单孔与传统三孔法腹腔镜阑尾切除术治疗成人急性阑尾炎的随机对照研究*
刘海龙,曾和平,林谋斌,吴 炜,李 健,李 桢,汤 旻,李 镇,常 毅,徐嘏毅
(同济大学附属杨浦医院,上海,200090)
单孔与传统三孔法腹腔镜阑尾切除术治疗成人急性阑尾炎的随机对照研究*
刘海龙,曾和平,林谋斌,吴 炜,李 健,李 桢,汤 旻,李 镇,常 毅,徐嘏毅
(同济大学附属杨浦医院,上海,200090)
目的:比较单孔腹腔镜阑尾切除术(single-port laparoscopic appendectomy,SPLA)与传统三孔法腹腔镜阑尾切除术(conventional laparoscopic appendectomy,CLA)治疗成人急性阑尾炎的安全性与有效性。方法:将2014年1月至2015年12月收治的160例急性阑尾炎患者按随机数字表法分组,其中SPLA组78例、CLA组82例,观察两组患者的疗效。结果:术后24 h患者疼痛评分[(3.4±2.1)vs.(3.3±1.9)]两组差异无统计学意义(P=0.892)。术后3个月健康调查简表SF-36八个维度指标及总分差异无统计学意义(P>0.05)。术后3个月两组患者切口美观度自评分[(8.2±1.1) vs.(7.4±1.4)]差异有统计学意义(P<0.001)。SPLA组手术时间较CLA组长(P<0.001),中转率高(P=0.013)。两组术后镇痛药使用率(P=0.619)、住院时间(P=0.680)及并发症发生率(P=0.425)差异均无统计学意义。结论:与常规腹腔镜阑尾切除术相比,SPLA治疗成人急性阑尾炎在切口美观度方面具有优势,术后疼痛、生活质量方面两种术式相当,但SPLA手术时间更长,且依赖于术者较高的腹腔镜操作技巧。
急性阑尾炎;阑尾切除术;腹腔镜检查;单孔;成年人
急性阑尾炎是胃肠外科最常见的急腹症。腹腔镜阑尾切除术(laparoscopic appendectomy,LA)已逐渐成为阑尾炎手术治疗的金标准[1-2]。近年,单孔腹腔镜阑尾切除术(single-port laparoscopic appendectomy,SPLA)逐渐开展,与传统三孔法腹腔镜阑尾切除术(conventional laparoscopic appendectomy,CLA)相比,SPLA的最大优势可能是切口更美观[3]。但目前SPLA的临床应用价值尚存有争议[4-6]。本研究进行了一项随机对照临床试验,将疼痛视觉模拟评分法(visual analogue scale,VAS)、患者切口美观度评分、健康调查简表(the MOS 36-item short form health survey,SF-36)等患者报告结局(patient-reported outcome,PRO)指标纳入结局评价,比较SPLA与CLA治疗成人急性阑尾炎的安全性、有效性,为SPLA的合理应用提供临床证据。
1 资料与方法
