Efficacy and safety of a digital navigation template combined with cervical pedicle screw implantation: study protocol for a prospective, single-center, self-controlled, clinical trial
Wei Wei, Long-yan Xing, Jia-xun Jiao, Lei Zhao, Ai-qing Lu *
1 Department of Orthopedic Disease, Harrison International Peace Hospital, Hengshui, Hebei Province, China
2 Department of Nuclear Magnetic Resonance, Harrison International Peace Hospital, Hengshui, Hebei Province, China
3 Department of Orthopedics and Traumatology, Zhangjiagang Hospital Affiliated to Nanjing University of Chinese Medicine,Zhangjiagang, Jiangsu Province, China
IntroductIon
Background
Cervical pedicle screw fixation is a surgical procedure often used by surgeons in the department of orthopedics; it is a reliable method for the treatment of traumatic and nontraumatic cervical instability and the removal and fixation of a cervical disc.1,2Cervical pedicle screw fixation is popularized and applied by clinicians because of its biomechanical advantages. However, the cervical vertebrae are irregular bones with a complex anatomical structure. The spinal cord passes through the middle of the cervical vertebrae.The vertebral body is adjacent to the vertebral artery, and the nerve root passes through the upper and lower vertebral bodies. Screw implantation on the vertebral body carries a high surgical risk.3,4The high cervical vertebral variability and complex internal three-dimensional (3D) space further adds to the risk of the operation. Clinically, such operations often require the senior physician to manually insert the screws. According to the anatomical landmarks, the entry point is fixed and then the direction and depth of the screw are determined according to the surgeon’s own experience. The location of the screw path should be repeatedly determined by X-ray or computed tomography (CT) during the operation; however, the failure rate of bare-hand screw insertion is still high. Repeated X-ray and CT detection prolongs the operation time, increases intraoperative blood loss, and increases the risk of surgery.5
With the rapid development of science and technology,digital technology has found application in various fields of medicine; surgery is moving toward individuation,precision, and minimal invasion.6-8Digital orthopedics has become a new field of modern medicine.6-8Computeraided image navigation can achieve minimal invasion and intelligent orthopedic surgery.9-11Compared with bare-hand screw insertion, the digital navigation template has the advantages of high accuracy and small error in the screw insertion depth.9-11
Main objective
The objective of this study is to determine the clinical eff icacy and safety of the digital navigation template combined with cervical pedicle screw implantation.
Methods/desIgn
Study design
This prospective, single-center, self-controlled, clinical trial will analyze the data of 32 patients with cervical spondylosis at the Harrison International Peace Hospital in China.Before surgery, a 3D navigation model of the cervical vertebrae will be designedvia3D reconstruction, and 3D printing will be used to generate the navigation template.The cervical pedicle screws will be implanted according to preoperatively designed models. The patients will be followed up for 40 months. The screw position observed after implantation will be rated as excellent and good. Changes in pain and neurological function will be measured before and after implantation. This open-label trial does not set a control group or use the blind method for group assignment.Figure 1exhibits the flow chart of the study protocol.
Strengths and limitations
• The digital pedicle navigation template designed based on 3D printing improves the accuracy of screw implantation
• No control group
• Small sample size
Study setting
Harrison International Peace Hospital in China.
Recruitment
We will recruit 32 patients with cervical spondylosis, who are hospitalized in the Harrison International Peace Hospital, Hebei Province, China, from December 2017 to April 2019. We will dispatch the study plan leaflets to inpatients.Patients and their family members will voluntarily decide whether to participate in the study after reading the leaflet.After screening according to the inclusion criteria described below and providing informed consent, the data from these patients will be collected for our study.
Study population
Thirty-two patients with cervical spondylosis will be recruited from the Harrison International Peace Hospital,Hebei Province, China, including 21 men and 11 women,with a mean age of 41.0 ± 10.8 (23–56) years. The site of injury will include the atlanto-axial joint in 3 cases and other cervical segments in 29 cases. The fixation method will include two-stage fixation in 13 cases, three-stage fixation in 12 cases, four-stage fixation in 6 cases, and more than four-stage fixation in 1 case. All patients will be subjected to a digital navigation template combined with cervical pedicle screw implantation.
