Linking anger trait with somatization in low-grade college students: Moderating roles of family cohesion and adaptability
Liang LIU, Cuilian LIU, Xudong ZHAO
•Original research article•
Linking anger trait with somatization in low-grade college students: Moderating roles of family cohesion and adaptability
Liang LIU1,2*, Cuilian LIU3, Xudong ZHAO2
family cohesion, family adaptability, family conflict, anger proneness, anger trait, moderation,somatization
1. Introduction
Somatization is commonly described as physical symptoms that have no medical basis or are discordant with the degree of illness indicated by objective tests or observable signs. Previous research showed that between 22% and 58% of patients in primary care settings complain of medically unexplained symptoms [1]and the prevalence of somatization disorders was between 2.1% to 5.8% for different ethnicities.[2]Clarifying the factors that contribute to the development and maintenance of somatic symptoms and the pathways from those risk and protecting factors to somatization has the potential to contribute to the design of suitable treatment strategies for individuals with somatic complaints.
Anger trait and somatization
Anger trait, as defined by Spielberger et al.[3], is a tendency to experience angry feelings and is thought to be a relatively stable personality characteristic. A wider range of situations are easier to be perceived by individuals high in anger trait as anger eliciting. These people tend to experience more persistent anger during these situations than do individuals with low anger trait.Prior research has suggested that anger trait is empirically linked with the development and maintenance of somatic complaints. Liu and colleagues surveyed 109 couples, and found that proneness to experience anger is associated with somatic symptoms reporting.[4]In a study of 105 patients who survived myocardial infarction, positive association between distressed personality and somatization has been reported. As defined by Denollet and colleagues,individuals with distressed personality tend to experience anger and other negative emotions.[5-7]Jellesma’s research demonstrated that adolescents classified as having distressed personalities reported more recent somatic complaints than those with other personality traits.[8]
Family function and somatic symptoms
Associations between original family functions and individual somatic complaints have been established theoretically and empirically by prior studies.[9]Minuchin et al. defined the dynamic of psychosomatic families as boundary confusion, rigid behavioral control, and poor adaptability.[10]In an observation of 120 somatic patients, Obimakinde et al. reported the correlations of somatization with disrupted marriage,low social status and financial constraints.[11]Brown et al. found that somatization disorder patients reported significantly more family conflict and less family cohesion than comparison subjects.[12]Similarity,association between chronic pain and lower family cohesion has also been marked.[13]
Family function in the path from anger trait to somatization
A number of studies and theories have assessed the prediction that somatic symptoms are associated with anger trait and original family environment. However,for young adults high in anger trait, the role that family circumstance plays in the link from anger trait to somatization still remains unclear. According to family therapy theory, family function and dynamics do not just contribute etiologically to psychosomatic symptoms, but also play a role in its maintenance.[10,14]
The present cross-sectional study, in a sample of under-graduate students, examines family cohesion and family adaptability as moderators of the association between anger trait and reports of physical symptoms commonly associated with somatization. We tried to test whether the variances in family cohesion and adaptability would affect the strength of the relations between anger trait and somatization. In contrast to the majority of prior studies that have been restricted to clinical samples, which are likely to have higher levels of medical illness, a college sample offers the advantages of examining links between family environment, anger trait and somatization in people drawn from a spectrum of normal health statuses.
In research on somatization, an ever-present concern is how to distinguish symptoms that indicate physical disease from symptoms that are medically unexplained. In the present study, the terms ‘somatization’ and ‘somatic symptoms’ are used to indicate physical symptoms without medical explanation, with the understanding that our ability to differentiate symptoms with and without physical basis is imperfect. In addition, several factors that have been linked to both medical illness and somatization are also controlled: age, gender, socioeconomic status and onechild family.[4,11,15,16]Finally, we examined current levels of depression and anxiety both because depression and anxiety are commonly associated with somatization and anger experience,[4,17,18,19]and because depressive symptoms may bias participants toward more negative responses to other assessments, including inventories of physical symptoms.[20]
2. Methods
2.1 Participants
2600 college students in one university from Shanghai were invited to participate in the study from Feb to May 2015. 46 students (2%) refused participation and 18 subjects (0.1%) were excluded due to physical disease (diagnosed by physicians) or mental health disorders (screened by at least 2 psychiatrists according to ICD-10). Thus, 2536 students (96%) were enrolled in the study. Written informed consent was signed by each participant at the beginning of thestudy. Participants finished questionnaires including measurements that assessed their demographic data,anger trait, family cohesion, family adaptability and health symptoms including somatization, depression,anxiety, phobia and obsession. The effective response sample was 2008 participants (1128 male and 880 female) which accounted for effective rate of 79%. This study was approved by the institutional review board of Tongji University School of Medicine.
