死溶栓血流分级(TICI)分级[6]评价血管再通情况,2b~3级为血管再通。术后24 h采用NIHSS量表评价神经功能,总评分42分,0~4分,正常或轻度异常;5~15分,中度异常;16~20分,中至重度异常;21~42分,重度异常。术后90 d采用改良Rankin量表(mRS)评价临床预后,≤2分,预后良好;>2分,预后不良。(2)安全性评价:记录术后24 h症状性颅内出血发生率和术后90 d内病死率。症状性颅内出血定义为任意性质的颅内出血且NIHSS评分增加≥4分。
三、统计分析方法
采用SPSS 17.0统计软件进行数据处理与分析。计数资料以相对数构成比(%)或率(%)表示;呈正态分布的计量资料以均数±标准差(x±s)表示;呈非正态分布的计量资料以中位数和四分位数间距[M(P25,P75)]表示,采用Wilcoxon秩和检验。血管内机械取栓预后良好相关因素的筛查,采用单因素和多因素前进法Logistic回归分析。以P≤0.05为差异具有统计学意义。
结 果
本组25例患者发病至股动脉穿刺时间2~8 h,中位时间5.00(4.00,6.30)h;股动脉穿刺至血管再通时间1.50~4.00 h,中位时间2.00(2.00,2.50)h;均完成血管内机械取栓,取栓次数1~3次,中位值2(2,2)次;7例(28%)先行静脉溶栓再桥接血管内机械取栓;6例(24%)行单纯球囊扩张术,3例(12%)行单纯支架植入术,4例(16%)行球囊扩张术和支架植入术;4例(16%)取栓后行动脉溶栓;11例(44%)术后应用替罗非班。25例患者中20例实现完全或部分血管再通(TICI分级2b~3级),血管再通率达80%,其中完全血管再通(TICI分级3级)13例(52%)、部分血管再通(TICI分级2b级)7例(28%)。术后24 h NIHSS评分0~28分,中位评分8(4,12)分,低于入院时的14(11,17)分且差异有统计学意义(Z=-3.532,P=0.000);3例(12%)发生症状性颅内出血。术后均完成90 d随访,15例(60%)预后良好(mRS评分≤2分),0分者2例(8%)、1分者7例(28%)、2分者6例(24%),10例(40%)预后不良(mRS评分>2分),3分5例(20%)、4分1例(4%)、5分2例(8%);2例(8%)死亡,1例为症状性颅内出血、1例为再灌注损伤致脑疝形成。