1.1 临床资料 本组病例为2014年1月至2015年12月同济大学附属杨浦医院普通外科收治的急性阑尾炎患者。急性阑尾炎诊断标准[7]:(1)转移性右下腹疼痛或右下腹疼痛病史;(2)查体右下腹压痛,可伴有反跳痛;(3)体温>38℃,或白细胞>10×109/L。纳入标准:(1)符合上述诊断标准;(2)18~90岁;(3)已签署知情同意书。排除标准:(1)临床未确诊急性阑尾炎;(2)>90岁或<18岁;(3)病程超过5 d;(4)右下腹扪及包块或影像学检查提示右下腹包块;(5)肝硬化、凝血功能障碍、弥漫性腹膜炎、休克、有腹部手术史、腹水、可疑恶性病变、妊娠、全麻禁忌者;(6)术中探查排除急性阑尾炎诊断或同时处理其他腹内疾病。160例患者符合纳入标准,采用随机数字表法分别纳入SPLA(n=78)与CLA组(n=82)。两组患者临床资料见表1。
表1 两组患者资料
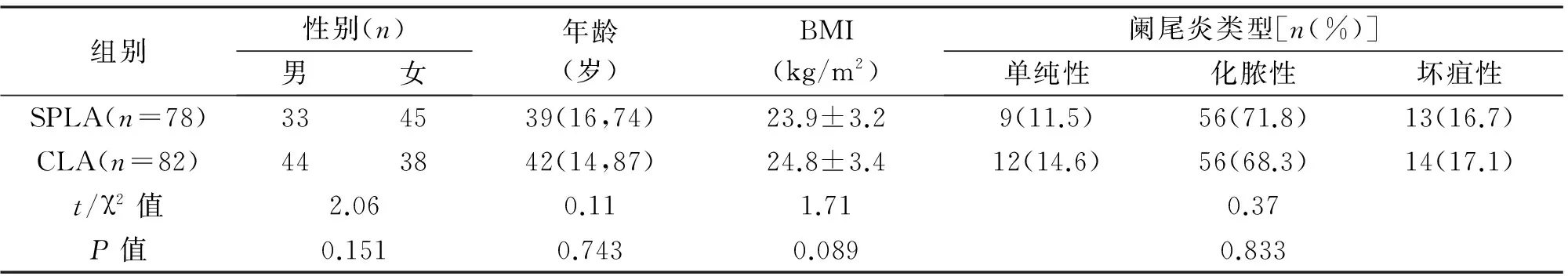
组别性别(n)男女年龄(岁)BMI(kg/m2)阑尾炎类型[n(%)]单纯性化脓性坏疽性SPLA(n=78)334539(16,74)23.9±3.29(11.5)56(71.8)13(16.7)CLA(n=82)443842(14,87)24.8±3.412(14.6)56(68.3)14(17.1)t/χ2值2.060.111.710.37P值0.1510.7430.0890.833
1.2 手术方法 术前处理:(1)术区备皮,清洁脐孔,留置导尿;(2)抗生素使用:术前30 min静滴头孢呋辛1.5 g,头孢过敏者应用氨曲南2.0 g。手术均由4位具有高级职称的普通外科医师完成,4位医师均具有多年的腹腔镜手术经验,能熟练完成两种手术。SPLA组:全麻气管插管,患者取仰卧位,常规消毒铺巾。取脐右下缘切口,穿刺5 mm Trocar,建立人工气腹,压力维持在14 mmHg,置入5 mm腹腔镜。观察孔上缘约3 mm处穿刺5 mm Trocar作为主操作孔,下缘3 mm处穿刺5 mm Trocar,置入无损伤抓钳,见图1、图2。所用器械均为传统腹腔镜手术器械。患者头低足高15°,向左倾斜15~30°。探查腹腔内脏器,并沿结肠带找到阑尾,显露阑尾,置入5 mm超声刀,离断阑尾系膜血管后,完全游离阑尾至根部,提起阑尾,置入圈套器将阑尾根部圈套结扎,用超声刀离断阑尾,将阑尾装入标本套,自脐部穿刺孔取出。见图3、图4。检查术野无活动性出血,退出器械后放气腹,切口聚维酮碘消毒后,用可吸收线缝合脐孔,皮内缝合切口或胶水粘合切口,结束手术。常规三孔法LA组:术前准备、麻醉同前。取脐上缘切口,穿刺5 mm Trocar,建立人工气腹,压力维持在14 mmHg,置入腹腔镜,主操作孔为左侧髂前上棘与脐连线中外1/3交界处10 mm穿刺孔,副操作孔为脐与耻骨联合连线中点5 mm穿刺孔。器械均为传统腹腔镜手术器械。操作同SPLA组。后12 h开始进流质食物,根据患者情况使用镇痛药物。

图1 单孔腹腔镜使用的三枚5 mm Trocar 图2 三枚Trocar的位置
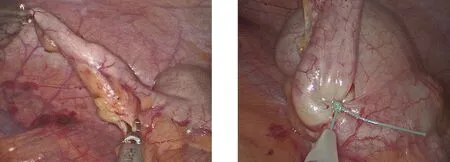
图3 单孔腹腔镜下超声刀处理阑尾系膜图4 单孔腹腔镜下用圈套器结扎阑尾根部
1.3 观察指标
1.3.1 主要观察指标 (1)切口美观度评分(0~10分):术后3个月随访时患者自评,非常不满意0分,非常满意10分[8];(2)SF-36健康调查:术后3个月电话或信件随访完成[9-10];(3)VAS评分:术前评分及术后24 h评分[11]。