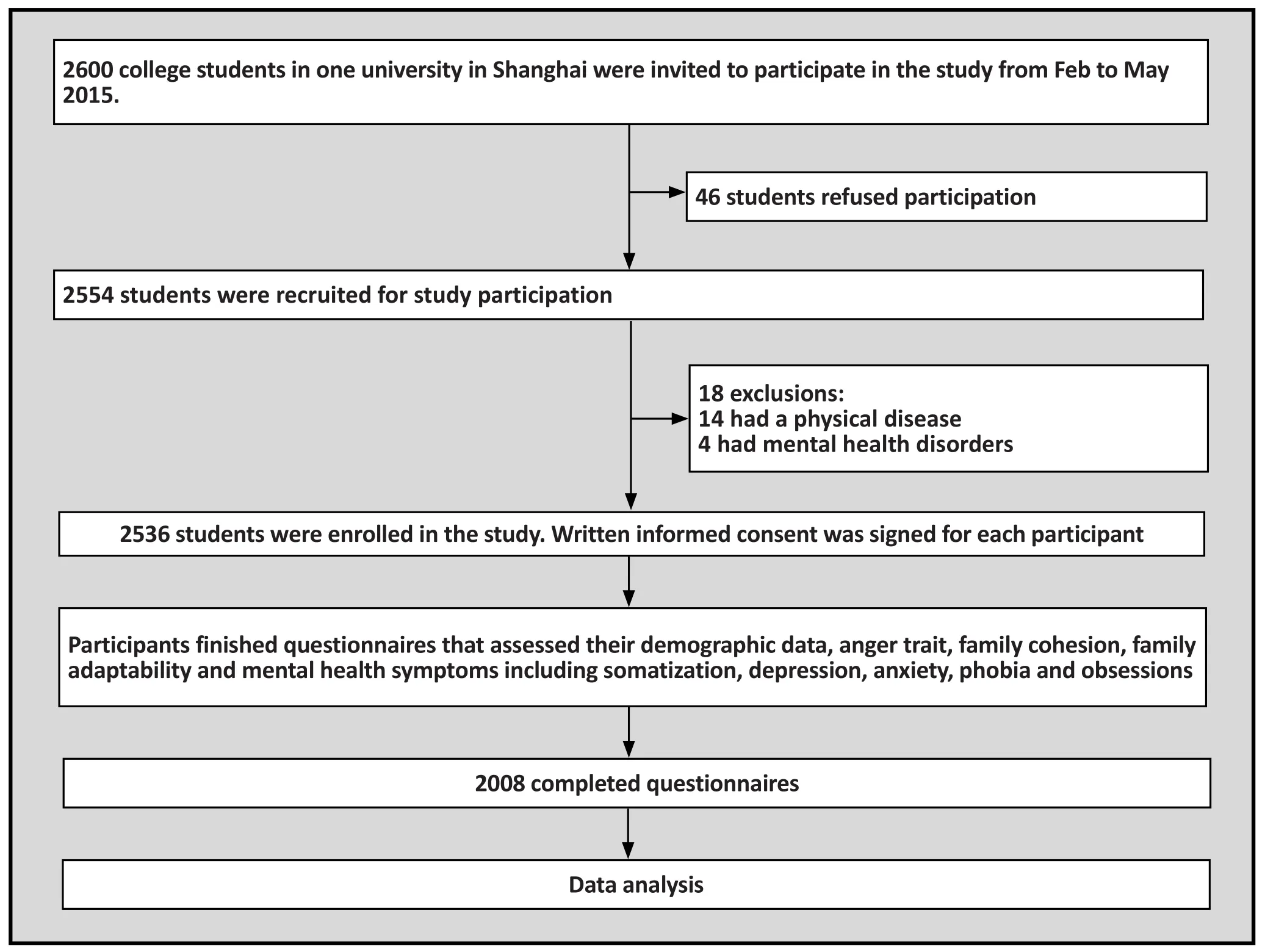
Figure 1. Flow chart of the study
2.2 Measures
2.2.1 Demographics
Information regarding age, gender, grade, major, family economic status, ethnicity, education level of parents and being in a one-child family or not were obtained using written questionnaires. Mean age of the participants was 19.8 years (SD = 0.9). 89.6% were ethnically Han Chinese and 10.4% were a Chinese ethnic minority. With respect to family economic status, 19% of participants indicated their status was good, 78.1 % normal and 12.7% reported a poor economic status. 1477 (73.6%) students came from one-child families. 51.6 % of the participants were freshmen and 47.6% were sophomores.
