异位胸腺瘤5例影像学表现的临床分析
董科+崔璨+王利霞+温广华


[摘要] 目的 探讨异位胸腺瘤(ET)的影像学表现,以提高对ET的认识。 方法 回顾性分析浙江大学金华中心医院2010~2016年经病理证实的5例ET临床及影像学资料。其中CT平扫+增强扫描3例,CT平扫并MRI增强扫描1例,CT平扫+增强并PET/CT扫描1例。 结果 5例ET临床表现为乏力2例、无症状3例。发生于下颈部2例,后下纵隔2例,左侧胸膜累及纵隔1例。影像学5例平扫CT均表现为密度均匀,CT值范围33~51 HU,4例增强扫描动脉期结节状强化,静脉期均匀强化,平均强化幅度为34 HU;1例MRI表现为呈等T1等T2信号,增强扫描明显均匀强化;1例PET/CT表现为18F-FDG代谢明显增高。 结论 异位胸腺瘤少见,临床表现缺乏特异性,本组5例影像学表现具有一定特征:平扫密度均匀,增强扫描明显强化,PET/CT呈高代谢。正确认识其表现有助于提高诊断准确性。
[关键词] 异位胸腺瘤;CT;MRI;PET/CT
[中图分类号] R746.1;R655.7 [文献标识码] A [文章编号] 1673-7210(2017)03(b)-0127-05
Imaging features of ectopic thymoma:report of five cases and review of literature
DONG Ke1 CUI Can2 WANG Lixia3 WEN Guanghua1▲
1.Department of Nuclear Medicine, Jinhua Hospital of Zhejiang University, Zhejiang Province, Jinhua 321000,China; 2.Department of Radiology, Jinhua Hospital of Zhejiang University, Zhejiang Province, Jinhua 321000, China; 3.Department of Pathology, Jinhua Hospital of Zhejiang University, Zhejiang Province, Jinhua 321000, China
[Abstract] Objective To investigate the imaging features of ectopic thymoma, in order to improve the understanding of ectopic thymoma. Methods From 2010 and 2016, the clinical and radiographic data of 5 cases with ectopic thymoma proved by pathological results were analyzed retrospectively. 3 patients underwent enhanced CT examination, 1 patient underwent unenhanced CT and contrast-enhanced MRI examination, 1 patient underwent enhanced CT and PET/ CT examination. Results Among 5 cases, 2 cases showed symptoms of fatigue, while 3 cases showed no symptoms. 2 lesions were located in the lower neck, 2 cases were in the posterior-inferior mediastinum, 1 case was in the left pleura invaded in mediastinum. On unenhanced CT, 5 tumors showed homogeneous density (CT value 33-51 HU). On arterial phase of the enhanced CT of 4 tumors showed nodular enhancement, and on the vein phase showed homogeneous enhancement. Aaverage enhancement degree was 34 HU. On MR images, 1 tumor showed iso-signal both on T1WI and T2WI, obvious homogeneous enhancement on contrast MR images. On PET/CT images, 1 tumor showed accumulation of 18F-FDG. Conclusion Ectopic thymoma is a rare neoplasm and the clinical manifestation were lack of specificity. All the 5 cases exhibits some imaging characteristics, such as homogeneous density on unenhanced CT, obvious enhancement, accumulation of FDG, which may be of value in the diagnosis of ectopic thymoma.