Inclusion criteria
Patients fulfilling all of the following criteria will be considered for study inclusion:
• In accordance with the diagnostic criteria of the Third National Symposium on cervical spondylosis,5patients with arm numbness and pain; a consistent range with the innervation of cervical spinal nerves; and positive brachial plexus traction test or foraminal compression test results
• Those with complete X-ray, CT, and MRI data
• Those who have successfully completed the imaging examination and have answered all relevant questionnaires
• Those under continuous treatment in the outpatient ward of our hospital
• Those who provide signed informed consent
Exclusion criteria
Patients fulfilling one or more of the following conditions will be excluded from the study:
• Previous surgery
• Cognitive disorder
• Do not agree to participate in this study
Withdrawal criteria
Patients who meet one or more of the following criteria during the trial will be withdrawn from the study:
• The researchers believe them to be no longer suitable for continuing clinical validation
• Cannot complete the follow-up
Expected duration and reason
Considering the number of cervical spondylosis patients,the recruitment and follow-up will be completed in 4 years.
Interventions
Preoperative digital 3D measurement and design
Thirty-two patients will undergo cervical 64-multidetectorrow spiral CT (Siemens, Erlangen, Germany). Scanning parameters will be as follows: thickness 1.0 mm, current 310 mAs, and voltage 120 kV. Original data will be exported in standard DICOM format and loaded into Mimics 15.0 software for 3D model reconstruction. After showing the horizontal, coronal, and sagittal planes of the cervical spine,the Region Growing will be performed to create a set of Mask pixels. Editmasks will be conducted layer by layer to delete the other parts with the same gray matter and to complement the pixel.3The Calculate 3D in Segmentation menu will be carried out to form the simulated shape and to calculate the 3D fracture model. The 3D model of the cervical vertebrae will be produced using the Unite Boolean calculation. Subsequently, the entity model and navigation template will be created by 3D printing (Figure 2). The anatomical morphology of the posterior vertebral lamina and spinous process root of each vertebral body will be measured, and a screw insertion channel will be designed. The 3D distance will be measured using Mimics 13.0 software to identify the screw insertion depth. The reverse template of the above vertebral body and the screw insertion direction will be designed to form a unilateral navigation template,which will be created by 3D printing.
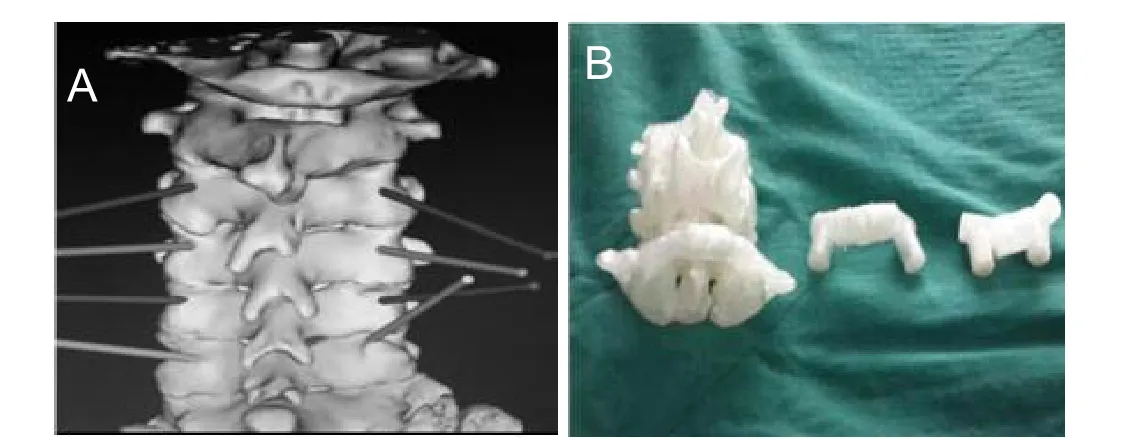
Figure 2:Three-dimensional (3D) reconstruction of the cervical vertebrae and the navigation template.
Application of individualized navigation template
The preoperative plan will be established according to the model of the cervical vertebrae and navigation template. The cervical spine and vertebral plate will be exposed through the posterior and the preoperatively printed navigation template will be attached to the vertebral body. A hole will be drilled with a 2.0 mm drill in the designed direction.After reaching the appropriate depth, the probe will be used to confirm that the screw will not pierce the bone. After screwing in the appropriate screws, C-arm fluoroscopy will be utilized to identify the screw placement in the anteroposterior and lateral positions (Figure 3).