2.2.2 Somatic and depression symptoms
Somatic and depressive symptoms were measured using the Symptom Check List-90 (SCL-90). This is a self-report scale with 90 items that uses a 5-point Likert scale response set to assess how distressed the individual is by different symptoms over the prior one week(1=not at all, 5=extremely). The items are classified into ten primary symptom dimensions including somatization and depression. Continuous scores on the subscales were derived by computing the mean rating for items on each scale. The higher the score is, the more severe the psychological symptoms are. The SCL-90 has demonstrated good reliability and convergent validity in the Chinese population.[21]
2.2.3 Anger trait
Anger trait was assessed using State-Trait Anger Expression Inventory 2 (STAXI-2, Chinese version). It is a self-report scale developed by Spielberger[22]and translated into Chinese by Liu and Gao.[23]STAXI-2 contains 57 items using 4-point Likert scale response.The items are classified into nine dimensions to measure an individual’s anger state, anger trait and anger expression styles. The score derived from the subscale of Anger Trait/T was used to demonstrate participants’ anger trait. Participants with higher score on this subscale tend to experience more angry feelings generally. Except for the dimensions of anger-in and anger-out, good test-retest reliability and convergent and external validity have been established for the other subscales of the STAXI-2 (Chinese version).[23]
2.2.4 Family cohesion and adaptability
Family adaptability and cohesion scale, second edition(FACES II, Chinese Version) was used to measure the family cohesion and adaptability of the participants.[24]The FACES-II is a self-report scale composed of 30 items. Participants rated how well each of the items described their original families on a 5-point Likert-type scale ranging from never (1) to always(5). Continuous scores on the two factor-analytically derived subscales indexing Family cohesion and Family adaptability were used. Family cohesion refers to the extent to which family members stay emotionally close to each other. Family adaptability concerns the families’ability to adapt to different challenges and situations resourcefully. The higher scores are positively related to higher family closeness trait and higher family reflexivity referring to problem solving. The FASCESII (Chinese Version) has demonstrated adequate testretest reliability and internal consistency.[24]
2.3 Statistical analysis
SPSS 19.0 was used to conduct the statistical analysis.Because previous research has demonstrated a gender difference in the link from anger trait to experiencing somatization,[4]correlational and regression analysis were conducted separately for male and female participants.One-way ANOVA or Man-Whitney test were used to compare the scores of somatization, depression, ager trait, family cohesion and family adaptability between genders. Links between anger trait, depression, family cohesion and family adaptability and somatization were assessed with Spearman correlation coefficients. Based on the theory of Baron and Kenney, the significance of potential moderators, family cohesion and family adaptability, were identified using hierarchical linear regression analysis (Enter).[25]If the independent variable is denoted as X (anger trait), the moderator as Z (family cohesion or family adaptability), and the dependent variable as Y (somatization), Y is regressed on X, Z and X*Z. Moderator effects are indicated by the significant effect of X*Z while X and Z are controlled. All statistical tests were two-tailed and the level of statistical significance was set at p<0.05.
3. Results
3.1 Comparison of the variables between genders
As shown in table 1, no significant differences on somatization, depression and anxiety between genders were revealed. Female subjects reported higher scores on anger trait, family cohesion and family adaptability than that of male subjects.

Table 1. Comparison on the scores of Somatization, Depression, Anger trait, Family cohesion and Family adaptability
3.2 Correlations among variables in the moderation model
Pearson correlations revealed that somatic symptom scores were significantly correlated in the expected directions with depression and anger trait for both male and female students (see Table 2). For both genders, somatization was negatively associated with family cohesion and family adaptability.
3.3 Testing the moderation effects of family cohesion and family adaptability
Moderation analyses were carried out according to the guidelines established by Baron and Kenny and elaborated by Kraemer and colleagues.[25,26]Table 3 and Table 4 present the results of hierarchical regressions testing whether family cohesion and family adaptability moderate the link between anger trait and somatization. Age, socioeconomic status and being in a one-child family/not were introduced in step 1 as covariates and accounted for 2% of the variance in somatization for men and women. In step 2, anger trait was included as independent variable (X) and accounted for 13% of variance in somatic symptoms for both genders.As Table 3 shows, family cohesion (moderator, Z) and anger trait * family cohesion (X*Z) were entered in step 3. Results demonstrated that, for both male and female students,the standardized regression coefficient (β) of X*Z stayed significant while X and Z are controlled. It indicated that family cohesion moderated the link between anger trait and somatization. In step 4, depression and anxiety were added to see if basic associations remained unchanged even after accounting for depressive and anxious symptomatology. For men, addition of current depressive and anxious symptoms explained a significant 42% of additional variance. The standardized regression coefficients for anger trait was reduced somewhat but remained significant and the β for X*Z remained marginally significant. This implied that,for males, the moderating role of family cohesion was to some degree marginally significant with consideration of current depression and anxiety. For females, depressive and anxious symptoms explained another 33% of the variance in somatization. The standardized regression coefficients for anger trait and X*Z were reduced somewhat but remained significant. This suggested that, for females, current depression, anxiety and anger trait were independently linked with somatization, and the moderating role of family cohesion was significant even when depression and anxiety were accounted for. The negative β of X*Z implied that the higher the family cohesion scores were, the weaker the link between anger trait and somatic symptoms was. The final regression models explained 52% of the variance in women’s somatization scores and 60% of the variance in men’s somatic scores.
