经胸微创封堵与体外循环治疗不同直径干下型VSD疗效分析
伍成德,刘鹏,林巍,林刚,符芳永
(中南大学湘雅医学院附属海口医院心胸外一科,海南海口570208)
经胸微创封堵与体外循环治疗不同直径干下型VSD疗效分析
伍成德,刘鹏,林巍,林刚,符芳永
(中南大学湘雅医学院附属海口医院心胸外一科,海南海口570208)
目的探讨干下型室间隔缺损(VSD)直径大小对手术疗效的影响,对比分析经胸微创封堵与体外循环治疗不同直径干下型室间隔缺损的治疗效果。方法对2008年8月至2016年8月中南大学湘雅医学院附属海口医院心胸外一科收治的63例缺损直径在3~10 mm的先天性干下型VSD 2~6岁患儿病例资料进行回顾性分析,其中男性35例,女性28例。依据手术方式的不同将其分为体外组和微创组,再依据直径大小差异各分为两组,经胸微创封堵治疗34例,男女比例为19/15,其中直径3~5 mm 13例,>5 mm 21例;正中切口体外循环治疗29例,男女比例为16/13,其中直径在3~5 mm 11例,>5 mm 18例。分别对其手术成功率、术中术后情况及术后并发症进行比较,进行统计分析。结果体外组手术时间、输血总量、机械通气时间、术后重症监护时间、术后住院时间均较微创组长,两种手术方式总体成功率差异有统计学意义(P<0.05)。缺损直径在3~5 mm时,两种手术方式治疗干下型室间隔缺损的手术成功率均为100.00%,差异无统计学意义(P>0.05);缺损直径在5~10 mm时,体外组手术成功率为100.00%,明显高于微创组的80.95%,差异有统计学意义(P=0.045)。手术失败患者的缺损直径均在8~10 mm。两种手术治疗方式的手术时间、输血总量、机械通气时间、术后重症监护时间、术后住院时间及手术成功率均不受缺损直径大小的影响(P>0.05)。两种手术治疗干下型室间隔缺损的术后早期并发症比较差异均无统计学意义(P>0.05),但两种手术方式治疗干下型室间隔缺损的总早期并发症发生率差异有统计学意义(P=0.041),体外组的总体发生率为5.75%,高于微创组的1.67%。两种手术治疗方式的早期并发症发生率不受缺损直径大小的影响(P>0.05)。结论VSD缺损直径大小对不同手术治疗方式的成功率有影响。体外组早期并发症发生率较微创组高,早期并发症发生率不受缺损直径大小影响;微创组较体外组术中优势明显。缺损直径较小选择微创封堵优势明显,缺损直径越大选择体外循环手术治疗优势越明显。
室间隔缺损;干下型;微创封堵术
室间隔缺损(ventricular septal defect,VSD)是常见的先天性心血管畸形之一,其发病率约占先天性心血管疾病的20%~25%[1]。干下型室间隔缺损是室间隔缺损的常见类型,主要位于室间隔漏斗部,紧邻主、肺动脉瓣,位置特殊,该类缺损在亚洲人群中的发病率较高,约占室间隔缺损的15%[2-4]。VSD的传统治疗方法为体外循环(cardiopulmonary bypass,CPB)直视修补术,随着心血管微创技术的快速发展,经胸微创封堵术和介入封堵术因创伤小、恢复快、效果好等优点,在VSD的治疗活动中得到广泛应用。介入封堵治疗术禁忌证较多,不适合用于干下型VSD的治疗。邻近主动脉瓣下的VSD导管介入封堵术操作复杂,并发症较多[5],成功率低,是经皮导管封堵术的相对禁忌证[6]。故该法不适用于干下型VSD的治疗,本文不予以讨论。本研究对经胸微创封堵术和CPB直视修补术2种治疗干下型VSD方法进行比较,探讨两种手术方法在不同缺损直径干下型VSD治疗中的疗效差异,为临床制定最佳治疗方案提供理论依据。
