Influencing factors of inpatient expenditure pattern for cancer in China, 2015
Lan Lan, Yue Cai, Tao Zhang, Ruixian Wu, Ming Xue, Qun Meng,
1West China School of Public Health, Sichuan University, Chengdu 610041, China;2Center for Health Statistics and Information, National Health and Family Planning Commission, Beijing 100032, China
Influencing factors of inpatient expenditure pattern for cancer in China, 2015
Lan Lan1*, Yue Cai2*, Tao Zhang1, Ruixian Wu2, Ming Xue2, Qun Meng1,2
1West China School of Public Health, Sichuan University, Chengdu 610041, China;2Center for Health Statistics and Information, National Health and Family Planning Commission, Beijing 100032, China
Objective:We analyzed the proportion of cancer-caused hospitalization expenses in total hospitalization expenses from national authoritative data and explored influencing factors of the proportion so as to provide effective data information for more rational utilization of health resources.
Cancer; expenditure pattern; multilevel; China
View this article at: http://dx.doi.org/10.21147/j.issn.1000-9604.2017.01.02
Introduction
Since the 1970s, incidence rate and mortality for cancer have been rising in China. Cancer has become the first killer of human in the 21st century. Based on the data of China National Cancer Center, the crude morbidity rate of cancers in 2012 has reached 264.85/100,000 and the crude mortality rate of cancers has reached 161.49/100,000 (1). About 13% of death in Chinese residents (1 out of 7–8 deaths) was caused by cancer (2). Cancer not only seriously affects the health of the residents, but also causes heavy economic burden to family and society. The prevention and treatment for cancer has become a major public health problem in China. In 2010, the total expenditure for the prevention and treatment of cancer was 94.84 billion RMB (13.79 billion US dollars), accounting for 5.14% of the total health expenses and 0.24% of gross domestic product (GDP) in China at the same period (3). In 2015, the totalexpense for cancer in tumor special hospitals reached 50.76 billion RMB (7.38 billion US dollars) (4).
Information on hospital expenditure is an important input to the economic and financial analyses of many types of health interventions, and is also essential for budgeting and planning exercises. Previous studies (5,6) mainly focused on the quantification of the cost of cancer, which is an absolute number and cannot account for the cancercaused proportion of health resources in various diseases. Moreover, analysts estimating the costs of health interventions requiring hospitalization often cut corners because they lack data and the costs of undertaking full step-down costing studies are high. They sometimes use the costs taken from a single hospital; and sometimes use simple rules of thumb for allocating total hospital costs (7,8). To fill the gap, for the first time, we analyzed the proportion of cancer-caused hospitalization expenses in total hospitalization expenses from the national authoritative data, explored the influencing factors of the proportion, and provided effective data information for more rational utilization of health resources, so as to control unreasonable medical expenses, reduce the economic burden, and promote health care system reform and the management of health care costs. Furthermore, this study could be used to understand possible influencing factors of inpatient expenditure pattern for cancer (IEPC), and provides evidence for future studies to predict costs in regions where data were not available.
Materials and methods
Data source
The related information on inpatient expenditure for cancer in China in 2015 is from the inpatient medical record home page (IMRHP) of general hospitals, whose main contents include patients’ demographic information, code of diagnosis, code of surgery, results of treatments, hospitalization expenses, etc. The IMRHP was quarterly reported by the general and special hospitals in the secondary and above levels through the Health Statistics and Report System of Center for Health Statistics and Information (CHSI), National Health and Family Planning Commission, China. Hospital information reported by every hospital in China is from hospital information database. Hospitals update their information as long as the information changed through the Health Statistics and Report System of CHSI. Hospital information mainly includes hospital’s property, level, number of staff, number of beds, situation of equipment, volume of medical services, etc. Provincial data, including GDP per capita, the proportion of urban population, age structure, sex ratio and so on, are from China Health and Family Planning Statistical Yearbook 2016.