The interaction effect was further explored using simple slope analyses[27]and conditioned at 1 standard deviation above and below the mean on Family cohesion(see Fig. 1). When conditioned at one standard deviation below the mean on Family cohesion, high anger trait was significantly related to more somatic complaints,β= 0.16, t (110) = 2.09, p = 0.04. When conditioned at one standard deviation above the mean on Family cohesion, high anger trait had a non-significant relation to somatization, β= -0.12, t (140) = -1.94, p = 0.06.
Table 4 shows results of similar models in which family adaptability was tested as a moderator of the link between anger trait and somatization. In step 3, the standardized regression coefficient (β) of anger trait *family adaptability (X*Z) was significant while anger trait (X) and family adaptability (Z) were controlled. It indicated that family adaptability moderated the link between anger trait and somatization for both genders.However, after depression and anxiety were controlled in step 4, although the standardized regression coefficients for anger trait remained significant for men and marginally significant for women, the βs of anger trait * family adaptability were no longer significant for either gender. For men, addition of current depressive and anxious symptoms explained a significant 42% of additional variance. For women, depressive and anxious symptoms explained another 35% of the variance in somatization. The final regression models explained 52% of the variance in women’s somatization scores and 59% of the variance in men’s somatic scores.
4. Discussion
4.1 Main findings
The initial analyses of the present study replicated the independent associations found in previous studiesbetween anger trait and somatization, depression and somatization, and family functions and somatic complaints.[4,5,10,13,20,28]With respect to the linear regression analysis, when current depression and anger were considered in the same model, we found that for both males and females, anger trait was significantly linked with somatization. This finding supports the conclusions of prior studies that anger trait was an independent predictor of somatic complaints, even after accounting for co-variables such as gender, family income and depressive symptoms.[4-7]

Table 2. Spearman correlations between somatization and depression, anger trait, family cohesion and family adaptability

Table 3. Hierarchical regression analysis for moderation model of family cohesion
The main findings of this study were that, in a college student-based sample, degree of family cohesion moderated the link between anger trait and somatization for women, whereas for men this link was only marginally moderated by family cohesion. How might we understand these moderation effects, and the difference between genders? For females, the negative β of anger trait * family cohesion (X*Z) implied that the higher the family cohesion scores were the weakerthe link from anger trait to somatic symptoms. This implied that even for women who were more prone to anger, if they were embedded in the families with more cooperation and interpersonal emotional support,somatization would not be presented as a sequence of anger feelings. This might be to some degree related with Chinese tradition. In China, the character of female is more likely to be considered as dependent and tender.[29]It is more acceptable that female adults continue to have emotional involvements with their original families than men do. When enmeshed into overt anger, it might be more natural and appropriate for women to seek emotional support and empathy from previous caregivers and families. Hence, the family circumstance with higher cohesion could provide them with more resources and help to protect women from the attack of angry experiences. This is somewhat consistent with the results of previous research on the outcome of resource-oriented family therapy approaches, which found that somatic patients would benefit from psychotherapy models exploring and cultivating the family’s resources, such as fosteringmore interpersonal empathy between members.[30,31]

Table 4. Hierarchical regression analysis for moderation model of family adaptability
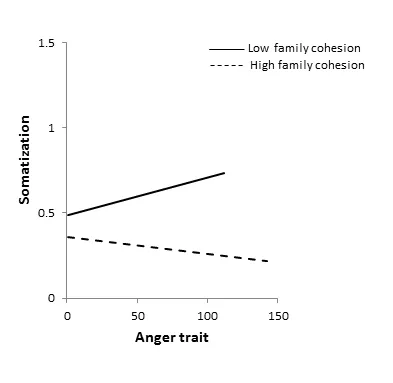
Figure 2. Simple slope analyses of moderation effect of family cohesion on the associations between anger trait and somatization in female subjects
For males, analysis only revealed a marginal moderation effect of family cohesion in the link between anger trait and somatization. This gender difference could be related with traditional gender identification for males. Men are more characterized as independent and expected to have better ability to manage emotions on their own.[29]Thus, men with higher anger proneness may shift efforts to get support outside the family, such as from friends. This might have reduced the protective power of family cohesion in the link from men’s angry experience to their somatization. However, the moderation effect still remained marginally significant for men.It might partially be explained by the special psychodevelopment life stage of our sample. 98.3% of the participants of present study were freshmen or sophomores. Most of them were at the family life stage of launching of young adult and still struggling to differentiate from their parents and original families.[32]Hence, when confronted with anger or other negative feelings, men might also stay closer with their families and get emotional support or empathy to some degree.This might have partially raised the moderation effect of family cohesion for men.