1 资料与方法
1.1 一般资料2008年8月至2016年8月中南大学湘雅医学院附属海口医院心胸外一科经超声心动图确诊63例2~6岁先天性单纯干下型室间隔缺损的患儿,其中男性35例,女性28例,年龄2~6岁,体质量7~16 kg。经胸微创封堵治疗34例,男女比例为19/15;正中切口体外循环治疗29例,男女比例为16/13。术前同每位患者家属沟通并签署知情同意书,该研究经医院伦理委员会审批通过[2016(科研伦审-017)]。
1.2 纳入标准患儿无其他重要脏器先天性畸形或功能不全、染色体病、先天性和继发性免疫抑制或缺陷等;术前经胸超声心动图提示无肺动脉高压者及中重度主动脉瓣脱垂或关闭不全;患儿均为窦性心律;VSD直径≤10 mm且≥3 mm;病历资料完整;术中使用封堵器为先健科技(深圳)有限公司生产,型号及规格为XJFVM04-16(批准文号:国械注准20163770339)。
1.3 方法根据研究目的收集患儿相关资料:(1)基本信息(年龄、性别、体质量);(2)辅助检查结果(超声心动图、心电图、术中经食道超声);(3)手术记录(术式、体外循环时间、手术时间、输血量);(4)住院病历信息(ICU气管插管时间、ICU监护天数、住院天数及手术早期并发症情况)。将收集到的资料依据手术方式不同分为体外循环组和微创组;参照国际室间隔分类标准[7-8],再将每组病例资料按其缺损直径大小分为>5 mm组和3~5 mm组,对比分析两种治疗方法在不同组中的疗效,微创组术中失败患者则改为体外循环直视手术,体外循环手术失败患者则视为患者死亡。
1.4 统计学方法釆用SPSS17.0软件对所收集数据进行统计分析。计量资料符合正态分布者采用独立样本t检验,结果以均数±标准差(x-±s)表示;计数资料釆用χ2检验或Fisher's确切检验,结果以百分比表示。P<0.05为差异有统计学意义。
2 结果
2.1 术前基本情况体外循环组和微创组两组患儿在年龄、性别、体质量及VSD直径等基线资料比较差异均无统计学意义(P>0.05),见表1~表3。
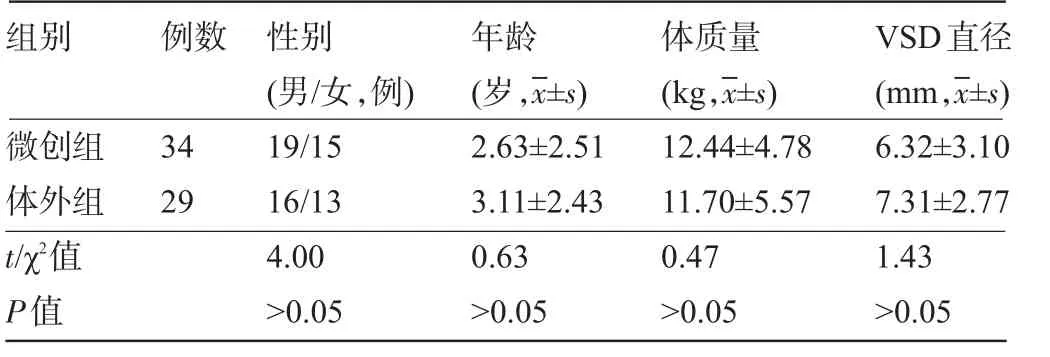
表1 两组术前基本资料比较
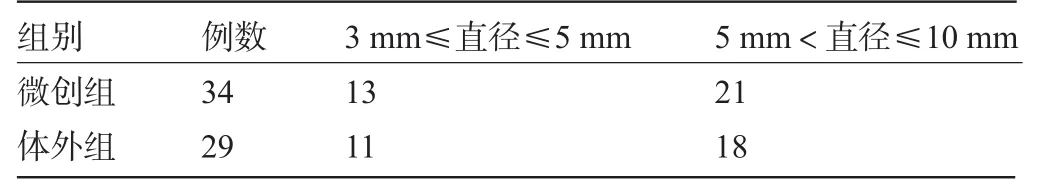
表2 两组数据内部VSD直径缺损程度分布情况(例)

表3 两组数据VSD直径分布情况比较(x-±s)
2.2 两组术中和术后早期结果体外组手术时间、输血总量、机械通气时间、术后重症监护时间、术后住院时间均较微创组长,但不同直径两组间手术成功率差异有统计学意义(P<0.05)。缺损直径为3~5 mm时,两种手术方式治疗干下型室间隔缺损的手术成功率均为100.00%,差异无统计学意义(P>0.05);缺损直径为5~10 mm时,体外组手术成功率为100.00%,明显高于微创组的80.95%,差异有统计学意义(χ2=4.021,P=0.045),手术失败病例均为缺损直径8~10 mm的患者,见表4。不同直径干下型室间隔缺损对两种手术治疗方式组内在手术时间、输血总量、机械通气时间、术后重症监护时间、术后住院时间及手术成功率方面比较差异均无统计学意义(P>0.05),见表5。