进一步探讨血管内机械取栓预后良好的相关因素,以预后良好作为因变量,性别、年龄、既往史(高血压、糖尿病、心房颤动)、入院时NIHSS评分、发病至股动脉穿刺时间、股动脉穿刺至血管再通时间、血管内机械取栓次数、取栓前行静脉溶栓、行球囊扩张术和(或)支架植入术、取栓后行动脉溶栓、术后应用替罗非班、TICI分级为自变量,行单因素Logistic回归分析,结果显示,TICI分级2b~3级是血管内机械取栓预后良好的相关因素(P=0.046;表1,2);将TICI分级纳入多因素Logistic回归方程,结果显示,TICI分级2b~3级是血管内机械取栓预后良好的独立因素(OR=0.316,95%CI:0.102~0.982,P=0.046;表3)。
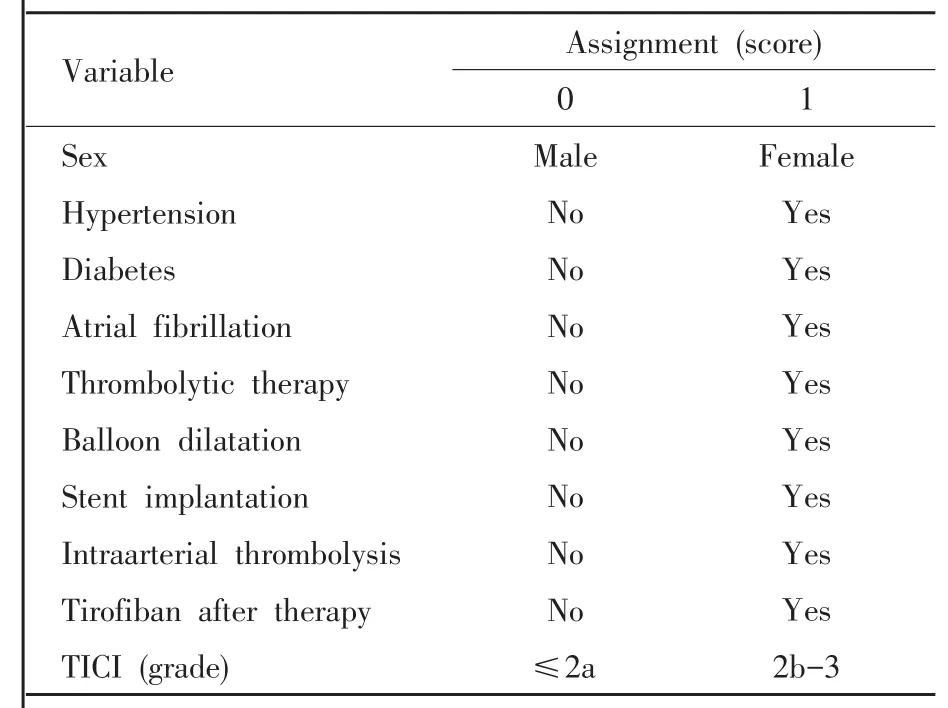
表1 血管内机械取栓预后良好相关因素变量赋值表Table 1. Variable assignment of relevant factors of favorable prognosis on thrombectomy
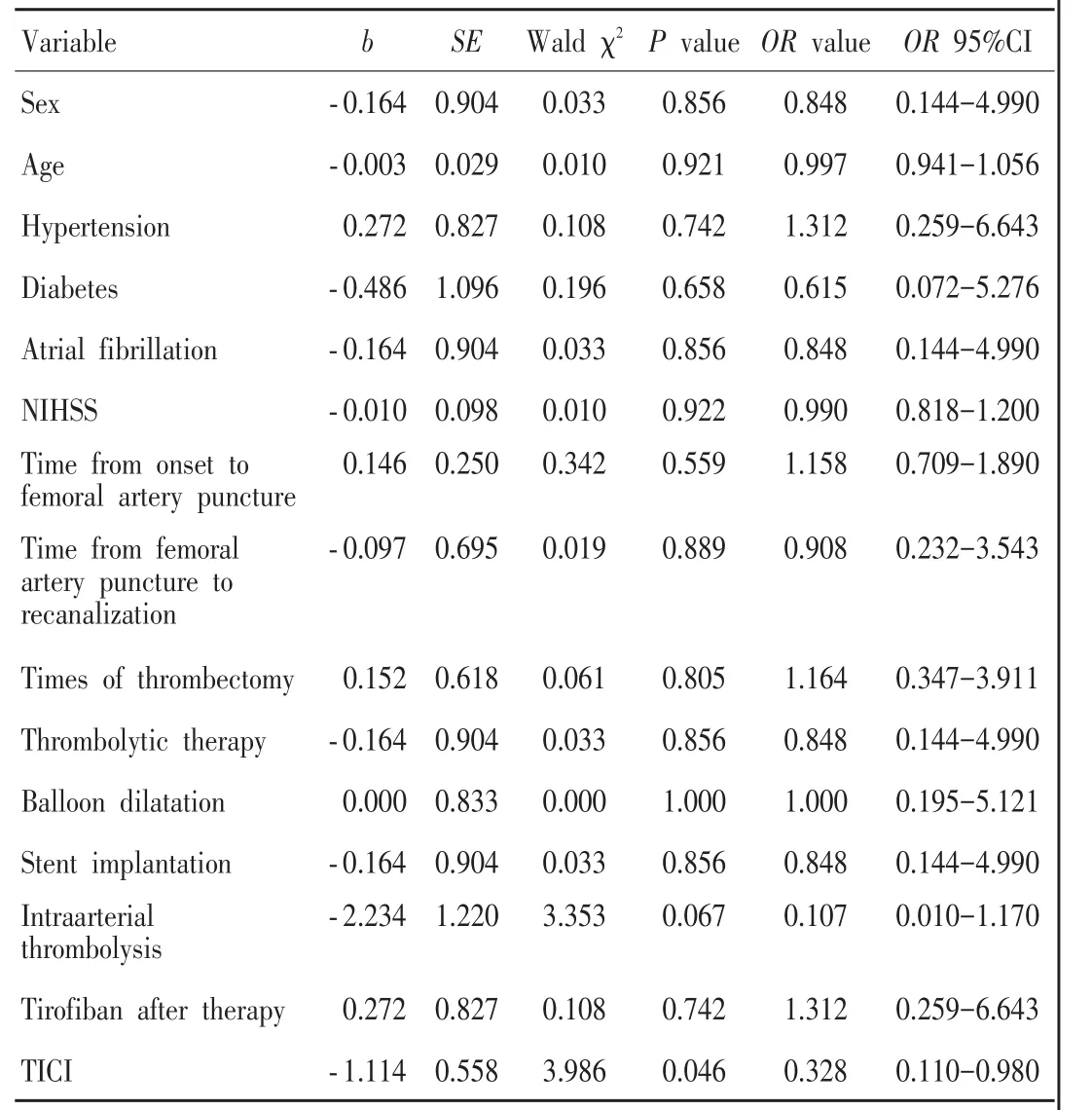
表2 血管内机械取栓预后良好相关因素的单因素Logistic回归分析Table 2. Univariate Logistic regression analysis of relevant factors of favorable prognosis on thrombectomy
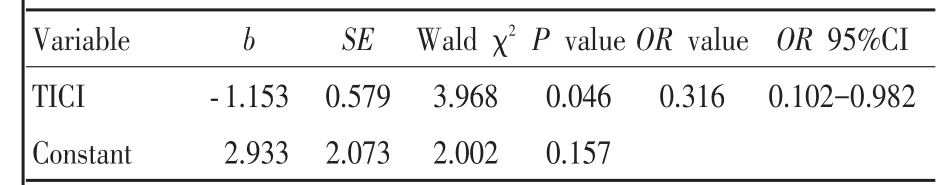
表3 血管内机械取栓预后良好相关因素的多因素前进法Logistic回归分析Table3. Relevant factors of good prognosis on endovascular thrombectomy by multivariate forward Logistic regression analysis
典型病例
患者 男性,74岁,因意识障碍、四肢抽搐3 h,于2013年10月11日入院。患者3 h前无明显诱因突发意识障碍,呼之不应,伴四肢抽搐,遂急诊入院。既往有冠心病、心房颤动和脑卒中病史,但未遗留后遗症,余无特殊。入院后体格检查:血压145/90 mm Hg,嗜睡,言语欠流利,双侧瞳孔等大、等圆,直径约3 mm,双眼向右侧凝视,左侧鼻唇沟浅,伸舌不合作,左侧肢体肌力0级、肌张力降低,右侧肢体疼痛刺激有回缩动作,感觉和共济运动检查不合作,左侧Babinski征阳性、右侧阴性,脑膜刺激征阴性,Kernig征阴性。入院时NIHSS评分14分。头部MRI显示,右侧侧脑室旁急性梗死灶(图1a);MRA显示,右侧大脑中动脉M1段闭塞(图1b)。