Comparatively, although family adaptability was found to moderate the link between anger trait and somatization for both genders, significant moderation effects were revealed for neither gender after accounting for current depression. One possible explanation for the difference might be that somatization is more tightly linked with the experience or management of negative emotions including anger and depression, but not so strongly with strategies individuals and families take to deal with stress and daily challenges.[33-35]Additionally, depressive symptoms may bias participants toward more negative responses to stressful emotions and bodily feelings.[20]When the present depressive emotions are absent, the subjects’cognition is less biased by depressive emotions. Then more flexible coping strategies in the family could help high anger-trait individuals find better methods to manage anger and exempt them from experiencing angry feelings, and in turn develop less somatic complaints. Comparatively, comorbidity of depression might have exaggerated individuals subjective feelings about the biological response fostered by anger, and strengthened the correlation between anger trait and somatization. Then, the protecting effect of family adaptability and flexibility may be reduced because angry subjects with depression are over focused on the sequence brought by anger. This is somehow consistent with the results of prior research on the outcome of antidepressant use, that the body symptoms of depression were usually relieved after the scores on depressive emotions decreased.[36]
4.2 Limitations
This study has several limitations. First, the crosssectional design establishes associations but cannot determine causality. Although the path from anger trait to somatic complaints and the moderation effect of family cohesion makes sense temporally, other explanations or paths are also possible. For example,low family cohesion may lead to higher proneness, and in turn, foster more somatization. Prospective studies are needed to shed light on causal relationships among anger, family function and somatization.
Secondly, in the present study we selected college students who might be higher functioning,better educated and generally healthier than a more mixed population that included individuals who have mental health disorders or interpersonal difficulties.They might have a higher level of mentalization than those in the general population do. Thus, we must be circumspect about the generalizability of our findings to the general population. It is important for future studies to explore the same moderation model in a more mixed and general sample.
Third, we have not controlled some other potential co-variables which might shed influence on the development and maintenance of somatization in current study. For example, previous research revealed insecure attachment, history of childhood abuse personality style and anger suppression were also associated with somatization and negative emotions.Future research incorporating measures of more potential co-variables are suggested.
Fourth, in the current study only self-reports of somatic symptoms were used. There were no independent measures of physical health. Despite our efforts to control for variables associated with medical illness, the SCL-90 scores may reflect some degree of actual medical morbidity as well as somatization. A crucial direction for future research on the role of family functions in the path from anger trait to somatization is to incorporate indices of objective health.
Fifth, in our study all the psychosomatic symptoms and anger traits were assessed by selfreport scales. The scores of self-report scales might be subjective and it would be more objective to add some other-evaluation scales in future research.
4.2 Implications
Research exploring the factors which moderate the link between anger and somatization may help inform the psychiatric and psychological treatment of angry individuals who report medically unexplained physical symptoms. Moreover, the results of current study provide more empirical and direct evidence to help understand the mechanism by which family therapy works for somatization.
Because anger trait is a relatively stable personal characteristic that tends to persist and may be difficult to change, it might be more productive for therapists to look for potentially modifiable factors such as fostering more family cohesion for clients from a more systemic way.[3,4]Consistent with the proposition of Walsh and Satir, our findings suggest that angry women with somatic complaints might benefit from family therapy approaches that teach their family how to foster more interpersonal empathy and adaptive emotional bonds rather than just focusing on teaching individuals how to manage anger and avoid anger-eliciting situations.[30,37]
For college men who are more prone to anger,the results of the current study implied that a comprehensive model that combines family cohesion fostering with individual anger management might be more effective to reduce their vulnerability to medically unexplained somatic symptoms.
Funding
The study was funded by the National Natural Science Foundation of China (Funding NO: 81301154).
Conflict of interest statement
The authors declare no conflict of interest.
Informed consent
Written informed consent was signed by each participant at the beginning of the study and all private information was kept confidential.
Ethical approval
All procedures were approved by the institutional review board of Tongji University School of Medicine.
Authors’ contribution
Liang Liu was the principle investigator and contributed to the program design, subject screening, data inputting and analysis, article writing and editing.
Cuilian Liu distributed the measurements and input the data.
Xudong Zhao has contributed to the screening of subjects and editing of articles.