2.3 术后早期并发症两种手术治疗干下型室间隔缺损的术后早期单一并发症发生率差异均无统计学意义(P>0.05),但两种手术方式治疗干下型室间隔缺损早期并发症总发生率差异有统计学意义(χ2=4.164,P=0.041),体外组的总体发生率为5.75%,高于微创组的1.67%,见表6。不同缺损直径VSD两种手术方式治疗早期并发症组间比较差异无统计学意义(P>0.05),见表7。不同缺损直径干下型室间隔缺损对两种手术治疗方式早期并发症发生率差异无统计学意义(P>0.05),见表8。
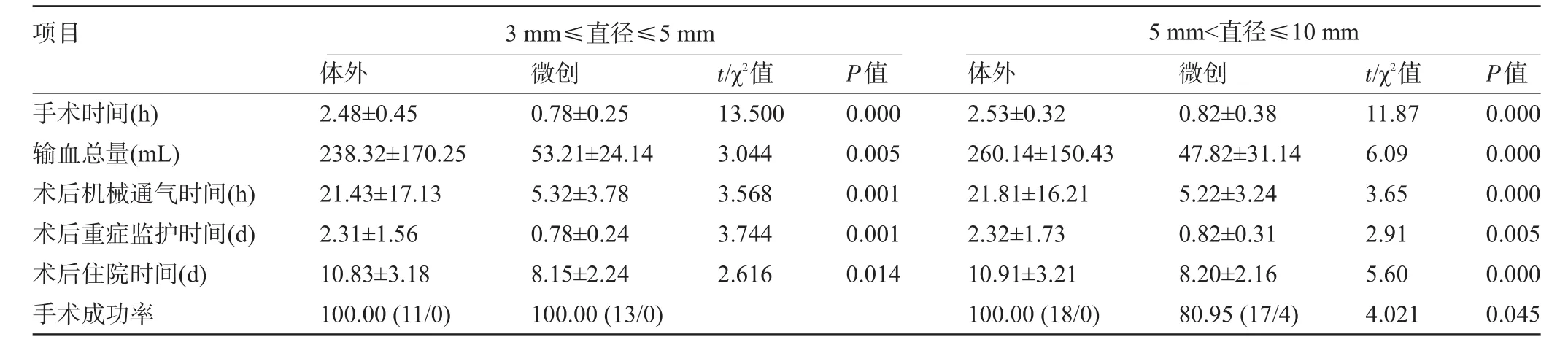
表4 不同缺损直径VSD两种手术治疗术中及术后情况组间比较(x-±s)
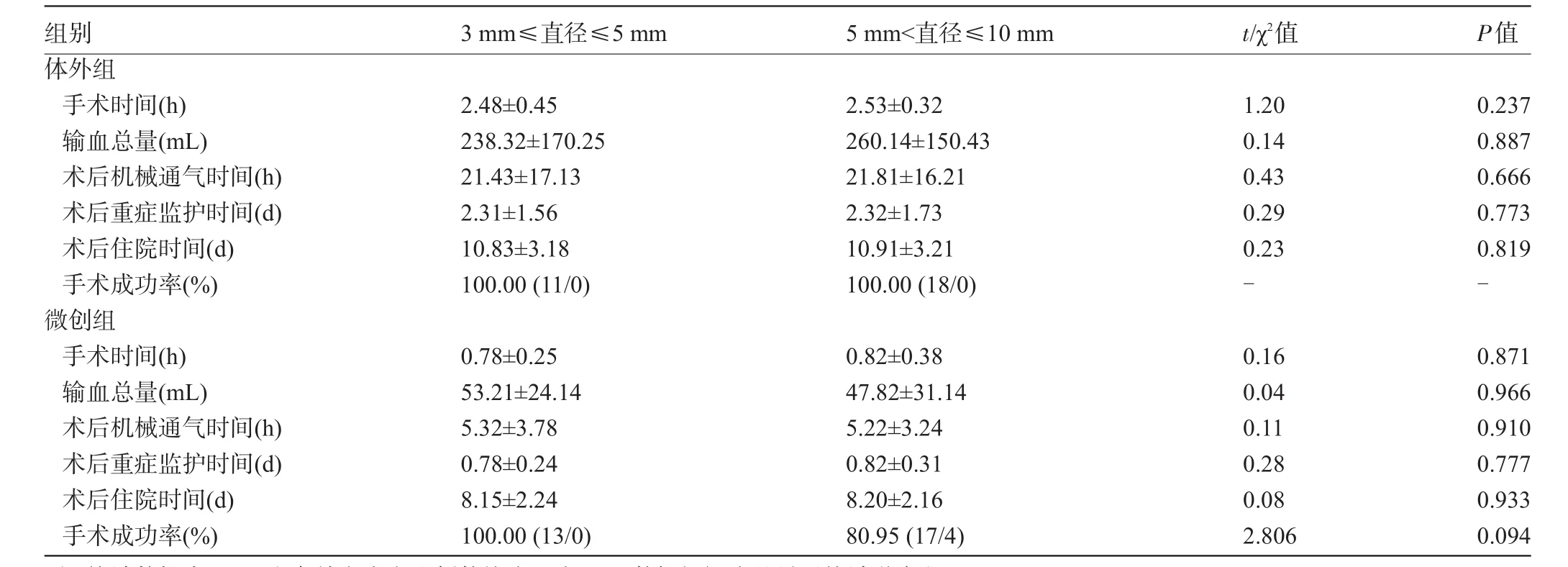
表5 不同缺损直径VSD组内术中及术后情况组内比较

表6 两种手术治疗方法早期并发症总体比较[例(%)]

表7 不同缺损直径VSD两种手术治疗早期并发症组间比较[例(%)]

表8 不同缺损直径VSD早期并发症组内比较[例(%)]
3 讨论
1954年,Lillehei及其团队[9]开展了世界上首例VSD直视修补术,随着手术适应证的严格控制、早期手术和术后监护水平的提高,目前体外直视修补术死亡率低,术后并发症也非常少。体外直视修补术已成为VSD治疗的金标准。1998年经胸微创封堵术治疗VSD开始用于临床[10],相关研究报道疗效确切[11-12]。本研究主要通过分析VSD直径大小对体外和微创两种手术治疗室间隔缺损疗效差异,旨在为临床医师制定手术方案提供参考依据。
本研究将VSD缺损直径大小作为研究的主要指标,观察VSD缺损直径大小对微创及体外循环两种手术治疗室间隔缺损组间及组内疗效差异。通过对两种手术方法的手术成功率进行对比分析,我们发现不同直径两组间手术成功率存在差异,在VSD缺损直径为3~5 mm时,两种手术方式治疗干下型室间隔缺损的手术成功率均为100.00%,差异无统计学意义(P>0.05);但缺损直径为5~10 mm时,体外组手术成功率为100.00%,明显高于微创组的80.95%,差异有统计学意义(χ2=4.021,P=0.045),微创组手术失败者缺损直径均在8~10 mm。目前,室间隔缺损微创封堵伞的直径规格为4~12 mm,在对VSD患者进行封堵伞封堵时要求缺损直径小于封堵伞2~4 mm,根据需要适当选择封堵器的规格[13]。因此,本文仅对缺损直径≤10 mm的患者进行进行研究。有研究表明缺损直径越大,封堵伞所承受的压力越大,稳定性越差,手术成功率越低,这一理论在我们的实验结果中得到了印证[14-18]。
通过术中和术后情况比较,我们发现体外组手术时间、输血总量、机械通气时间、术后重症监护时间、术后住院时间均较微创组长;但两种手术治疗方式组不同缺损直径干下型室间隔缺损的手术时间、输血总量、机械通气时间、术后重症监护时间、术后住院时间及手术成功率差异均无统计学意义(P>0.05)。方舒等[19]研究表明,微创手术具有创伤小、ICU内气管插管时间短、住院时间短、输血比例小的优点。
将两种手术治疗干下型室间隔缺损的术后早期并发症进行比较,我们发现两种手术治疗干下型室间隔缺损的各单一并发症差异均无统计学意义(P>0.05),但两种手术方式治疗干下型室间隔缺损的总早期并发症发生率差异有统计学意义(χ2=4.164,P=0.041),体外组的总体并发症发生率为5.75%,明显高于微创组的1.67%。不同缺损直径干下型室间隔缺损对两种手术治疗方式的早期并发症发生率的影响差异无统计学意义(P>0.05),而张刚成等[20]研究表明微创手术较开胸手术并发症明显减少。