Every year before March, national CHSI checks the completeness and validity of IMRHP and hospital information of last year by provincial level and informs the provincial CHSIs of the results of data quality control. Besides, national CHSI carries out data quality supervision and inspection regularly, and helps the provinces with poorer data quality to improve their data’s completeness and validity.
Statistical analysis
Brief conceptual framework
Considering the possible clustering in IEPC, we used multilevel model to explore the influencing factors of ratio. As the ratio after logarithmic transformation obeys normal distribution, we proposed two-level (hospital level and province level) linear regression model. We used SAS software (Version 9.3; Institute Inc., Cary, USA) to clean data, explore analysis and choose explanatory variables, and modeled by MLwiN (Version 2.02; Multilevel Models Project Institute of Education, London, UK).
Multilevel model
To keep the consistency with World Health Organizaiton relative study (9) we applied linear regression model to estimate the influencing factors of IEPC. To better explain the potential clustering and differences of the proportions, we proposed two-level linear regression model, with hospital as the low level and province as the high level, taking account of the potential homogeneity with similar disease distribution in provinces (10).
Outcome variable
As the outcome variable, IEPC’s numerator is the total hospitalization expenditure of patients primarily diagnosed as cancer (International Classification of Diseases 10: C00-C97) in a hospital and denominator is the total hospitalization expenditure in a hospital. A total of 40.76 million IMRHP from 2,886 general hospitals were included in the analysis.
Explanatory variables


Results
Descriptive analysis
We analyzed 40.76 million IMRHP of 2,886 hospitals in 30 provinces of China in 2015 except Tibet because of few data on Tibet. The distribution of IMRHP is presented inFigure 1. There was a big difference in the number of the eligible reported IMRHP among provinces in China in 2015. The IEPC of the total inpatient records was 11.46% in China in 2015, ranging from 3.03% to 19.61% across provinces. Top three provinces on IEPC was Fujian, Jiangsu and Zhejiang, whose IEPC were 19.61%, 18.29% and 16.35%, respectively. Guizhou, Shandong and Shaanxi had the least proportion of IEPC, which were 3.03%, 3.92% and 4.74%, respectively. Due to the skewed distribution for IEPC, we used median and inter-quartile range as presented inTable 1.
The number of public hospitals was approximately 6 times as many as that of private hospitals, while the median of IEPC% of public hospitals was about 2 times as high as that of private hospitals. The number of secondary hospitals amounted to 2,071, which was far more than the numbers of primary and tertiary hospitals. For IEPC%, tertiary hospitals were the highest, secondary hospitals were about a quarter of tertiary hospitals, and the remaining was approximately one seventh of the tertiary. Despite middle regions had the least number of hospitals than the west and the east regions, the median of IEPC% of east regions was slightly higher than that of the middle, and that of west regions was the least (Table 2).
Model results
Single factor analysis and correlation analysis were carried out for explanatory variables. We established a variance covariance matrix to analyze the correlations in all variables, which were divided into four categories: property, level, scale and efficiency of hospital. The results of correlations showed that staff and income variables are highly correlated with beds (Pearson correlation coefficient >0.9). The highly correlated variable (Pearson correlation coefficient >0.75) with the rest variables in each category was selected as representative. Finally, we selected four representative types: hospital property (1 is a public hospital, 0 is a private hospital), hospital level (1, 2, 3 are primary, secondary and tertiary hospital, respectively), number of beds in a hospital, and bed utilization in a hospital (numerator is bed-days used by patients and denominator is total beddays in hospital).
Variance covariance matrix for provincial variables showed that the region (the east, middle and west of China) and life expectancy per capita are highly correlated with GDP per capita. According to single factor liner regression model, the population variable had no statistical significance. In the end, the provincial variables include: GDP per capital, age-standardized mortality for cancer(12), proportion for inpatient outside of home province (numerator is the total number of trans-provincial inpatients and denominator is the total number of provincial inpatients), ratio of population aged 15–64 years old, ratio of population ≥65 years old, and sex ratio.