1.3.2 次要观察指标 镇痛药物使用、手术时间、手术中转率、并发症发生率(切口感染、腹腔感染、大出血、残端瘘、术后肠梗阻)及住院时间。
2 结 果
2.1 临床结局指标 两组患者术后镇痛药物使用情况、住院时间差异无统计学意义(P=0.619,P=0.680),SPLA组手术时间明显长于LA组(P<0.001)。SPLA组中10例中转为三孔法LA或开腹手术,CLA组中2例中转开腹,SPLA组中转率显著高于CLA组(P=0.013)。手术中转原因主要为阑尾显露困难及阑尾根部穿孔。SPLA组术后发生并发症5例(6.4%),分别为穿刺孔感染2例、腹腔感染2例、术后炎性肠梗阻1例;CLA组术后3例(3.7%)发生并发症,分别为穿刺孔感染2例、穿刺孔出血1例;两组总体并发症发生率差异无统计学意义(P=0.425)。见表2。
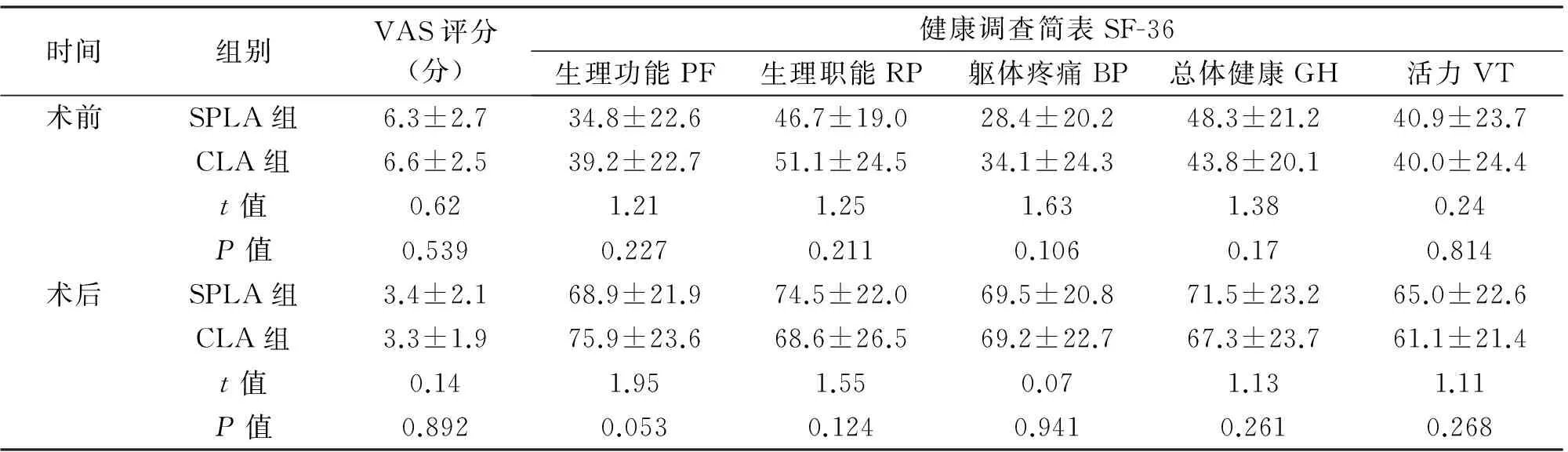
2.2 PRO指标 术后24 h,两组患者疼痛评分差异无统计学意义(P=0.892)。术后3个月健康调查简表SF-36八个维度指标及总分差异均无统计学意义(P>0.05)。术后3个月两组患者切口美观度自评分差异有统计学意义(P<0.001)。两组PRO见表3。
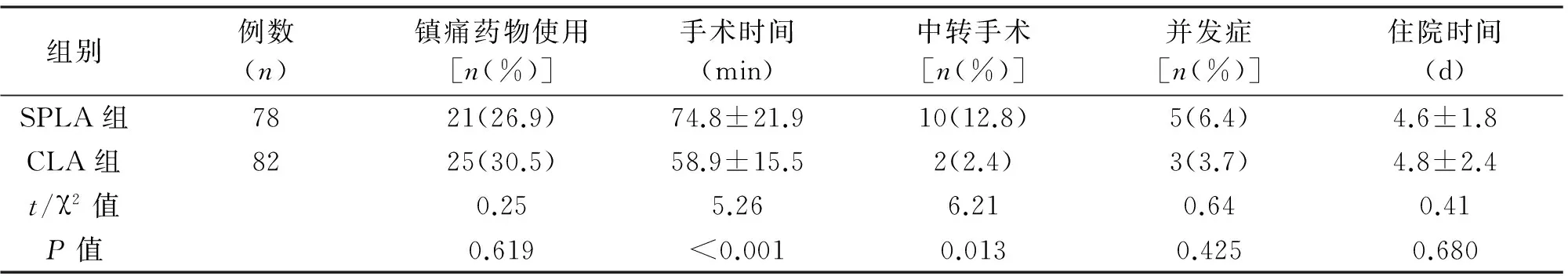
组别例数(n)镇痛药物使用[n(%)]手术时间(min)中转手术[n(%)]并发症[n(%)]住院时间(d)SPLA组7821(26.9)74.8±21.910(12.8)5(6.4)4.6±1.8CLA组8225(30.5)58.9±15.52(2.4)3(3.7)4.8±2.4t/χ2值0.255.266.210.640.41P值0.619<0.0010.0130.4250.680
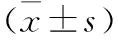
时间组别VAS评分(分)健康调查简表SF-36生理功能PF生理职能RP躯体疼痛BP总体健康GH活力VT术前SPLA组6.3±2.734.8±22.646.7±19.028.4±20.248.3±21.240.9±23.7CLA组6.6±2.539.2±22.751.1±24.534.1±24.343.8±20.140.0±24.4t值0.621.211.251.631.380.24P值0.5390.2270.2110.1060.170.814术后SPLA组3.4±2.168.9±21.974.5±22.069.5±20.871.5±23.265.0±22.6CLA组3.3±1.975.9±23.668.6±26.569.2±22.767.3±23.761.1±21.4t值0.141.951.550.071.131.11P值0.8920.0530.1240.9410.2610.268
续表3