总之,VSD缺损直径大小对体外手术及微创手术治疗的手术成功率存在一定的影响,缺损直径为3~5 mm时,两种手术方式成功率差异无统计学意义,但缺损直径为5~10 mm时,体外循环手术成功率较高。两种手术方式治疗干下型VSD,体外循环组并发症较微创组高,但两种手术方式早期并发症发生率均不受缺损直径大小影响;体外循环手术较微创手术在手术时间、输血总量、机械通气时间、术后重症监护时间及术后住院时间长。直径缺损为3~5 mm的干下型室间隔缺损选择微创手术优势明显,直径缺损在5~10 mm时,选择微创手术需慎重,尤其是对缺损直径在8~10 mm的患者。缺损直径越大选择体外循环手术治疗优势越明显。
[1]周永昌,郭万学,燕山,等.超声医学[M].6版.北京:人民军医出版社,2012:462.
[2]Griffin ML,Sullivan I,Anderson RH,et al.Doubly committed subarterial ventricular septal defect:new morphological criteria with echocardiographic and angiocardiographic correlation[J].British Heart J,1988,59(4):474-479.
[3]Mitchell SC,Korones SB,Berendes HW.Congenital heart disease in 56,109 births.Incidence and natural history[J].Circulation,1971,43(3):323-332.
[4]An G,Zhang H,Zheng S,et al.Minimally invasive surgical closure for doubly committed subarterial ventricular septal defects through a right subaxillary thoracotomy[J].Interact Cardiovasc Thorac Surg,2016,23(6):924-928.
[5]徐玮泽,张泽伟,曹兴许,等.经胸右心室穿刺偏心伞封堵主动脉瓣下室间隔缺损[J].中华胸心血管外科杂志,2011,27(3):178-179.
[6]吴勤,高雷,杨一峰,等.超声心动图引导经胸小切口室间隔缺损封堵术[J].中南大学学报(医学版),2012,37(7):699-705.
[7]Capelli H,Andrade J L,Somerville J.Classification of the site of ventricular septal defect by 2-dimensional echocardiography[J].American Journal of Cardiology,1983,51(9):1474-1480.
[8]Spicer DE,Hao HH,Co-Vu J,et al.Ventricular septal defect[J].Orphanet Journal of Rare Diseases,2014,9(1):144.