1. Fink P, Sorensen L, Engberg M, Holm M, Munk-Jorgensen P. Somatization in primary care-Prevalence, health care utilization, and general practitioner recognition.Psychosomatics. 1999; 40(4): 330-338. doi: https://doi.org/10.1016/s0033-3182(99)71228-4
2. Khoo EM, Mathers NJ, McCarthy SA, Low WY. Somatisation disorder and its associated factors in multiethnic primary care clinic attenders. Int J Behav Med. 2012; 19(2): 165-173.doi:https://doi.org/10.1007/s12529-011-9164-7
3. Spielberger CD, Johnso EH, Russell SF, Crane RJ, Jacobs GA, Worden TJ. The experienceand expression of anger:Construction and validation of an anger expression scale.In: Cheney,MA, Rosenman RH, editors. Anger and Hostility in Cardiovascular and Behavioral Disorders. New York: McGraw-Hill; 1985. pp. 5-30
4. Liu L, Cohen S, Schulz, MS, Waldinger RJ. Sources of somatization: Exploring the roles of insecurity in relationships and styles of anger experience and expression.Soc Sci Med. 2011; 73(9): 1436-1443. doi: https://doi.org/10.1016/j.socscimed.2011.07.034
5. Denollet J, Sys SU, Brutsaert DL. Personality and mortality after myocardial-infarction. Psychosom Med. 1995; 57(6):582-591. doi: https://doi.org/10.1093/eurheartj/ehi252
6. Denollet J, Gidron Y, Vrints CJ, Conraads VM. Anger,suppressed anger, and risk of adverse events in patients with coronary artery disease. Am J Cardiol.2010; 105(11): 1555-1560. doi: https://doi.org/10.1016/j.amjcard.2010.01.015
7. Perbandt K, Hodapp V, Wendt T, Jordan J. [The distressed personality (Type D) - Correlations with anger, aggression and hostility]. Psychother Psychosom Med Psychol. 2006; 56(8):310-317. German
8. Jellesma FC. Health in young people: Social inhibition and negative affect and their relationship with self-reported somatic complaints. J Dev Behav Pediatr. 2008; 29(2): 94-100.doi: https://doi.org/10.1097/dbp.0b013e31815f24e1
9. Terre L, Ghiselli W. A developmental perspective on family risk factors in somatization. J Psychosom Res. 1997; 42(2):197-208. doi: https://doi.org/10.1016/s0022-3999(96)00237-1
10. Minuchin S, Rosman BL, Baker L. Psychosomatic Families.Anorexia Nervosa in Context. Boston: Harvard University Press; 1978. pp: 104-105
11. Obimakinde AM, Ladipo MM, Irabor AE. Familial and socio-economic correlates of somatisation disorder. Afr J Prim Health Care Fam Med. 2015; 7(1): 8. doi: https://doi.org/10.4102/phcfm.v7i1.746
12. Brown RJ, Schrag A, Trimble MR. Dissociation, childhood interpersonal trauma, and family functioning in patients with somatization disorder. A J P. 2005; 162(5): 899-905.Doi: https://doi.org/10.1176/appi.ajp.162.5.899
13. Scharff L, Langan N, Rotter N, Scott-Sutherland J, Schenck C, Tayor N, et al. Psychological, behavioral, and family characteristics of pediatric patients with chronic pain -A 1-year retrospective study and cluster analysis. Clin J Pain. 2005; 21(5): 432-438. doi: https://doi.org/10.1097/01.ajp.0000130160.40974.f5
14. Retzlaff R, von Sydow K, Beher S, Haun MW, Schweitzer J. The efficacy of systemic therapy for internalizing and other disorders of childhood and adolescence: A systematic review of 38 randomized trials. Family Process. 2013;52(4):619-652. doi: https://doi.org/10.1111/famp.12041
15. Fan MJ. Effects of the “one-child” policy and the number of children in families on the mental health of children in China. Revista De Cercetare Si Interventie Sociala. 2016; 52:105-129
16. Cameron L, Erkal N, Gangadharan L, Meng X. Little emperors: Behavioral impacts of China’s one-child policy. Science. 2013; 339(6122): 953-957. doi: https://doi.org/10.3886/icpsr34521
17. Versella MV, Piccirillo ML, Potter CM, Olino TM, Heimberg RG. Anger profiles in social anxiety disorder. J Anxiety Disord.2016 ; 37: 21-29
18. Asberg K. Hostility/anger as a mediator between college students’ emotion regulation abilities and symptoms of depression, social anxiety, and generalized anxiety. J Psychol.2013; 147(5): 469-490
19. Zimmer-Gembeck MJ, Nesdale D, Webb HJ, Khatibi M,Downey G. A longitudinal rejection sensitivity model of depression and aggression: Unique roles of anxiety, anger,blame, withdrawal and retribution. J Abnorm Child Psychol.2016; 44(7): 1291-1307. doi: https://doi.org/10.1007/s10802-016-0127-y