于入院后4.50 h行DSA检查,显示右侧大脑中动脉M1段闭塞,远端显影良好(图2),遂予血管内机械取栓,采用Solitaire AB支架取栓1次即成功取出血栓,术后未应用替罗非班。患者于入院后5.50 h实现完全血管再通(TICI分级3级)。术后即刻左侧肢体肌力恢复至3级。术后24 h复查MRI和MRA显示,右侧大脑中动脉完全再通(图3)。患者共住院14 d,出院时NIHSS评分为5分。出院后继续康复治疗,术后90 d随访时mRS评分1分。
讨 论
2015年,N Engl J Med发表5项血管内治疗大血管闭塞致急性缺血性卒中的前瞻性多中心随机对照临床试验,包括血管内治疗急性缺血性卒中的多中心随机临床试验(MR CLEAN)[5]、延长急性神经功能缺损至动脉内溶栓时间的临床试验(EXTEND-IA)[7]、前循环近端闭塞小病灶性卒中的血管内治疗并强调最短化CT扫描至再通时间临床试验(ESCAPE)[8]、血管内机械取栓作为急性缺血性卒中血管内主要治疗试验(SWIFT PRIME)[9]、西班牙8小时内支架取栓与内科治疗随机对照试验(REVASCAT)[10],使血管内治疗成为治疗大血管闭塞致急性缺血性卒中的“新标准”[11]。同年,美国心脏协会(AHA)/美国卒中协会(ASA)更新急性缺血性卒中血管内治疗指南,将血管内机械取栓联合静脉溶栓治疗急性前循环大血管闭塞致缺血性卒中列为Ⅰ类推荐、A级证据[12]。随即我国也发表《急性缺血性卒中血管内治疗中国指南2015》[13]。
然而上述循证医学证据均来自欧美国家,而作为脑卒中发病率较高的中国,目前的循证医学证据仍较少。本研究采用Solitaire支架血管内机械取栓治疗大脑中动脉闭塞致急性缺血性卒中,血管再通率高达80%(20/25),术后90天随访时预后良好率达 60%(15/25),与国内其他研究相符[14-16],表明Solitaire支架血管内机械取栓可以快速、有效恢复脑组织灌注,改善临床预后。本研究有2例死亡患者,1例术前DSA显示左侧颈内动脉末段闭塞,血栓延伸至左侧大脑中动脉M1段,采用Solitaire AB支架取栓2次后TICI分级达3级,但血管再通后发生缺血-再灌注损伤,导致脑疝形成,死亡;1例术前DSA显示左侧颈内动脉末段至大脑中动脉M1段闭塞,血栓负荷量较大,采用Solitaire支架多次取栓联合球囊扩张术仍未实现血管再通,术后发生症状性颅内出血,死亡。进一步探讨血管内机械取栓预后良好的相关因素,单因素和多因素前进法Logistic回归分析显示,仅血管再通级别高(TICI分级2b~3级)是预后良好的独立因素。