Efficacy evaluation
Primary outcome measure
At 40 months after implantation, X-ray and CT in the anteroposterior and lateral positions will be conducted to assess the screw position. The screw position will be categorized into four grades. Grade 1: the screws are completely in the vertebral cancellous bone. Grade 2: the screws break through the vertebral cortical bone, within 1 mm. Grade 3: the screws break through the vertebral cortical bone,between 1 and 2 mm. Grade 4: the screws break through the vertebral cortical bone, more than 2 mm. The excellent/good rate is equal to the number of patients at grades 1 and 2/the total number of patients × 100%.
Secondary outcome measures
• The Visual Analog Scale score, which ranges from 0 to 10, will be assessed before implantation and 40 months after implantation. A higher score indicates more severe neck pain.12
• The American Spinal Injury Association classification will be assessed before implantation and 40 months after implantation. Grade A: Complete lesion; no sensory or motor function is preserved in the cervical region. Grade B: Incomplete lesion; sensory but no motor function is preserved below the neurological level. Grade C: Incomplete lesion; motor function is preserved below the neurological level and more than half of the key muscles below the neurological level have a muscle grade less than 3. Grade D: Incomplete lesion; motor function is preserved below the neurological level and at least half of the key muscles below the neurological level have a muscle grade of 3 or more. Grade E: Motor and sensory functions are normal.13• Cervical X-ray and CT scans will be performed before implantation and 40 months after implantation to observe the location of screw insertion and the recovery of the injured cervical vertebra.
• Incidence of adverse reactions will be used to assess the safety of implantation 40 months after implantation. The incidence of adverse reactions is equal to the number of patients with adverse reactions/the total number of patients× 100%.
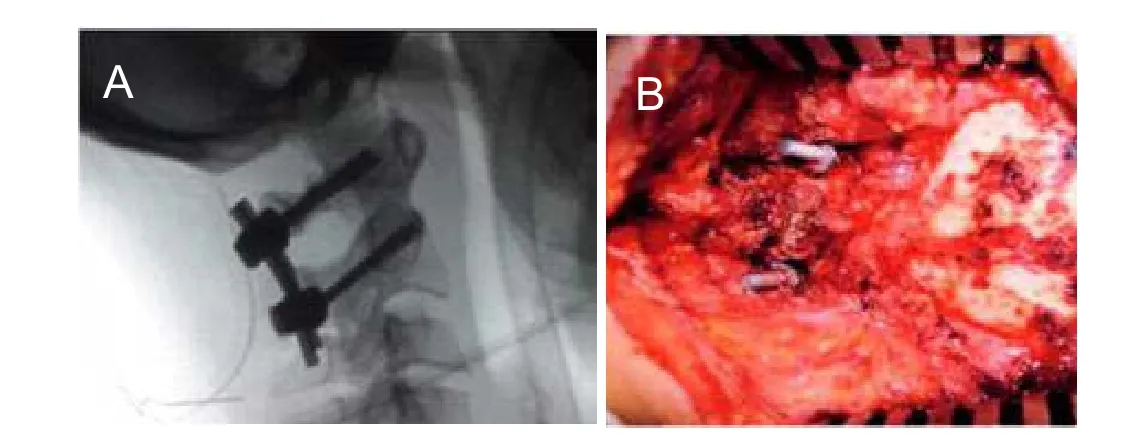
Figure 3: Intraoperative application of the navigation template.
Safety evaluation
Adverse reactions, including the screw falling off, loosening, dizziness, headache, numbness, and infection, will be directly recorded, and the possible causes will be analyzed.Adverse events, adverse reactions, reasons, and explanations will be listed.
Monitoring plan
Early stage of the trial
The protocols have been approved by the Ethics Committee of the Harrison International Peace Hospital in China. We will sign the trial agreement with the hospital. Researchers must be familiar with clinical orthopedic procedures and protocols.
Middle stage of the trial
Regular monitoring ensures that the enrolled patients will comply with the inclusion and exclusion criteria. All operations will be in strict accordance with the scheme to ensure data integrity.
Late stage of the trial
After the patient completes all examinations, a trial visit will be required to prevent the omission of test records.
Statistical considerations
Statistical design, methods, and analysis rules
All data will be analyzed using SPSS 13.0 software (SPSS,Chicago, IL, USA), according to the intention-to-treat principle. Normally distributed measurement data will be expressed as the means ± standard deviation. Non-normally distributed measurement data will be expressed as the lower quartile (q1) and median and upper quartiles (q3). Count data will be presented as percentages.