[9]Lillehei CW,Cohen M,Warden HE,et al.The result of direct vision closure of ventricular septal defects in eight patients by means of controlled cross circulation[J].Surgery Gynecology&Obstetrics,1955,101(4):446-466.
[10]Zhu D,Tao K,An Q,et al.Perventricular device closure of residual muscular ventricular septal defects after repair of complex congenital heart defects in pediatric patients[J].Texas Heart Institute Journal,2013,40(5):534-540.
[11]Tao K,Lin K,Shi Y,et al.Perventricular device closure of perimembranous ventricular septal defects in 61 young children:early and midterm follow-up results[J].Journal of Thoracic&Cardiovascular Surgery,2010,140(4):864-870.
[12]Xing Q.Minimally invasive transthoracic device closure of ventricular septal defects in younger and low body weight children;clinical experience and mid-term results[C]//2011:105-106.
[13]中国医师协会儿科医师分会先天性心脏病专家委员会.儿童常见先天性心脏病介入治疗专家共识[J].中华儿科杂志,2015,53(1):17-24.
[14]王欣,赵天力,吴勤,等.经胸微创封堵术与体外循环下手术治疗室间隔缺损效果的比较[J].中华心血管病杂志,2012,40(10):830-833.
[15]Khan ZA,Arif RA,Maadullah,et al.Device closure of atrial septal defect with amplatzer septal occluder in adults—safety and outcome[J].Journal of Ayub Medical College Abbottabad Jamc,2013,25(3-4):48-49.
[16]Oses P,Hugues N,Dahdah N,et al.Treatment of isolated ventricular septal defects in children:Amplatzer versus surgical closure[J].Annals of Thoracic Surgery,2010,90(5):1593-1598.