时间组别健康调查简表SF-36社会功能SF情感职能RE精神健康MH总分切口美观度评价术前SPLA组48.5±19.847.5±22.658.7±21.4353.8±79.1-CLA组52.6±24.049.5±24.861.5±23.5371.8±105.3-t值1.180.540.781.22-P值0.2390.5890.4380.225-术后SPLA组77.7±19.874.6±19.780.2±21.2581.8±83.68.2±1.1CLA组73.7±19.476.7±21.575.1±21.8567.6±97.87.4±1.4t值1.310.651.480.994.27P值0.1940.5200.1400.325<0.001
3 讨 论
Semm[12]于1983年首次报道了LA,经过发展已成为急性、慢性阑尾炎手术治疗的金标准,目前临床应用LA较多[13]。SPLA是近年新开展的术式。单孔腹腔镜手术是指由一个1.5~4.0 cm的小切口置入多个穿刺器或一个带有多个操作孔道的穿刺器,通过操作孔道置入手术器械完成手术操作,通常取脐部小切口[2]。初步研究表明,SPLA的有效性、安全性与常规LA相比差异无统计学意义,且SPLA在切口美观度方面优于LA,甚至有学者认为SPLA可能取代LA成为阑尾切除术的首选术式[4,10]。
既往针对SPLA的报道多为回顾性研究[14-18],少数随机对照研究[19-20]也主要以临床客观指标为结局指标,缺少反应患者主观感受的PRO。PRO是指来自于患者对自身健康状况、功能状态及治疗感受的报告[21]。PRO是通过标准化的量表收集而来的,它能提供的信息远远多于临床医生或生理测量所得的信息,从而使临床疗效的判断更全面、真实、可靠。2013年CONSORT声明推荐将PRO作为随机对照研究需要报告的结局指标之一[22]。
本研究采用了三个PRO指标:VAS、患者切口美观度评分、SF-36健康调查简表。其中切口美观度评价两组差异有统计学意义,提示SPLA的切口利用脐部皱褶的掩饰,其切口美观度较LA具有明显优势。这与既往大多数研究结果一致[17-18,23]。在术后疼痛方面,本研究提示SPLA与LA差异无统计学意义,既往也有报道得到相同结果[14-15,18,23-26]。但也有研究表明,SPLA在术后疼痛方面优于LA[17,27],甚至也有研究认为SPLA术后疼痛反而较重[8,28]。这可能是由于不同的研究采用的“单孔”方式不一致造成的。生活质量方面的比较,既往研究较少,本研究提示两组间SF-36生活质量评分差异无统计学意义。
SPLA的缺点主要是手术时间较长[4,28],且有可能中转多孔手术或开腹手术。根据笔者经验,对于脐周切口的位置选择,将主操作孔、副操作孔放在脐孔直径上,两者尽量远离,可获得最大的操作空间;而观察孔放在两个操作孔之间的上方,并且使用30°镜,能获得最佳的视野,从而降低操作难度,缩短手术时间。熟练掌握腹腔镜技术,尤其腔镜下缝合打结技巧,能更好的处理阑尾根部坏疽穿孔,降低中转率。
本研究结果表明,SPLA治疗成人急性阑尾炎,较传统三孔法腹腔镜手术在切口美观度方面具有优势,在术后疼痛、生活质量方面两者相当,但单孔腹腔镜手术时间更长,且依赖于术者的腹腔镜操作技巧。SPLA的临床应用价值需要进一步多中心、大样本及长期随访研究结果证实。
[1] 欧梦川,杨显金,王崇树.腹腔镜在急腹症中的应用现状及进展[J].中国普外基础与临床杂志,2016,23(3):378-382.