The Visual Analog Scale scores before implantation and 40 months after implantation will be analyzed with a pairedsamplest-test. The American Spinal Injury Association classification results will be analyzed using the McNemar's test. The significance level will beα= 0.05.
Expected loss rate
We will assume a patient loss rate of less than 20%.
Data missing processing
In the case of missing data, the patient will be excluded from the study and subsequently replaced with a new case.
Baseline analysis
The patients’ baseline information, including demographic data, general disease history, and clinical data, are shown inTable 1.
Data management
Case report forms of all cases will be completed by clinical researchers and reviewed by the auditors. After data entry,the case report forms will not be altered, and the database will be locked by a data manager. The locked database or file will not be changed.
Quality control
During the clinical trial, the sponsor will regularly send inspectors to the research center for monitoring visits to ensure that all contents of the research program will be strictly abided to. The original data will be checked to ensure that the case report form will be true, complete,and correct.
Ethical requirements and informed consent
The study protocol will be conducted in accordance with theDeclaration of Helsinki. The writing and editing of the article will be performed in accordance with the Standard Protocol Items: Recommendations for Interventional Trials(SPIRIT) (Additional file 1). The investigator has the responsibility of providing the ethics committee with clinical trial protocols, informed consent forms, and information provided to the subjects, in order to obtain independent approval documents for implementing the clinical trial. The research will be carried out after the approval of the ethics committee. The protocols have been approved by the Ethics Committee of the Harrison International Peace Hospital in China (approval number: 20120630).
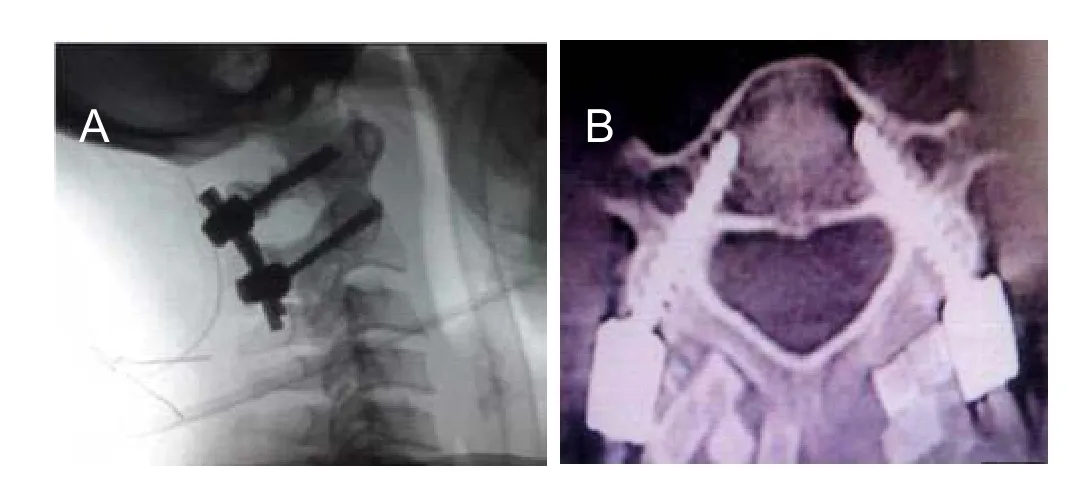
Figure 4:Shape of pedicle screws 40 months after implantation.
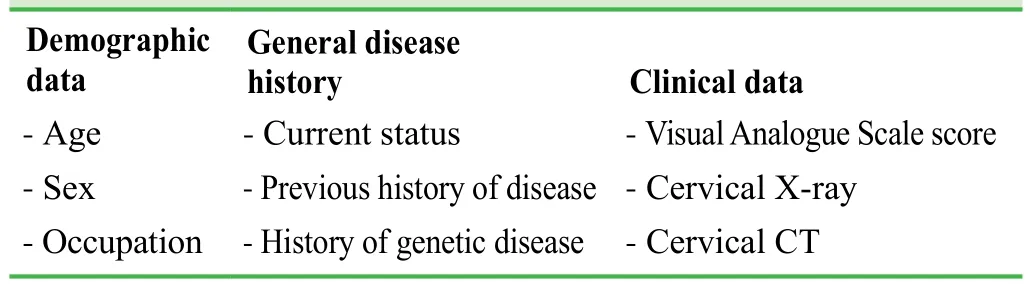
Table 1: Baseline data and general disease history of the included patients
results
Trial status
The results of preliminary experiment from 2012 to 2016 have been obtained as follows.