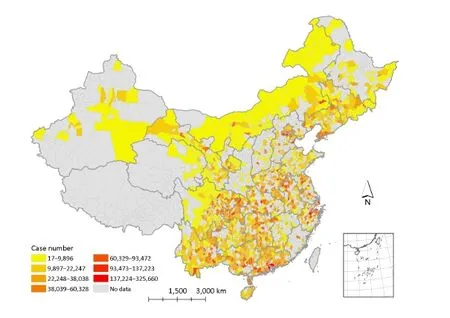
Figure 1 The distribution for inpatient medical record home page (IMRHP) in China, 2015. The case number is the number of IMRHP in a county.
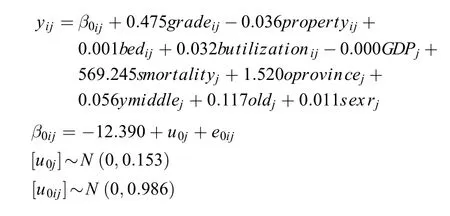
Then we put the selected variables one by one into the model to model. As shown in model 0 without any explanatory variables, also called zero model, second-level’s residual had statistically significant difference, suggesting the IEPC in a province having homogeneity. When we put the variables successively in the model, we found that hospital level and number of beds in a hospital had statistical significance, and the rest of the explanatory variables showed no significance. The interpreted proportion of the variation reached 50.65% in the final model. The residual normal figures of hospital level and province level were similar to a straight line, indicating that the hypothesis of first level and second level’s residual obeying normal distribution is reasonable and the application of the above model is correct. Fixed coefficient of each variable is presented inTable 3. The results of final model are as follows:
Discussion
Studying influencing factors of IEPC in China can provide evidence for more reasonable allocation of limited health resources. The results show that cancer takes up a large amount of health resources, strengthening the importance of greater attention. Additionally, IEPC in a high level has clustering, namely that there is heterogeneity between provinces and similarity within a province.
Model results demonstrate that hospital level and number of beds are the influencing factors of IEPC. We can see that the higher the level of hospitals, the higher the value of IEPC. This result can be explained by the fact that the patients with severe diseases tend to visit the hospitalswith higher level. Although the levels can reflect the ability of diagnosis and treatment of hospitals in a certain level, there still is a high variation of inpatient volume among hospitals in the same level. The number of beds in tertiary hospitals ranges from 400 to 2,000. Our study shows that the expenditure of cancer was concentrated in hospitals with more beds. Briefly, rising one level of the hospital led to the increase of 0.475 natural logarithm units of IEPC averagely. The number of beds increasing 1,000 each made the natural logarithm of IEPC increase one unit averagely.

Table 1 IEPC of 30 provinces in China, 2015
Although the rest of the explanatory variables cannot influence the IEPC, they can explain the differences between provinces to some extent, including GDP per capita, age-standardized mortality for cancer, proportion for inpatient outside of home province and ratio of population aged 15–64 years old. The final model can explain 50.65% of the variation, and the independent variables explained the model well (13).