[17]秦永文,赵仙先,吴弘,等.国产室间隔缺损封堵器的安全性和疗效评价[J].中国循环杂志,2005,20(1):10-13.
[18]El-Sisi A,Sobhy R,Jaccoub V,et al.Perimembranous ventricular septal defect device closure:choosing between amplatzer duct occluderⅠandⅡ[J].Pediatric cardiology,2017,38(3):596-602.
[19]方舒.经胸微创封堵术与体外循环下治疗儿童干下型室间隔缺损的比较[D].杭州:浙江大学,2015.
[20]张刚成,沈群山,尚小珂,等.经皮导管介入封堵与外科微创封堵治疗室间隔缺损的对比研究[J].中国介入心脏病学杂志,2013,21(1):17-20.
Curative effect of transthoracic mini-invasive occlusion and cardiopulmonary bypass on subpulmonic ventricular septal defect of different diameters.
WU Cheng-de,LIU Peng,LIN Wei,LIN Gang,FU Fang-yong.Cardiothoracic DepartmentⅠ,Central South University Xiangya School of Medicine Affiliated Haikou Hospital,Haikou 570208,Hainan,CHINA
ObjectiveTo investigate the effect of diameter of subpulmonic ventricular septal defect(VSD)on the curative effect of operation,and to compare the curative effect of transthoracic mini-invasive occlusion and cardiopulmonary bypass on subpulmonic VSD of different diameters.MethodsThe clinical data of 64 children with the diameter of 3-10 mm congenital subpulmonic VSD,including 35 males and 28 females,who admitted to Cardiothoracic Department of Central South University Xiangya School of Medicine Affiliated Haikou Hospital from August 2008 to August 2016,were retrospectively analyzed.The patients were divided intoin vitroand mini-invasive group according to the different surgical methods,and then were divided into two groups according to their differences in diameter.There were 34 cases in the mini-invasive group with male to female ratio of 19/15,with 13 cases of 3-5 mm diameter and 21 cases of more than 5 mm.There were 29 cases of median incision cardiopulmonary bypass(in vitrogroup)with male to female ratio of 16/13,with 11 cases of 3-5 mm diameter,18 cases of more than 5 mm.The operative success rate,intraoperative and postoperative complications were compared and analyzed statistically.ResultsThe operative time,total blood transfusion,mechanical ventilation time,postoperative intensive care time and postoperative hospitalization time of in vitrogroup were significantly longer than those of mini-invasive group(P<0.05).There was a significant difference in the overall success rate between the two surgical methods(P<0.05).There was no significant difference in the success rate between the two groups in the 3-5 mm diameter of the defect(100.00%vs100.00%,P>0.05).When the diameter of the defect was 5-10 mm,the success rate ofin vitrogroup was 100.00%,which was significantly higher than 80.95%of the mini-invasive group(χ2=4.021,P=0.045).All failed patients had a defective diameter of 8 mm to 10 mm.The operative time,total blood transfusion,mechanical ventilation time,postoperative intensive care time,postoperative hospital stay and operation success rate were not affected by the diameter of the defect(P>0.05).There was no significant difference in the early complications of the two types of surgical treatment of subpulmonic VSD(P>0.05).However,there were statistically significant differences in the incidence of early complications between the two surgical methods for thetreatment of subpulmonic VSD(P=0.041).The overall incidence of thein vitrogroup was 5.75%,which was significantly higher than 1.67%of mini-invasive group.The incidence of early complications of both surgical treatments was not affected by diameter(P>0.05).ConclusionThe diameter of VSD has an effect on the success rate of different surgical methods.The incidence of early complications in the cardiopulmonary bypass(in vitro)group was higher than that in the mini-invasive group,and the incidence of early complication was not affected by the diameter of the defect.The minimally invasive group has obvious advantages than the cardiopulmonary bypass group.For the defect with the smaller diameter,the mini-invasive occlusion has obvious advantages.Otherwise,cardiopulmonary bypass has obvious advantages.
Ventricular septal defect(VSD);Subpulmonic;Mini-invasive occlusion
R541.1
A
1003—6350(2017)18—2974—05
2017-04-05)
10.3969/j.issn.1003-6350.2017.18.014
林刚。E-mail:3125007420@qq.com