图1 术前头部影像学检查所见1a 横断面DWI显示,右侧侧脑室旁急性梗死灶(箭头所示) 1b MRA显示,右侧大脑中动脉M1段闭塞(箭头所示)Figure 1 Preoperative head imaging findings Axial DWI showed acute infarction beside the right lateral ventricle(arrow indicates,Panel 1a).MRA showed right MCA-M1 segment occlusion(arrow indicates,Panel 1b).
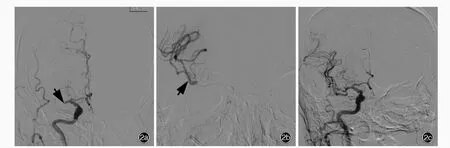
图2 DSA检查所见 2a 术前可见右侧大脑中动脉M1段闭塞(箭头所示) 2b 术中可见右侧大脑中动脉远端显影良好(箭头所示) 2c 采用Solitaire AB支架取栓1次即成功取出血栓,术后即刻可见血管再通Figure 2 DSA findings Right MCA-M1 segment occlusion was found before therapy(arrow indicates,Panel 2a).Visualization of distal right MCA was good(arrow indicates,Panel 2b).Thrombectomy with Solitaire AB stent was successful for one time,and right MCA was recanalized immediately(Panel 2c).
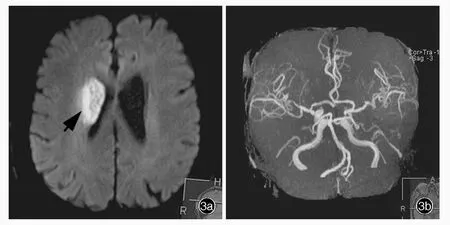
图3 术后24 h复查头部影像学所见 3a 横断面DWI显示,右侧侧脑室旁急性梗死灶较术前无扩大(箭头所示) 3b MRA显示右侧大脑中动脉完全再通Figure 3 Head imaging findings 24 h after therapy Axial DWI showed acute infarction beside the right lateral ventricle was not enlarged compared to preoperation (arrow indicates,Panel 3a). MRA showed successful recanalization of right MCA(Panel 3b).