[Key words] Ectopic thymoma; CT; MRI; PET/CT
胸腺瘤起源于胸腺上皮組织,多位于前上纵隔,位于其他部位者称为异位胸腺瘤(ectopic thymoma,ET)。ET较罕见,可发生于中后纵隔、颈部、胸腔等部位[1-8]。笔者遇到5例,本文结合国内外文献进行分析,旨在提高对本病的认识。
1 资料与方法
1.1 一般资料
回顾性分析2010~2016年浙江大学金华中心医院经外科手术或粗针穿刺病理确诊的5例ET患者的临床及影像学资料。其中男1例,女4例;年龄45~64岁。临床表现为乏力2例,无症状3例。其中CT平扫增强3例,CT平扫并MRI增强1例,CT平扫增强并PET/CT扫描1例。
1.2 检查方法
本组患者CT扫描采用西门子emotion 16螺旋CT机,扫描参数:电压120 kV、电流150 mA,层厚5 mm,螺距1.5;扫描范围从上颈部至上腹部,其中4例患者在平扫后行增强扫描;对比剂使用300 mgI/mL碘海醇,总量80 mL,速率3.0 mL/s。l例患者MRI检查采用Siemens Magnetom Avanto 1.5T超导型磁共振成像扫描仪,表面线圈,采用自旋回波(SE)TWI(TR 500~600 ms、TE 10~15 ms),快速自旋回波(TSE)T2WI(TR4000 ms,TE 80~120 ms)及脂肪抑制快速自旋回波TWI(TR 3600~4500 ms,TE 80~120 ms),矩陣320×320,层厚5 mm,层间距0.5~1.0 mm,平扫结束后经肘静脉以2.5 mL/s流速注射钆喷酸葡胺(Gd-DTPA)15 mL行增强扫描。1例患者PET/CT检查采用德国Siemens Biograph 64 PET/CT仪,18F-FDG由浙江安迪科正电子技术有限公司提供,放化纯>95%。患者空腹6 h,在安静环境下休息至少20 min。检查前空腹血糖<6.1 mmol/L。由静脉按体量注射18F-FDG 2.22~4.44 MBq/kg,休息55~60 min,排尿后行图像采集。扫描范围从颅底至股骨上段。先行CT扫描,电压120 kV,电流100 mA,矩阵512×512,患者保持平静呼吸以便与PET相匹配。后行PET显像三维采集,每床位采集1.5 min,共采集5~6个床位。采用OSEM算法和基于CT的衰减校正,PET及CT图像扫描层厚均为5 mm,以系统软件进行图像融合;根据病变位置勾画ROI后由工作站软件自动计算SUVmax。
2 结果
2.1 肿瘤的部位、形态与大小
5例ET病灶发生于下颈部2例,后下纵隔2例,左侧胸膜累及纵隔1例。2例肿块呈类圆形,1例呈椭圆形,2例呈不规则形。病灶最大横断面7.4 cm×6.3 cm~5.2 cm×2.1 cm。
2.2 影像学表现
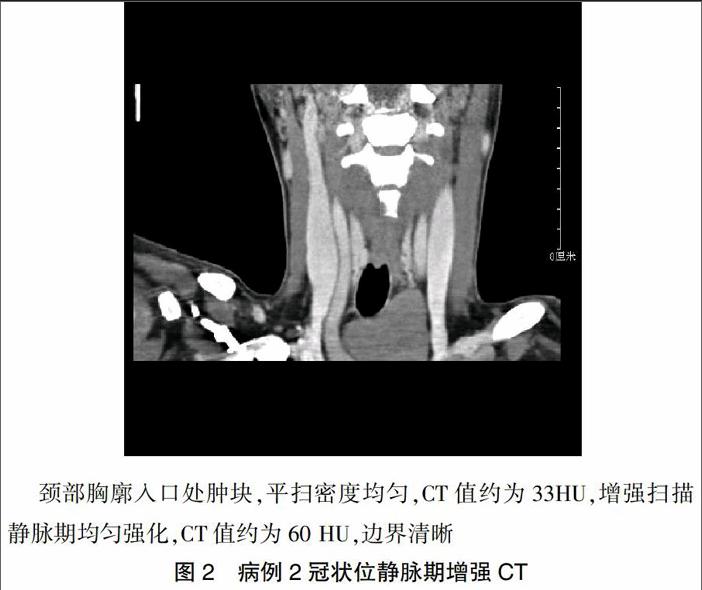
2.2.1 肿瘤的CT表现 5例ET均行CT平扫检查,CT值范围33~51 HU,密度均匀。增强扫描4例,动脉期结节状或雪花状强化,静脉期均匀强化,较平扫升高48~96 HU,平均强化幅度为34 HU,邻近组织结构受压移位,其中3例CT表现见(图1~3)。