20. Waldinger RJ, Schulz MS, Barsky AJ, Ahern DK. Mapping the road from childhood trauma to adult somatization: The role of attachment. Psychosom Med. 2006; 68(1): 129-135. doi:http://doi.org/10.1097/01.psy.0000195834.37094.a4
21. Huang Y, Li L. [SCL-90 as Measurement of Mental Health in College Students: a meta-analysis]. Zhongguo Xin Li Wei Sheng Za Zhi. 2009; 23(5): 366-371. Chinese. doi: http://dx.chinadoi.cn/10.3969/j.issn.1000-6729.2009.05.015
22. Spielberger C. Professional Manual for the State-Trait Anger Expression Inventory-2 ( STAXI-2 ). Odessa, FL: Psychological Assessment Resources; 1999
23. Liu H, Gao H. [Reliability and validity of the Chinese version of State-Trait Anger Expression Inventory-2 in college students]. Zhongguo Xin Li Wei Sheng Za Zhi. 2012;26(1): 70-76. Chinese. doi: http://dx.chinadoi.cn/10.3969/j.issn.1000-6729.2012.01.016
24. Phillips MR, Shen Q, Zheng Y. Zhao J, Jiang S, Wang L, et al. [Prelimilary evaluation of Chinese version of FACES II and FES: comparison of normal families and failies of schizophrenic patients]. Zhongguo Xin Li Wei Sheng Za Zhi.1991; 5(5): 198-202. Chinese
25. Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual,strategic, and statistical considerations. J Pers Soc Psychol.1986; 51(6): 1173-1182. doi: https://doi.org/10.1037//0022-3514.51.6.1173
26. Kraemer HC, Stice E, Kazdin A, Offord D, Kupfer D. How do risk factors work together? Mediators, moderators,and independent, overlapping, and proxy risk factors.Am J Psychiatry. 2001; 158(6): 848-856. doi: https://doi.org/10.1176/appi.ajp.158.987.848
27. Aiken LS, West SG. Multiple Regression: Testing and Interpreting Interactions. London: Sage; 1991
28. Yeh ZT, Huang YH, Liu SI. Maternal depression and adolescent emotions: The role of family functioning. J Child Fam Stud. 2016; 25(7): 2189-2200. doi: https://doi.org/10.1007/s10826-016-0399-4
29. Jiang X, Wang P, Wang M. [Relationship between college students’ gender, gender-role identity and occupation-sex stereotype]. Zhongguo Lin Chuang Xin Li Xue Za Zhi. 2010;18(3): 366-368. Chinese
30. McDaniel SH, Hepworth J, Doherty WJ. Medical family therapy with somaticizing patients: the co-creation of therapeutic stories. Family Process. 1995; 34(3): 349-361.doi: https://doi.org/10.1037/10172-021
31. Zhao X, Xuan X. [‘Resource-oriented’ family therapy techniques]. Zhongguo Lin Chuang Xin Li Xue Za Zhi. 1999; 2:119-121. Chinese.
32. Simoes TA, Alberto IM. “But ... we are Africans!”: Family life cycle structuring and functioning in southern Angola. J Psychol Afr. 2015; 25(6): 504-511
33. Abbass A. Somatization: Diagnosing it sooner through emotion-focused interviewing. J Fam Pract. 2005; 54(3): 231
34. Haas J, Eichhammer P, Traue HC, Hoffmann H, Behr M,Cronlein T, Pieh C, Busch V. Alexithymic and somatisation scores in patients with temporomandibular pain disorder correlate with deficits in facial emotion recognition. J Oral Rehabil. 2013; 40(2): 81-90. doi: https://doi.org/10.1111/joor.12013
35. Sanchez-Garcia M, Martinez-Sanchez F, Van der Hofstadt CJ. Alexithymia and experimentally induced emotion recognition in people with somatizations. Psicothema. 2011;23(4): 707-712
36. Wade A, Andersen HF. The onset of effect for escitalopram and its relevance for the clinical management of depression.Curr Med Res Opin. 2006; 22(11): 2101-2110. doi: https://doi.org/10.1185/030079906x148319
37. Brubacher L. Integrating emotion-focused therapy with the Satir model. J Marital Fam Ther. 2006; 32(2): 141-153. doi:https://doi.org/10.1111/j.1752-0606.2006.tb01596.x
低年级大学生中与愤怒特质相关联的躯体化:家庭亲密度和适应性的调节作用
刘亮,刘翠莲,赵旭东
家庭亲密度、家庭适应性、家庭冲突、愤怒倾向,愤怒特质,调节,躯体化
Background:Between 22% and 58% of patients in primary care settings complain of somatic symptoms.Previous research has found that somatization was associated with anger traits and family functions.However, studies that specifically assess the moderating effect of family function in how anger traits become somatic complaints are lacking.