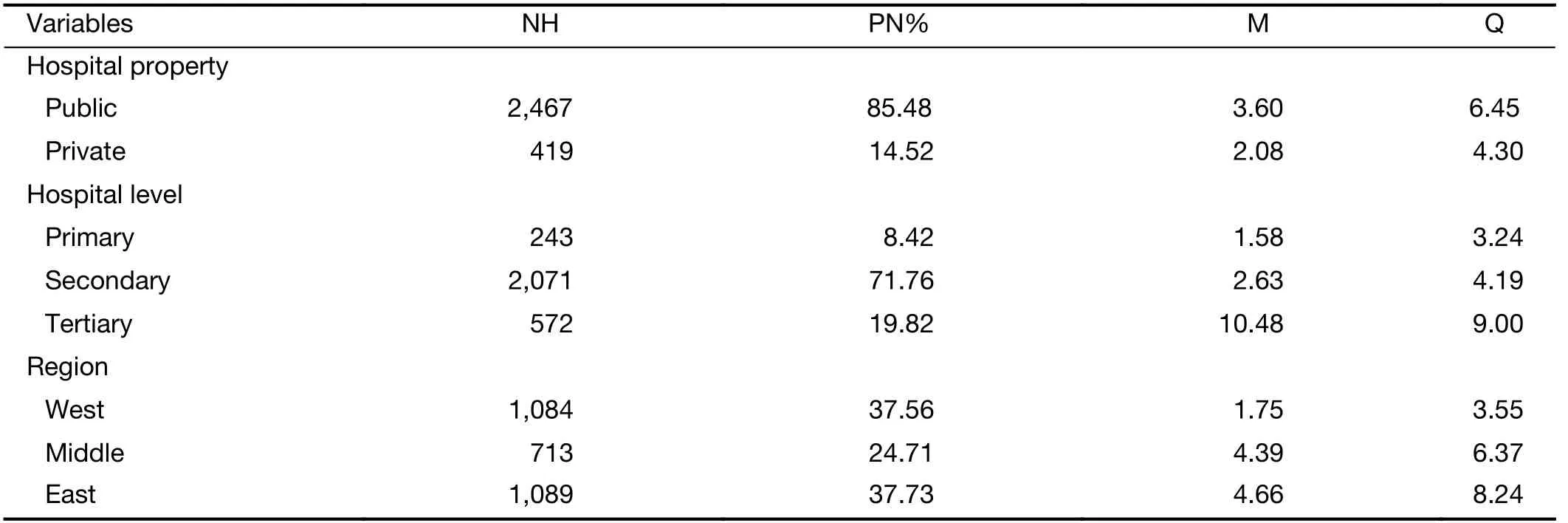
Table 2 IEPC in different classification in China, 2015
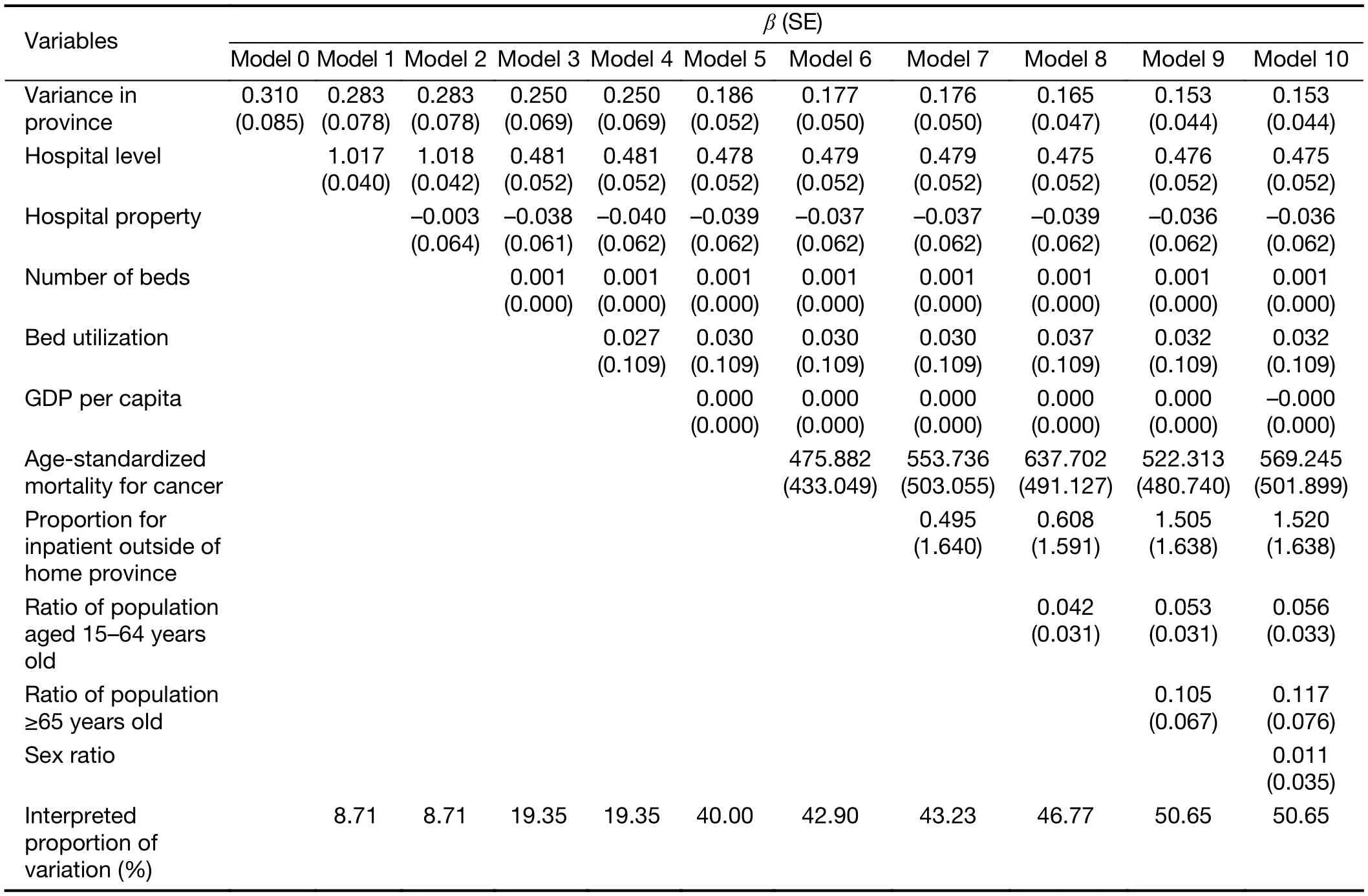
Table 3 Two-level linear regression model on influencing factors of IEPC
To our knowledge, this is the first study exploring the IEPC using national authoritative data to acquire the proportion of cancer in various diseases in China. We estimated the proportion and identified the influencing factors of it by multilevel model.
Limitations should be noted in interpreting the results ofour study. Firstly, some influencing factors (such as the price of cancer treatment) on IEPC could not be included in the model due to the limitation of data accessibility. Secondly, the variation of data completeness among different levels of hospitals and different regions may influence our final model. However, this is still the inpatient expenditure pattern study with the largest data sample.
Our study showed that a considerable proportion of IEPC variation could be explained by the differences of hospital level and number of beds. It implied that it is possible to estimate disease-specific ratio of inpatient expense taking account of key influencing factors in China. Furthermore, this study is an input to economic and financial analyses and provides evidence for future study on the national economic burden of cancer. What’s more, the influencing factors obtained from this study can predict the ratio in the area where data are not available.
Acknowledgements
This work was supported by National Natural Science Foundation of China (No. 71403189).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
1.Chen W, Zheng R, Zuo T, et al. National cancer incidence and mortality in China, 2012. Chin J Cancer Res 2016;28:1-11.
2.He J, Chen W. Chinese cancer registration report, 2012. Beijing: Military Medical Science Press, 2012.
3.Xu C, Cai P, Zhang Y, et al. Results and analysis of expenditure on prevention and treatment for malignant tumor in China in 2010. Zhongguo Wei Sheng Jing Ji (in Chinese) 2014;33:24-6.
4.China Health and Family Planning Statistical Yearbook, 2016. Beijing: China Union Medical College Press, 2016.
5.Zhou L, Guan P, Sun LP, et al. Health economic assessment for screening of gastric cancer in a high risk population in northeastern China. Chin J Cancer Res 2011;23:21-4.
6.Gelband H, Sankaranarayanan R, Gauvreau C, et al. Costs, affordability, and feasibility of an essential package of cancer control interventions in low-income and middle-income countries: key messages from Disease Control Priorities, 3rd edition. Lancet 2016;387:2133-44.