2.2.2 肿瘤的MR表现 病例4肿瘤位于后下纵隔,T10椎体水平左侧椎旁,椭圆形,MRI呈等T1等T2信号,增强扫描明显均匀强化(图4),与邻近结构分界清晰。
2.2.3 肿瘤的PET/CT表现 病例5肿瘤表现为左侧胸膜弥漫性不规则结节状增厚,后下纵隔多发结节,密度均匀,18F-FDG放射性摄取明显增高,SUVmax为11.3(图5)。
2.3 病理学表现
4例肿瘤手术切除,大体标本示肿瘤色暗红,包膜均较完整,切面鱼肉状;1例经粗针穿刺活检。5例病理学HE染色FNAC涂片,可见多量退变淋巴细胞,细胞分化欠成熟,其间夹杂少量圆形上皮样细胞;免疫组化:CK19染色(+)(图6)。5例均确诊为ET,其中AB型及B1型各2例,B2型1例。
3 讨论
胸腺瘤是最常见的纵隔肿瘤之一,多起源于胸腺上皮细胞或淋巴细胞。影像学上,胸腺瘤多为软组织密度,平扫CT值在40 HU以上;增强扫描可见中度或均匀强化。MRI检查,常表现为位于前纵隔或前上纵隔的圆形、卵圆形或分叶状肿块,信号多均匀、中等强度;当瘤体出现液化坏死时,可表现为不规则的高低MR信号区。
ET形成原因尚不明确。胚胎发育期胸腺组织起源于第3(或4)对咽囊。第6周时咽囊上皮增生形成左右两条细胞索,向胚体尾端伸长,末端抵达胚体内胸腔,增生变大并融合,第8周形成两侧叶定位于前上纵隔,此时细胞索退化消失。目前多认为如果退化不全,残余细胞则在颈部、甲状腺、胸腔等部位形成异位胸腺组织;另一种解释为未明确的原位胸腺瘤转移而成[9]。传统的胸腺瘤病理分类有多种,目前多采用1999年WHO分类方法:A型胸腺瘤:即髓质型或梭型细胞胸腺瘤。AB型胸腺瘤:即混合型胸腺瘤。B型胸腺瘤分为3个亚型,B1型胸腺瘤:即富含淋巴细胞的胸腺瘤、淋巴细胞型胸腺瘤、皮质为主型胸腺瘤或类器官胸腺瘤;B2型胸腺瘤:即皮质型胸腺瘤;B3型胸腺瘤:即上皮型、非典型、类鳞状上皮胸腺瘤或分化好的胸腺癌。C型胸腺瘤:即胸腺癌,组织学上此型较其他类型的胸腺瘤更具有恶性特征。本组患者病理AB型和B1型各2例,B2型1例。
ET临床少见[10-11],其发生率占胸腺瘤的2%~4%,女性多见。本组患者男女比例为1∶4。肿块较小时,临床多无症状。肿块较大,多表现为占位和局部压迫症状,与其发生的部位不同,而表现各异。如发生于颈部及纵隔[12],多表现为肿块、疼痛和压迫症状。本组病例1、病例2表现为颈部无痛性肿块,压迫邻近组织器官。病例3、病例4肿块较小,无明显临床症状及体征,为影像学检查偶然发现。肺及胸膜的ET报道较罕见[13-14],可出现胸闷、气促、咳嗽和胸痛等。本组病例5患者因乏力2周而胸部平扫CT检查发现。由于ET的临床表现无特异性,尤其是不合并重症肌无力患者,其诊断较困难。
ET的影像检查主要有CT和MRI[15]。通过回顾性分析本组病例影像学资料,并结合相关文献[1-15],笔者认为ET影像表现有以下特点:①病灶主要位于下颈部、后纵隔及胸腔。②病灶多较大,单发,类圆形,边界清晰;多发可呈不规则形。③CT、MRI平扫大多表现为密度均匀,增强扫描动脉期明显不均匀强化,呈结节状或雪花点状,静脉期强化均匀。④PET/CT呈均匀高代谢,囊变及钙化少见。