[2] Meljnikov I,Radojcic B,Grebeldinger S,et al.History of surgical treatment of appendicitis[J].Med Pregl,2009,62(9-10):489-492.
[3] Aly OE,Black DH,Rehman H,et al.Single incision laparoscopic appendicectomy versus conventional three-port laparoscopic appendicectomy:A systematic review and meta-analysis[J].Int J Surg,2016,35:120-128.
[4] Vettoretto N,Cirocchi R,Randolph J,et al.Acute appendicitis can be treated with single-incision laparoscopy:a systematic review of randomized controlled trials[J].Colorectal Dis,2015,17(4):281-289.
[5] Gao J,Li P,Li Q,et al.Comparison between single-incision and conventional three-port laparoscopic appendectomy:a meta-analysis from eight RCTs[J].Int J Colorectal Dis,2013,28(10):1319-1327.
[6] Ding J,Xia Y,Zhang ZM,et al.Single-incision versus conventional three-incision laparoscopic appendicectomy for appendicitis:a systematic review and meta-analysis[J].J Pediatr Surg,2013,48(5):1088-1098.
[7] Teoh AY,Chiu PW,Wong TC,et al.A double-blinded randomized controlled trial of laparoendoscopic single-site access versus conventional 3-port appendectomy[J].Ann Surg,2012,256(6):909-914.
[8] Kang CK,Lee SY,Kang DB,et al.Application of single incision laparoscopic surgery for appendectomies in patients with complicated appendicitis[J].J Korean Soc Coloproctol,2010,26(6):388-394.
[9] 李鲁,王红妹,沈毅.SF-36健康调查量表中文版的研制及其性能测试[J].中华预防医学杂志,2002,36(2):38-42.
[10] Kapischke M,Friedrich F,Hedderich J,et al.Laparoscopic versus open appendectomy-quality of life 7 years after surgery[J].Langenbecks Arch Surg,2011,396(1):69-75.
[11] Baik SM,Hong KS,Kim YI.A comparison of transumbilical single-port laparoscopic appendectomy and conventional three-port laparoscopic appendectomy:from the diagnosis to the hospital cost[J].J Korean Surg Soc,2013,85(2):68-74.
[12] Semm K.Endoscopic appendectomy[J].Endoscopy,1983,15(2):59-64.
[13] 姜海军,宫轲.单孔腹腔镜手术进展与未来[J].中国微创外科杂志,2010,10(1):37-40.
[14] Kang BM,Hwang JW,Ryu BY.Single-port laparoscopic surgery in acute appendicitis:retrospective comparative analysis for 618 patients[J].Surg Endosc,2016,30(11):4968-4975.
[15] Kang BH,Yoon KC,Jung SW,et al.Feasibility of single-incision laparoscopic appendectomy in a small hospital[J].Ann Surg Treat Res,2016,91(2):74-79.
[16] Kim JH,Kim HY,Park SK,et al.Single-incision Laparoscopic Appendectomy Versus Conventional Laparoscopic Appendectomy:Experiences From 1208 Cases of Single-incision Laparoscopic Appendectomy.Experiences From 1208 Cases of Single-incision Laparoscopic Appendectomy[J].Ann Surg,2015,262(6):1054-1058.
[17] Liang HH,Hung CS,Wang W,et al.Single-incision versus conventional laparoscopic appendectomy in 688 patients:a retrospective comparative analysis[J].Can J Surg,2014,57(3):E89-97.
[18] Buckley FP 3rd,Vassaur H,Monsivais S,et al.Single-incision laparoscopic appendectomy versus traditional three-port laparoscopic appendectomy:an analysis of outcomes at a single institution[J].Surg Endosc,2014,28(2):626-630.