7.Keating NL, Landrum MB, Huskamp HA, et al. Dartmouth atlas area-level estimates of end-of-life expenditures: How well do they reflect expenditures for prospectively identified advanced lung cancer patients? Health Serv Res 2016;51:1584-94.
8.Hirth RA, Chernew ME, Miller E, et al. Willingness to pay for a quality-adjusted life year: in search of a standard. Med Decis Making 2000;20:332-42.
9.Adam T, Evans DB. Determinants of variation in the cost of inpatient stays versus outpatient visits in hospitals: a multi-country analysis. Soc Sci Med 2006;63:1700-10.
10.Goldstein H, Rasbash J, Yang M, et al. A multilevel analysis of school examination results. Oxf Rev Educ 1993;19:425-33.
11.Adam T, Evans DB, Ying B, et al. Variability in costs across hospital wards. A study of Chinese hospitals. PLoS One 2014;9:e97874.
12.GBD 2015 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016;388:1603-58.
13.Ning M, Zhang Q, Yang M. Comparison of selfreported and biomedical data on hypertension and diabetes: findings from the China Health and Retirement Longitudinal Study (CHARLS). BMJ Open 2016;6:e009836.
Cite this article as: Lan L, Cai Y, Zhang T, Wu R, Xue M, Meng Q. Influencing factors of inpatient expenditure pattern for cancer in China, 2015. Chin J Cancer Res 2017;29(1):11-17. doi: 10.21147/j.issn.1000-9604.2017.01.02
10.21147/j.issn.1000-9604.2017.01.02
*These authors contributed equally to this work.
Ming Xue. Center for Health Statistics and Information, National Health and Family Planning Commission, Beijing 100032, China. Email: xueming@nhfpc.gov.cn; Qun Meng. West China School of Public Health, Sichuan University, Chengdu 610041, China; Center for Health Statistics and Information, National Health and Family Planning Commission, Beijing 100032, China. Email: mengqun@nhfpc.gov.cn.
Methods:Two-level lineal regression model was used to explore influencing factors of ratios of the cancer inpatient expenditure over the total inpatient expenditure of hospitals in China in 2015. A total of 40.76 million inpatient medical records were used to generate the outcome variables, while the explanatory variables were from hospital information database and China Health and Family Planning Statistical Yearbook and literatures.
Results:Inpatient expenditure pattern for cancer (IEPC) varied largely across provinces, ranging from 3.03% to 19.61%. The major sources of variability were from the differences of hospital level and number of beds. There was homogeneity within a province, while heterogeneity between the provinces. Rising one level of the hospital led to the increase of 0.475 natural logarithm units of IEPC averagely. The number of beds increasing 1,000 each made the natural logarithm of IEPC increase one unit averagely.
Conclusions:Our study showed that a considerable proportion of IEPC variation could be explained by the differences of hospital level and number of beds. It implied that it is possible to estimate disease-specific ratio of inpatient expense taking into account key influencing factors in China. Furthermore, this study is an input to economic and financial analyses and provides evidence for future study on the national economic burden of cancer.
Submitted Dec 12, 2016. Accepted for publication Feb 10, 2017.
 Chinese Journal of Cancer Research2017年1期
Chinese Journal of Cancer Research2017年1期
- Chinese Journal of Cancer Research的其它文章
- Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy in treatment of gastric cancer with peritoneal carcinomatosis
- PEG-asparaginase in BFM-90 regimen improves outcomes in adults with newly diagnosed lymphoblastic lymphoma
- Extranodal involvement in young patients with diffuse large B-cell lymphoma: distribution, prognostic value and treatment options
- Upregulation of kazrin F by miR-186 suppresses apoptosis but promotes epithelial-mesenchymal transition to contribute to malignancy in human cervical cancer cells
- Prognostic factors for transarterial chemoembolization combined with sustained oxaliplatin-based hepatic arterial infusion chemotherapy of colorectal cancer liver metastasis
- Clinical characteristics and response to tyrosine kinase inhibitors of patients with non-small cell lung cancer harboring uncommon epidermal growth factor receptor mutations