多项指南和临床研究均提出,发病至血管再通时间是影响预后的相关因素[5]。本研究发病至股动脉穿刺中位时间5.00(4.00,6.30)小时,股动脉穿刺至血管再通中位时间2.00(2.00,2.50)小时,但单因素和多因素前进法Logistic回归分析并未得出血管再通时间与预后存在相关性,可能与本研究样本量较小致统计偏倚有关。本研究术后24小时NIHSS评分[8(4,12)分]低于入院时[14(11,17)分]且差异有统计学意义,表明神经功能好转,提示及时、有效的血管再通可以明显改善神经功能。
此外,研究显示,前循环缺血性卒中血管内治疗后颅内出血风险较后循环缺血性卒中高,可能与颅内血管解剖学结构有关[17]:(1)大脑中动脉M1段垂直发出多条豆纹动脉,承受的血流压力较大,易出血。(2)取栓支架易对血管壁造成机械性损伤,尤其是取栓次数>3次时。本研究仅3例发生症状性颅内出血,可能与取栓次数较少有关。
尽管本研究取得良好效果,但是作为小样本回顾性研究,在术前适应证选择、操作技术、围手术期处理和并发症预防等方面仍有待改进,以提高血管内机械取栓的有效性、降低并发症发生率。
[1]Wu J.Neurology.2nd ed.Beijing:People's Medical Publishing House,2005:896[.吴江.神经病学.2版.北京:人民卫生出版社,2005:896.]
[2]Kharitonova TV,Melo TP,Andersen G,Egido JA,Castillo J,Wahlgren N;SITS Investigators.Importance of cerebral artery recanalization in patients with stroke with and without neurological improvement after intravenous thrombolysis.Stroke,2013,44:2513-2518.
[3]Cerebrovascular Disease Study Group,Chinese Society of Neurology,Chinese Medical Association.Chinese guidelines for diagnosis and treatment of acute ischemic stroke (2014).Zhonghua Shen Jing Ke Za Zhi,2015,48:246-257[.中华医学会神经病学分会;中华医学会神经病学分会脑血管病学组.中国急性缺血性脑卒中诊治指南2014.中华神经科杂志,2015,48:246-257.]
[4]Bhatia R,Hill MD,Shobha N,Menon B,Bal S,Kochar P,Watson T,Goyal M,Demchuk AM.Low rates of acute recanalization with intravenous recombinant tissue plasminogen activator in ischemic stroke:real-world experience and a call for action.Stroke,2010,41:2254-2258.
[5]Berkhemer OA,Fransen PS,Beumer D,van den Berg LA,Lingsma HF,Yoo AJ,Schonewille WJ,Vos JA,Nederkoorn PJ,Wermer MJ,van Walderveen MA,Staals J,Hofmeijer J,van Oostayen JA,Lycklama à Nijeholt GJ,Boiten J,Brouwer PA,Emmer BJ,de Bruijn SF,van Dijk LC,Kappelle LJ,Lo RH,van Dijk EJ,de Vries J,de Kort PL,van Rooij WJ,van den Berg JS,van Hasselt BA,Aerden LA,Dallinga RJ,Visser MC,Bot JC,Vroomen PC,Eshghi O,Schreuder TH,Heijboer RJ,Keizer K,Tielbeek AV,den Hertog HM,Gerrits DG,van den Berg-Vos RM,Karas GB,Steyerberg EW,Flach HZ,Marquering HA,Sprengers ME,Jenniskens SF,Beenen LF,van den Berg R,Koudstaal PJ,van Zwam WH,Roos YB,van der Lugt A,van Oostenbrugge RJ,Majoie CB,Dippel DW;MR CLEAN Investigators.A randomized trial of intraarterial treatment for acute ischemic stroke.N Engl J Med,2015,372:11-20.