依照ET發生部位,需要与不同的肿瘤相鉴别。发生于下颈部ET,需与甲状腺或甲状旁腺肿瘤相鉴别,肿瘤的定位是诊断的关键[16]。本组病例1、病例2的CT表现为下颈部类圆形肿块,呈中、重度强化(30~55 HU),邻近组织器官受压,但分界尚清。发生于后纵隔的ET,需要与神经源性肿瘤相鉴别。神经鞘瘤有包膜,病变往往较大而单发,内可见坏死液化;神经纤维瘤大多为实性,常多呈梭形,强化幅度较低[17-18]。病例3、病例4的CT及MRI表现为后纵膈脊柱旁软组织密度占位,密度均匀,中度强化,与神经纤维瘤表现相似,鉴别较困难。发生于胸膜的ET,影像表现与胸膜间皮瘤及转移瘤相似。本组病例5表现为胸膜多发不规则增厚,CT增强扫描强化幅度30 HU,18F-FDG代谢明显增高,SUVmax:11.3;但无胸膜间皮瘤常见的胸腔积液,PET/CT亦未找到转移瘤的原发病灶。因此当胸膜多发结节伴有重症肌无力等症状,而前纵隔内未发现肿瘤时,应考虑到胸膜异位胸腺瘤的可能。
细针抽吸细胞学检查容易误诊[19-21]。定性诊断仍依靠组织病理学及免疫学。本组病例1、5穿刺细胞学涂片表现为多量小淋巴细胞,而误诊淋巴瘤,后经组织病理学及免疫学确诊为异位胸腺瘤。
临床上,ET的治疗原则与典型胸腺瘤一致,首选手术切除。相关文献报道[22],非侵袭性胸腺瘤(Ⅰ期)完全切除包膜完整者无须放疗,5、10年生存率分别为90%和80%。如果肿瘤残余,除了A或AB型胸腺瘤外,还应行术后放疗。对于肿瘤>5 cm、有肉眼侵犯或种植的其他类型胸腺瘤,切除后应常规辅以放疗。辅助放化疗有助于减少复发及转移。胸腺瘤预后取决于分期、组织学类型、切除的完整性、MG、增生指数,DNA倍体等因素。本组病例1、2、3、5的患者,手术切除肿瘤包膜完整,均未见进行放化疗,随访复查至今未见肿瘤复发。病例4从胸部CT发现病灶到穿刺活检免疫组化确诊,间隔不到3个月。因乏力症状好转,拒绝手术及进一步治疗,现无明显异常临床症状及体征。
总之,ET未必有重症肌无力的临床表现,肿瘤较小时多无症状,肿块较大时压迫邻近结构时可表现出相应症状。多发生于下颈部、后纵隔及胸腔。CT及MRI检查肿块大多密度均匀,增强扫描明显强化,PET/CT呈高代谢。依其发生部位不同,需与甲状腺、神经源性、转移性等肿瘤相鉴别。正确认识其表现有助于提高诊断准确性。确诊依赖于手术或穿刺活检病理免疫学检查。
[参考文献]
[1] Arai H,Rino Y,Fushimi K,et al. Pericardial ectopic thymoma presenting with cardiac tamponade:report of a case [J]. Surg Today,2015,45(9):1200-1204.
[2] Kubo H,Nakasuga C,Tada K,et al. Solitary ectopic thymoma at ligamentum arteriosum; report of a case [J]. Kyobu Geka,2013,66(3):251-254.
