类风湿关节炎和骨关节炎患者膝关节置换术后并发症的临床对照研究
程金生,李俊霞,周 静
(冀中能源峰峰集团总医院骨科,邯郸 056201)
类风湿关节炎和骨关节炎患者膝关节置换术后并发症的临床对照研究
程金生,李俊霞,周 静
(冀中能源峰峰集团总医院骨科,邯郸 056201)
目的:对比骨性关节炎(osteoarthritis,OA)和类风湿关节炎(rheumatoid arthritis,RA)患者膝关节置换术后并发症发生情况。方法:选取67例RA和78例OA患者,均行膝关节置换术治疗,观察并记录患者的术前,术后3d和5d的VAS评分、ROM评分,随访2年期间并发症发生情况,对比OA和RA患者膝关节置换术后并发症发生情况。结果:与术前相比,RA组术后5d的VAS评分明显降低,OA组术后3d,5d的 VAS明显降低,OA组术后3d,5d的VAS评分明显低于RA组。术前两组ROM评分无统计学差异,与术前相比,RA组术后3 d的ROM评分明显降低,OA组术后5d的ROM评分明显增加,OA组术后3d,5d的ROM评分明显高于RA组,随访2个年期间,RA组2年内翻修率和伤口并发症发生率均明显高于OA组,关节失稳,假体松动,下肢深静脉血栓发生率比较,无统计学差异。两组主要伤口并发症为伤口渗液,发生率相比无统计学差异。其他3种并发症发生率相比,也没有统计学差异。结论:骨关节炎患者经人工膝关节置换术治疗后,并发症发生较少,膝关节活动较术前改善明显,疼痛度减轻。
类风湿关节炎;骨关节炎;人工膝关节置换术;伤口感染;并发症
我国RA的发病率为0.3%~0.5%,OA的发病率为0.1~0.2%,患病与衰老退化、肥胖超重、生活环境和运动损伤有关[1]。病情发展至晚期时,保守治疗疗效不佳,术后炎症易复发,临床治疗仍以手术治疗为主。人工膝关节置换术常用于治疗晚期OA和OR,能够消除疼痛、纠正畸形,改进膝关节的稳定性和活动度,进而提高患者的生活质量[2]。虽然膝关节置换术有着特有的疗效,但术后仍然存在诸如伤口感染、假体松动、深静脉血栓等并发症。为了提高手术疗效,有必要减少人工膝关节置换术后并发症。然而两种疾病发病机制并不一样,对人工膝关节置换术后并发症影响究竟如何报道较少。为此,回顾性分析来我院治疗的67例RA和78例OA患者,现报告如下:
1 资料与方法
1.1 一般资料选取67例RA和78例OA患者,年限:2011年3月~2015年3月,纳入标准:①入选患者分别符合RA和OA的诊断标准;②所有患者均采用人工膝关节置换术治疗;③经本院伦理委员会同意,术前每位患者均签署书面知情同意书。排除标准:有下肢骨折、膝关节骨不连、膝关节手术史、骨肿瘤患者。两组患者入院后根据病理类型分组,RA组(67例)男41例,女26例,平均年龄(64.9±7.3)岁,BMI指数为(23.8±4.3)kg/m2,OA组(78例)男48例,女30例,平均年龄(65.2 ±6.5)岁,BMI指数为(24.6±3.8)kg/m2,两组一般资料具有可比性(P>0.05)。
1.2 手术方法及处理术前所有患者常规预防性应用头孢曲松钠,全麻,手术由同一组医师完成。选取膝前正中皮肤行10~15 cm手术切口,髌旁内侧入路,彻底清除增生滑膜或骨赘,并充分止血,胫骨近端、股骨远端截骨,平衡软组织,选择合适型号膝关节假体置入,骨水泥固定10~13 min,X线确定固定良好后,伸屈膝关节检查活动度及稳定情况,术后关节腔内放置引流管,缝合手术切口,绷带加压包扎。术后给予镇痛、抗凝治疗。术后3 d在支具下进行负重锻炼。
1.3 观察指标(1)痛觉感受和关节活动度:采用VAS量表对术前,术后3d,5d的痛觉感受进行评分,分值范围0~10分,分值越低说明痛觉感受越轻;采用膝关节ROM对术前,术后3d,5d的手术效果进行评分,满分100分,分数越高说明膝关节活动度越好;(2)随访2年期间,观察并记录两组患者2年内翻修,关节失稳,假体松动,伤口并发症,下肢深静脉血栓发生情况;(3)观察并记录两组患者伤口并发症发生情况。
1.4 统计方法所有数据采用SPSS 17.0软件进行分析,将调查统计的内容作为变量,计量资料以,±s表示,采用t检验,计数资料以%表示,采用χ2检验,以P<0.05为差异有统计学意义。