[6]Zaidat OO,Yoo AJ,Khatri P,Tomsick TA,von Kummer R,Saver JL,Marks MP,Prabhakaran S,Kallmes DF,Fitzsimmons BF,Mocco J,Wardlaw JM,Barnwell SL,Jovin TG,Linfante I,Siddiqui AH,Alexander MJ,Hirsch JA,Wintermark M,Albers G,Woo HH,Heck DV,Lev M,Aviv R,Hacke W,Warach S,Broderick J,Derdeyn CP,Furlan A,Nogueira RG,Yavagal DR,Goyal M,Demchuk AM,Bendszus M,Liebeskind DS;Cerebral Angiographic Revascularization Grading(CARG)Collaborators,STIR Revascularization Working Group,STIR Thrombolysis in Cerebral Infarction(TICI)Task Force.Recommendations on angiographic revascularization grading standards for acute ischemic stroke:a consensus statement.Stroke,2013,44:2650-2663.
[7]Campbell BC,Mitchell PJ,Kleinig TJ,Dewey HM,Churilov L,Yassi N,Yan B,Dowling RJ,Parsons MW,Oxley TJ,Wu TY,Brooks M,Simpson MA,Miteff F,Levi CR,Krause M,Harrington TJ,Faulder KC,Steinfort BS,Priglinger M,Ang T,Scroop R,Barber PA,McGuinness B,Wijeratne T,Phan TG,Chong W,Chandra RV,Bladin CF,Badve M,Rice H,de Villiers L,Ma H,Desmond PM,Donnan GA,Davis SM;EXTEND-IA Investigators.Endovascular therapy for ischemic stroke with perfusion-imaging selection.N Engl J Med,2015,372:1009-1018.
[8]Goyal M,Demchuk AM,Menon BK,Eesa M,Rempel JL,Thornton J,Roy D,Jovin TG,Willinsky RA,Sapkota BL,Dowlatshahi D,Frei DF,Kamal NR,Montanera WJ,Poppe AY,Ryckborst KJ,Silver FL,Shuaib A,Tampieri D,Williams D,Bang OY,Baxter BW,Burns PA,Choe H,Heo JH,Holmstedt CA,Jankowitz B,Kelly M,Linares G,Mandzia JL,Shankar J,Sohn SI,Swartz RH,Barber PA,Coutts SB,Smith EE,Morrish WF,Weill A,Subramaniam S,Mitha AP,Wong JH,Lowerison MW,Sajobi TT,Hill MD;ESCAPE Trial Investigators.Randomized assessment of rapid endovascular treatment of ischemic stroke.N Engl J Med,2015,372:1019-1030.
[9]Saver JL,Goyal M,Bonafe A,Diener HC,Levy EI,Pereira VM,Albers GW,Cognard C,Cohen DJ,Hacke W,Jansen O,Jovin TG,Mattle HP,Nogueira RG,Siddiqui AH,Yavagal DR,Baxter BW,Devlin TG,Lopes DK,Reddy VK,du Mesnil de Rochemont R,Singer OC,Jahan R;SWIFT PRIME Investigators.Stent-retriever thrombectomy after intravenous t-PA vs t-PA alone in stroke.N Engl J Med,2015,372:2285-2295.
[10]Jovin TG,Chamorro A,Cobo E,de Miquel MA,Molina CA,Rovira A,San Román L,Serena J,Abilleira S,Ribó M,Millán M,Urra X,Cardona P,López-Cancio E,Tomasello A,Castaño C,Blasco J,Aja L,Dorado L,Quesada H,Rubiera M,Hernandez-Pérez M,Goyal M,Demchuk AM,von Kummer R,Gallofré M,Dávalos A;REVASCAT Trial Investigators.Thrombectomy within 8 hours after symptom onset in ischemic stroke.N Engl J Med,2015,372:2296-2306.
[11]Ding D.Endovascular mechanical thrombectomy for acute ischemic stroke:a new standard of care.J Stroke,2015,17:123-126.
[12]Powers WJ,Derdeyn CP,Biller J,Coffey CS,Hoh BL,Jauch EC,Johnston KC,Johnston SC,Khalessi AA,Kidwell CS,Meschia JF,Ovbiagele B,Yavagal DR;American Heart Association Stroke Council.2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment:a guideline for healthcare professionals from the American Heart Association/American Stroke Association.Stroke,2015,46:3020-3035.