Aim: This study was designed to examine whether the variances in family cohesion and family adaptability moderated the strength of the relationship between anger traits and somatization.
Methods:A cross-section design was conducted and 2008 college students were recruited from a comprehensive university in Shanghai. All participants finished questionnaires including Symptom Check List-90 (SCL-90), State-Trait Anger Expression Inventory 2 (STAXI-2, Chinese version) and Family Adaptability and Cohesion Scale, second edition (FACES II, Chinese Version) to assess their degree of current somatization, anger trait and family function. Hierarchical linear regression analysis (Enter) was conducted respectively for men and women to examine the moderation effect of family cohesion and family adaptability in the association between anger and somatization.
Results:Somatic symptoms were significantly linked in the expected directions with depression and anger trait for both genders. Family cohesion and family adaptability were negatively associated with somatic symptoms. For female college students family cohesion was found to moderate the link between anger trait and somatization, but for male college students the moderation effect of family cohesion was marginally significant. The moderating role of family adaptability was significant for neither male nor female after current depressive symptoms were accounted for.
Conclusion:Proneness to anger is an independent predictor of somatization. For women, a high level of family cohesion was a protective factor which could reduce the influence of anger trait on somatic symptoms. Without comorbidity of current depression, family adaptability to some degree exempted individuals with anger proneness from developing somatic complaints. Interventions that integrate family cohesion cultivation, family flexibility fostering and depression treatment might be more effective for somatic patients high in anger trait.
[Shanghai Arch Psychiatry. 2017; 29(1): 30-40.
http://dx.doi.org/10.11919/j.issn.1002-0829.216102]
1Pudong New District Mental Health Center, Shanghai, China
2Department of clinical psychology, Shanghai East Hospital, Tongji University School of Medical, Shanghai, China
3Tonjgi University, Shanghai, China
*correspondence: Dr. Liang Liu. Mailing address: 165 Sanlin RD, Shanghai Pudong New District Mental Health Center, Shanghai, China. Postcode: 200122.E-mail: Goldwalker@163.com
背景:22%至58%的患者在初级保健机构主诉躯体症状。既往研究发现躯体化与愤怒特质和家庭功能相关。然而,有关研究却非常缺乏,特别是评估家庭功能在愤怒特质如何成为躯体主诉中的调节作用。
目的:本研究的目的是验证家庭亲密度和适应性的变化是否调节愤怒特质和躯体化之间的关系强度。
方法:采用横断面研究设计并从上海一所综合性大学招募2008名大学生。所有参加者完成问卷,包括采用症状自评量表(SCL-90)、状态-特质愤怒表达量表2(STAXI-2中文版)、家庭亲密度和适应性量表第二版(FACES II中文版)来评估其当前的躯体化程度、愤怒特质与家庭功能。采用分层线性回归分析(进入)分别对男性和女性验证家庭亲密度和适应性对愤怒和躯体化之间的关联性的调节作用。
结果:躯体症状在男性女性中均与抑郁和愤怒特质以预期的方向显著相关。家庭亲密度和家庭适应性与躯体症状呈负相关。女大学生家庭亲密度对愤怒特质和躯体化之间的联系起到调节作用,而男大学生家庭亲密度的调节作用是轻微的。变量目前抑郁症状矫正后,家庭适应能力的调节作用在男性和女性中均没有显著性。
结论:容易愤怒是躯体化的一个独立预测因素。对于女性来说,较高的家庭凝聚力是一种保护因素,可以减少愤怒特质对躯体症状的影响。没有当前抑郁的共病的话,家庭适应性在一定程度上可以避免有愤怒倾向的个体发展为躯体化。家庭凝聚力培养、家庭灵活性培养和抑郁治疗相结合的干预措施可能对有愤怒特质的躯体化患者更有效。
Dr. Liang Liu obtained his MD degree from Tongji University Medical School in 2011. He has been working at the Pudong New District Mental Health Center since 2016 where he is an attending psychiatrist. His main research interest is family therapy.
- 上海精神医学的其它文章
- Win ratio –An intuitive and easy-to-interpret composite outcome in medical studies
- The Development of the Mind: A Three Month Old Infant
- The use of psychotropic drugs during pregnancy
- Personality characteristics and neurocognitive functions in parents of children with Autism Spectrum Disorder
- Relationship of mean platelet volume to MDD: a retrospective study
- The psychometric properties of the Quick Inventory of Depressive Symptomatology-Self-Report (QIDS-SR) in patients with HBV-related liver disease