[19] Villalobos Mori R,Escoll Rufino J,Herrerías González F,et al.Prospective,randomized comparative study between single-port laparoscopic appendectomy and conventional laparoscopic appendectomy[J].Cir Esp,2014,92(7):472-477.
[20] Frutos MD,Abrisqueta J,Lujan J,et al.Randomized prospective study to compare laparoscopic appendectomy versus umbilical single-incision appendectomy[J].Ann Surg,2013,257(3):413-418.
[21] Doward LC,Gnanasakthy A,Baker MG.Patient reported outcomes:looking beyond the label claim[J].Health Qual Life Outcomes,2010,8:89.
[22] Calvert M,Blazeby J,Altman DG,et al.Reporting of patient-reported outcomes in randomized trials:the CONSORT PRO extension[J].JAMA,2013,309(8):814-822.
[23] SCARLESS Study Group,Ahmed I,Cook JA,et al.Single port/incision laparoscopic surgery compared with standard three-port laparoscopic surgery for appendicectomy:a randomized controlled trial[J].Surg Endosc,2015,29(1):77-85.
[24] Kim SJ,Choi BJ,Jeong W,et al.The feasibility of single-port laparoscopic appendectomy using a solo approach:a comparative study[J].Ann Surg Treat Res,2016,90(3):164-170.
[25] Raakow J,Liesaus HG,Neuhaus P,et al.Single-incision versus multiport laparoscopic appendectomy:a case-matched comparative analysis[J].Surg Endosc,2015,29(6):1530-1536.
[26] Lee WS,Choi ST,Lee JN,et al.Single-port laparoscopic appendectomy versus conventional laparoscopic appendectomy:a prospective randomized controlled study[J].Ann Surg,2013,257(2):214-218.
[27] Kulaylat AN,Podany AB,Hollenbeak CS,et al.Transumbilical laparoscopic-assisted appendectomy is associated with lower costs compared to multiport laparoscopic appendectomy[J].J Pediatr Surg,2014,49(10):1508-1512.
[28] Carter JT,Kaplan JA,Nguyen JN,et al.A prospective,randomized controlled trial of single-incision laparoscopic vs conventional 3-port laparoscopic appendectomy for treatment of acute appendicitis[J].J Am Coll Surg,2014,218(5):950-959.
(英文编辑:程玉刚)
Randomized controlled study between single-port versus conventional three-port laparoscopic appendectomy for adult acute appendicitis
LIUHai-long,ZENGHe-ping,LINMou-bin,etal.
DepartmentofGeneralSurgery,YangpuHospital,TongjiUniversitySchoolofMedicine,Shanghai200090,China
Objective:To compare the safety and efficacy of single-port laparoscopic appendectomy (SPLA) with conventional three-port laparoscopic appendectomy (CLA) for adult acute appendicitis.Methods:Between Jan.2014 and Dec.2015,a total of 160 adult patients with acute appendicitis were randomly assigned to SPLA group (78 cases) and CLA group (82 cases).Treatment outcomes were analyzed.Results:There was no significant difference in patients’ 24 h pain score between SPLA group and CLA group [(3.4±2.1)vs.(3.3±1.9),P=0.892]).There were no significant differences in the SF-36 health survey (P>0.05).The patient-reported cosmetic scores were better in SPLA group [(8.2±1.1) vs.(7.4±1.4),P<0.001].Operation time in SPLA group was significantly longer than that in CLA group (P<0.001).Conversion rate of surgery in SPLA group was significantly higher (P=0.013).There were no significant differences in the analgesics required (P=0.619),hospital stay (P=0.680) and complication rate (P=0.425) between the two groups.Conclusions:SPLA for adult acute appendicitis is superior to CLA with regard to cosmetic outcomes,SPLA is comparable to CLA in postoperative pain and quality of life.However,adoption of SPLA will rely on the presence of better laparoscopic expertise,and it takes more time to accomplish this procedure.
Acute appendicitis;Appendectomy;Laparoscopy;Single-port;Adult
1009-6612(2017)07-0536-05
10.13499/j.cnki.fqjwkzz.2017.07.536
上海市卫生局青年科研项目(编号:20134Y198)
曾和平,E-mail:darkknight3000@163.com
刘海龙(1981—)男,同济大学附属杨浦医院普通外科主治医师,主要从事普通外科、微创外科的研究。
R656.8
A
2017-02-23)