[13]Chinese Apoplexy Society,Chinese Apoplexy Society Neural Intervention Branch,Chinese Academy of Preventive Medicine Stroke Prevention and Control Professional Committee Intervention Group.Chinese guidelines of endovascular treatment for acute ischemic stroke(2015).Zhongguo Zu Zhong Za Zhi,2015,10:590-606[.中国卒中学会,中国卒中学会神经介入分会,中华预防医学会卒中预防与控制专业委员会介入学组.急性缺血性卒中血管内治疗中国指南2015.中国卒中杂志,2015,10:590-606.]
[14]Li GL,Du SW,Li JW,Yan F,Xiang SS,Chen J,Zhang HQ.Effect analysis of Solitaire FR stent mechanical thrombectomy combined with 5F Navien catheter aspiration technique for the treatment of acute middle cerebral artery occlusion.Zhongguo Nao Xue Guan Bing Za Zhi,2017,14:37-42[.李桂林,杜世伟,李静伟,闫峰,向思诗,陈健,张鸿祺.Solitaire FR直接机械取栓联合5F Navien导管抽吸技术治疗大脑中动脉急性闭塞的效果分析.中国脑血管病杂志,2017,14:37-42.]
[15]Wang HS,Liu S,Zhao LB,Zhou CG,Xia JG,Zu QQ,Shi HB.Solitaire AB stent thrombectomy for the treatment of acute middle cerebral artery occlusion:analysis of curative effect.Jie Ru Fang She Xue Za Zhi,2015,24:658-661[.王洪生,刘圣,赵林波,周春高,夏金国,祖庆泉,施海彬.Solitaire AB型支架取栓治疗急性大脑中动脉栓塞疗效分析.介入放射学杂志,2015,24:658-661.]
[16]Peng Y,Xuan JG,Chen RH,Zhu XC,Yang YL.Thrombectomy with Solitaire AB stent in the treatment of acute middle cerebral artery occlusion:eight cases report.Zhongguo Nao Xue Guan Bing Za Zhi,2011,8:373-377[.彭亚,宣井岗,陈荣华,朱旭成,杨伊林.Solitaire AB支架取栓术治疗急性大脑中动脉闭塞八例.中国脑血管病杂志,2011,8:373-377.]
[17]Novakovic RL,Toth G,Narayanan S,Zaidat OO.Retrievable stents,"stentrievers,"for endovascular acute ischemic stroke therapy.Neurology,2012,79:148-157.
Thrombectomy with Solitaire stent for treating acute middle cerebral artery occlusion
CHEN Xiao-hui,ZHONG Meng-fei,YANG Zhi-jie,LÜ Zai-gang,LIU Meng-hui,LI Hai-ting,CHEN Xiu-ju,GAO Zong-en
Department of Neurology,Shengli Oilfield Central Hospital,Dongying 257034,Shandong,China
Corresponding author:GAO Zong-en(Email:gaozongen@126.com)
ObjectiveTo assess the efficacy and safety of thrombectomy with Solitaire stent for treatment of acute middle cerebral artery occlusion(MCAO),and to identify the predictive factors for clinical outcome.MethodsA total of 25 patients with acute middle cerebral artery(MCA)-M1 segment occlusion were treated by thrombectomy with Solitaire stent.Time from onset to femoral artery puncture,time from femoral artery puncture to recanalization,times of thrombectomy,thrombolytic therapy or not,balloon dilatation and/or stent implantation,intraarterial thrombolysis or not,tirofiban treatment after therapy or not were recorded.Vascular recanalization immediately after procedure was evaluated by Thrombolysis in Cerebral Infarction(TICI).National Institutes of Health Stroke Scale(NIHSS)was used to evaluate neurological function of patients 24 h after operation,and the clinical outcomes were assessed by modified Rankin Scale(mRS)at 90 d after treatment.The occurrence rate of symptomatic intracranial hemorrhage within 24 h after operation and mortality within 90 d after treatment were recorded.ResultsMedian time from onset to femoral artery puncture was 5.00(4.00,6.30)h;median time from femoral artery puncture to recanalization was 2.00(2.00,2.50)h;times of thrombectomy was 2(2,2);7 patients(28%)received intravenous thrombolysis before thrombectomy;6 patients(24%)underwent balloon dilatation only;3 patients(12%)underwent stent implantation only;4 patients(16%)underwent balloon dilatation and stent implantation;4 patients(16%)received intraarterial thrombolysis after thrombectomy;11(44%)received tirofiban therapy after operation.There were 20 patients(80%)of recanalization with TICI 2b-3 grade.The NIHSS score at 24 h after operation was significantly decreased than before procedure[8(4,12)score vs.14(11,17)score;Z=-3.532,P=0.000].Symptomatic intracranial hemorrhage occurred in 3 patients(12%).At 90 d after treatment,15 patients(60%)had favorable prognosis(mRS≤2 score).Two patients(8%)died.Univariate and multivariate forward Logistic regression analysis showed the TICI 2b-3 grade was independent factor for favorable prognosis(OR=0.316,95%CI:0.102-0.982;P=0.046).ConclusionsThrombectomy with Solitaire stent is safe and effective for treating acute MCAO.With the increase of TICI grade,the prognosis is better.