2 结果
2.1 痛觉和关节活动度比较术前两组VAS评分无统计学差异(P>0.05),与术前相比,RA组术后5d的VAS评分明显降低,OA组术后3d,5d的 VAS明显降低(P<0.05),OA组术后3d,5d的VAS评分明显低于RA组(P<0.05)。术前两组ROM评分无统计学差异(P>0.05),与术前相比,RA组术后3 d的ROM评分明显降低,OA组术后5d的ROM评分明显增加(P<0.05),OA组术后3d,5d的ROM评分明显高于RA组(P<0.05),见表1。
2.2 并发症比较随访2个年期间,RA组2年内翻修率和伤口并发症发生率均明显高于OA组(P<0.05),关节失稳,假体松动,下肢深静脉血栓发生率比较,无统计学差异(P>0.05),见表2。
2.3 伤口并发症从表3可知,两组主要伤口并发症为伤口渗液,发生率相比无统计学差异(P>0.05)。其他3种并发症发生率相比,也没有统计学差异(P>0.05)。
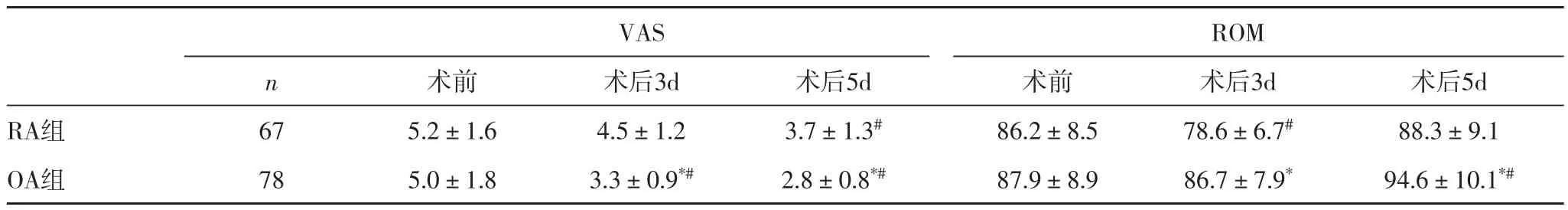
表1 两组VAS和ROM评分对比
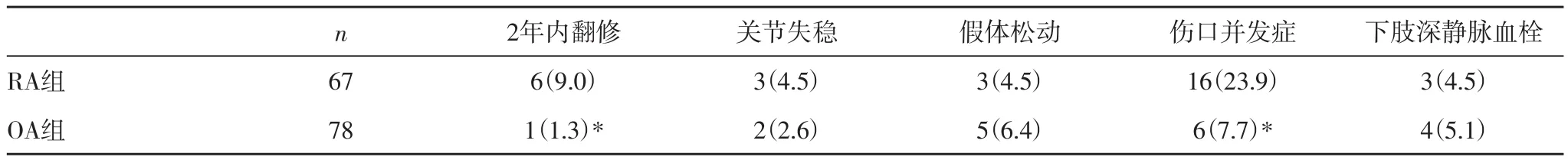
表2 两组术后并发症对比 [n(%)]

表3 两组伤口并发症对比 [n(%)]
3 讨论
OA和RA均是临床上常见的外科疾病,老年人是上述疾病发生的高危人群,RA是主要以软骨、滑膜组织病变为主,OA是主要以关节劳损、关节畸形、关节软骨破坏为主的退行性疾病,两类关节炎均会导致膝关节活动受限,关节疼痛、僵硬和肿胀[3]。
人工膝关节置换术是治疗OA和RA晚期常用的治疗手段,能迅速缓解患者疼痛,恢复患者的运动功能[4]。随着我国人口老龄化速度不断加剧,OA和RA发病率也逐年增长,越来越多的患者将会应用到这一技术[5]。但由于膝前关节特殊的生理解剖结构,表现为软组织薄弱、血运较差,人工膝关节置换术后易出现皮肤坏死等伤口并发症[6-7]。再加上膝关节炎症带来的疼痛感较严重,难以忍受,部分患者在术前长期服用糖皮质激素和免疫抑制剂,导致全身免疫系统紊乱,抵抗力下降,进而增加术后伤口感染风险。因此,有效降低术后并发症,提高患者生活质量及手术效果是OA和RA的手术治疗目的[8]。
本研究中,采用VAS量表对患者术前术后疼痛感觉进行评价,RA组患者直到术后第5天疼痛感才开始有所减轻,而OA组患者术后第3d疼痛感就开始减轻,并且术后3天,5天的疼痛感均轻于RA组。分析原因,可能为RA组患者滑膜组织血管神经增生,使患者的疼痛敏感性增加,经人工膝关节置换术治疗后,疼痛感未能迅速降低。本研究采用关节活动度来评价手术治疗效果,RA组术后3 d的ROM评分明显低于术前评分,OA组术后3d的ROM评分略低于术前评分。分析原因,除了与刚进行完手术患者不便活动有关外,还与RA患者滑膜及软骨组织破坏程度较大,不利于肢体活动有关。随访2个年期间,RA组2年内翻修率和伤口并发症发生率均明显高于OA组,关节失稳,假体松动,下肢深静脉血栓发生率比较,无统计学差异。有研究表明,RA是人工膝关节术后感染翻修的危险因素。本研究也证实了RA患者术后2年翻修率明显高于OA组患者,翻修多与术后假体松动、伤口感染有关。进一步研究发现,伤口渗液为主要伤口并发症。分析原因,可能与患者病程周期较长,术前长期应用糖皮质激素有关。浅层伤口渗液可不进行处理,伤口可自行愈合。若为深层伤口渗液,甚至裂口暴露至假体,应及时给予抗生素治疗,并且停止术后康复训练,以免关节囊及皮肤伤口的继续撕裂,增加感染风险。
综上所述,骨关节炎患者经人工膝关节置换术治疗后,并发症发生较少,膝关节活动较术前改善明显,疼痛度减轻。
[1] Sun Z, Hesler BD, Makarova N, et al. The Association Between Rheumatoid Arthritis and Adverse Postoperative Outcomes: A Retrospective Analysis[J]. Anesth Analg, 2016, 122(6): 1887-1893.