[3] Taweevisit M,Sampatanukul P,Thorner P S. Ectopic thymoma can mimic benign and malignant thyroid lesions on fine needle aspiration cytology:a case report and literature review [J]. Acta Cytol,2013,57(2):213-220.
[4] Amodeo G,Cipriani O,Orsini R,et al. A rare case of ectopic laterocervical thymoma [J]. Craniomaxillofac Surg,2013, 41(1):7-9.
[5] Kim H S,Lee H J,Cho S Y,et al. Myasthenia gravis in ectopic thymoma presenting as pleural masses [J]. Lung Cancer,2007,57(1):115-117.
[6] Pai K R,Thonse V R,Azadeh B,et al. Ectopic thymoma of the chest wall [J]. Interact Cardiovasc Thorac Surg,2005, 4(1):9-11.
[7] Caramori G,Calia N,Pasquini C,et al. Ectopic thymoma simulating a pericardial cyst [J]. Monaldi Arch Chest Dis,2005,63(4):230-233.
[8] Azoulay S,Adem C,Gatineau M,et al. Pericardial ectopic thymoma [J]. Virchows Arch,2005,446(2):185-188.
[9] Pai KR,Thonse VR,Azadeh B,et al. Ectopic thymoma of the chest wall [J]. Interact Cardiovasc Thorac Surg,2005, 4(1):9-11.
[10] Minniti S,Valentini M,Pittali L,et al .Thymic masses of the middle mediastinum:report of 2 cases and review of the literature [J]. Thorac Imaging,2004,19(3):192-195.
[11] Ko SF,Tsai YH,Huang HY,et al. Retrotracheal thymoma masquerading as esophageal submucosal tumor [J]. World J Gaslroenlerol,2005,1l(20):3165-3166.
[12] Shien K,Shien T,Soh J,et al. Ectopic cervical thymoma:a case report with 18F-fluorodeoxyglucose positron emis?鄄sion tomography findings [J]. Acta Med.Okayama,2012, 66(4):357-361.
[13] Yamazaki K,Yoshino I,Oba T ,et al. Ectopic pleural thymoma presenting as a giant mass in the thoracic cavity [J]. Ann Thorac Surg,2007,83(2):315-317.
[14] Kitada M,Sato K,Matsuda Y,et al. Ectopic thymoma presenting as a giant intrathoracic tumor:a case report [J]. World J Surg Oncol,2011,9(3):66-69.
[15] 廖美焱,周云峰,張在鹏,等.异位胸腺瘤CT与MRI表现[J].中华放射学杂志,2007,41(8):889-891.
[16] 尉志红,樊上飞,靳宏星.甲状旁腺良性肿瘤的CT表现及鉴别诊断[J].中国中西医结合影像学杂志,2016, 14(1):81-83.
[17] 韩晶,沈文荣,郭震,等.颈部外周神经源性肿瘤的影像学诊断[J].临床放射学杂志,2002,21(1):30-32.
[18] 毕伟,丁长青,余磊,等.29例心包转移瘤的CT诊断分析[J].中国现代医生,2015,53(32):121-124.
[19] Pal KR,Thonse VR,Azadeh B,et al. Ectopic thymoma of the chest Wall [J]. Interact Cardio Vasc Thorac Surg,2005, 4(1):9-11.
[20] Ponder TB,Collins BT,Bee CS,et al. Diagnosis of cervical thymoma by fine needle aspiration biopsy with flow cytometry:a case report [J]. Acta Cytologica,2002,46(6):1129-1132.
[21] Chang ST,Chumag SS. Ectopic cervical thymoma:a mimic of T-lymphoblastic lymphoma [J]. Pathol Res Pract,2003, 199(9):633-635.
[22] Venuta F,Rendina EA,Anile M,et a1. Thymoma and thymic carcinoma [J]. Gen Thorac Cardiovasc Surg,2012, 60(1):1-12.