Stroke; Brain ischemia; Middle cerebral artery; Thrombectomy; Stents;Angiography,digital subtraction
This study was supported by National Scientific and Technical Support Program(No.2011BAI08B07).
10.3969/j.issn.1672-6731.2017.11.004
国家科技支撑项目(项目编号:2011BAI08B07)
257034东营,胜利油田中心医院神经内科
高宗恩(Email:gaozongen@126.com)
2016-10-29)
·小词典·
中英文对照名词词汇(二)
急性前循环缺血性卒中血管内治疗登记Endovascular Treatment for Acute Anterior Circulation Ischemic Stroke Registry(ACTUAL)
简易智能状态检查量表Mini-Mental State Examination(MMSE)
交感皮肤反应 sympathetic skin response(SSR)
胶质纤维酸性蛋白 glial fibrillary acidic protein(GFAP)角膜神经分支密度 corneal nerve branch density(CNBD)角膜神经纤维长度 corneal nerve fiber length(CNFL)
角膜神经纤维密度 corneal nerve fiber density(CNFD)
接触性热痛诱发电位contact-heat-evoked potential(CHEP)结蛋白 desmin(Des)
⑨对异化概念的理解,有两个基本的前提或出发点:一是生产商品的具体劳动与抽象劳动相分离,私人劳动与社会劳动相分离,二是劳动者与劳动的客观条件相分离.
经颅多普勒超声 transcranial Doppler ultrasonography(TCD)颈内动脉 internal carotid artery(ICA)
颈总动脉 common carotid artery(CCA)径向扩散率 radial diffusivity(RD)
静脉注射免疫球蛋白 intravenous immunoglobulin(IVIg)
聚乳酸羟基乙酸 polylactic-co-glycolic acid(PLGA)
抗神经节苷脂抗体 anti-ganglioside antibody(AGA)
可逆性胼胝体压部病变综合征reversible splenial lesion syndrome(RESLES)
扩散张量成像 diffusion tensor imaging(DTI)
临床痴呆评价量表 Clinical Dementia Rating Scale(CDR)
颅内动脉粥样硬化性狭窄intracranial atherosclerotic stenosis(ICAS)
路易体痴呆 dementia with Lewy bodies(DLB)
路易小体 Lewy body(LB)
卵泡刺激素 follicle stimulating hormone(FSH)
美国国立卫生研究院卒中量表National Institutes of Health Stroke Scale(NIHSS)
美国介入和治疗性神经放射学学会/美国介入放射学学会American Society of Interventional and Therapeutic Neuroradiology/Society of Interventional Radiology(ASITN/SIR)
美国介入和治疗性神经放射学学会/美国介入放射学学会侧支循环分级系统American Society of Interventional and Therapeutic Neuroradiology/Society of Interventional Radiology Collateral Flow Grading System(ASITN/SIR ACG)
美国心脏协会 American Heart Association(AHA)