[2] 安晓, 张琦, 龚科, 等. 骨性关节炎与类风湿关节炎患者单侧膝关节置换术后围术期效果比较[J]. 解放军医学院学报, 2014, 35(10): 1022-1024.
[3] Szentpetery A, Heffernan E, Haroon M, et al. Striking difference of periarticular bone density change in early psoriatic arthritis and rheumatoid arthritis following anti-rheumatic treatment as measured by digital X-ray radiogrammetry[J]. Rheumatology (Oxford), 2016, 55(5): 891-896.
[4] Mullen MB, Saag KG. Evaluating and mitigating fracture risk in established rheumatoid arthritis[J]. Best Pract Res Clin Rheumatol, 2015, 29(4-5): 614-627.
[5] 彭旭, 叶永杰. 类风湿与骨关节炎全膝关节置换术后并发症分析[J]. 医药前言, 2016, 6(6): 207-208.
[6] Yamamoto Y, Turkiewicz A, Wingstrand H, et al. Fragility Fractures in Patients with Rheumatoid Arthritis and Osteoarthritis Compared with the General Population[J]. J Rheumatol, 2015, 42(11): 2055-2058.
[7] 孔祥喆, 管德印, 蒋刚. 旋转平台假体人工膝关节置换在类风湿性关节炎中的临床应用[J]. 国际医药卫生导报, 2016, 22(2): 198-200.
[8] Collins KH, Paul HA, Reimer RA, et al. Relationship between inflammation, the gut microbiota, and metabolic osteoarthritis development: studies in a rat model[J]. Osteoarthritis Cartilage, 2015, 23(11): 1989-1998.
Com parison of postoperative com p lications of knee arthroplasty in patients w ith rheumatoid arthritis and osteoarthritis
Cheng Jin-sheng, Li Jun-xia, Zhou Jing
(Department of orthopedics, Jizhong Energy Fengfeng Group Hospital, Handan 056201, China)
Objective Comparing postoperative complications of knee arthroplasty in patients with rheumatoid arthritis and osteoarthritis. M ethods 67 patients withRA and 78 patients with OA were selected, they were given knee joint replacement treatment. The postoperative complications of knee arthroplasty in patients with rheumatoid arthritis and osteoarthritis were evaluated by VAS scores before operation, after 3 days and 5 days operation, ROM scores and complications during 2 years follow-up. Results Compared with the scores before operation, the VAS scores were decreasedafter 5 days operation in the RA group. The VAS scores were decreased after 3 days and 5 days operation in the OA group. In the OA group, the VAS scores were lower than that of the RA group after 3 days and 5 days operation. Compared with the scores before operation, the ROM scores after 3 days operation were decreased in the RA group. The ROM scores were increased after 5 days operation in the OA group. In the OA group, the ROM scores were higher than that of the RA group after 3 days and 5 days operation. During 2 years follow-up, the rate of revision and wound complication of RA group were higher than that of the OA group. There were no statistical significance on the joint instability, prosthesis loosening and deep venous thrombosis of lower extremity. The major wound complication was wound infiltration and there were no statistical significance on complications between two groups. There were no statistical significance on the rest of complication rate. Conclusion After operation, the complications were less in osteoarthritis patients. The knee joint motion was improved obviously and the pain was reduced.
rheumatoid arthritis; osteoarthritis; total knee arthroplasty; wound infection; complication
R593.22
A
1673-016X(2017)04-0085-03
2017-03-12
李俊霞,E-mail:lijunxia_197404@med icinepaper.com.cn