Follow-up results
The surgery was successful in all 32 patients. During the cervical pedicle screw fixation, 182 screws were implanted.The screw insertion depth, position, and direction were consistent with the preoperative design. X-ray and CT images showed that 167 screws (92%) were in grade 1 (Figure 4),15 screws (8%; 6 screws penetrated the medial cortex of the pedicle of the vertebral arch, and 9 screws penetrated the lateral cortex of the pedicle of the vertebral arch) in grade 2, and no screws were in grades 3 or 4.
Adverse reactions
All cases were followed up for 14–40 months. No injuries to the nerve root, vertebral artery, or spinal cord induced by screws were found. No severe complications appeared,such as screw loosening, slipping, or breaking.
DIscussIon
Significance of this study
A 3D navigation model of the cervical vertebrae will be designed based on the CT scans. Using this model, we will observe the patient's cervical vertebrae in all aspects,viamultiple angles and levels, before the operation, so as to fully understand and discuss the cervical morphology and surgical plan.14-17The entry channel will be designed and the screw insertion depth will be determined according to the anatomical morphology of the posterior vertebral lamina and spinous process root of each vertebral body. The reverse template will be designed to form a unilateral navigation template, which will be created by 3D printing. This will truly achieve an individualized surgical scheme to enable the optimal surgical design. This method not only reduces the operation time, intraoperative bleeding, surgical injury,and risk of surgery and improves the success rate of the operation, but also avoids the injury caused to the patient and the medical staff by multiple fluoroscopies during the operation.18Compared with bare-hand screw implantation,the application of a digital navigation template has the following advantages: (1) high accuracy of screw insertion and depth of insertion as the screw was inserted according to the preoperative navigation template. (2) The designed navigation template is a single-stage vertebral navigation system that is different from a computer-aided navigation system and has no requirement for a change in the position of the patient during the operation. The individualized design is not restricted by vertebral variation and spinous process hyperplasia. (3) The navigation template is small,convenient to disinfect, and does not use large instruments.The operation process is simple and can be mastered only by simple training, which can be easily accepted by clinicians.(4) Compared with the traditional surgery, this method does not need repeated fluoroscopy; fluoroscopy is only required after screwing, which shortens the operation time and avoids potential injury to medical staff. (5) The navigation template uses biodegradable plastics and the cost is low; therefore, it will not increase the patient’s economic burden.
Limitations of this study
This trial has some limitations. (1) The preoperative design is complicated, and required knowledge of computer technology. (2) Each patient has an individualized template, so the time from design to implementation is long. Therefore,it is not suitable for emergency surgery. (3) Because the navigation template is small, a tight attachment cannot be easily achieved intraoperatively, resulting in deviation of the screw channel. (4) The sample size is small and the trial does not have a control group. The above factors can affect the accuracy of the results, and the future research will be further improved.
Evidence for contribution to future studies
Whether the navigation template can attach to the bone structure is the key to the success or failure of the operation.A small gap between the navigation template and the cervical vertebrae can lead to a great deviation in the direction of the screw placement. Therefore, the soft tissue of the spinous process, vertebral lamina, and lateral mass should be stripped away as much as possible to allow the template to tightly adhere to the osseous structure. The screw placement at grade 2 in 15 cases is possibly a result of this.Furthermore, the navigation template may also have some errors during production,19which is related to the accuracy of the 3D printer. A previous study has reported that the error during template production by the 3D printer is 0–1 mm.20A slight error may cause surgery failure. We believe that the preoperative application of navigation templates in the 3D reconstruction of vertebral injuries can reduce the serious consequences of secondary errors. Moreover, after drilling, probe exploration of the walls of the bone channel can effectively prevent the screws from drilling out of the cortical bone, which is verified by plain radiography at the end of the surgery.
Author contributions
Study conception and design, manuscript writing, and critical revision of the manuscript: WW. Constructive suggestions during experiment design: AQL. Contributing to the completion of study: LYX, JXJ and LZ. All authors approved the final version of the paper.
Conflicts of interest
None declared.
Research ethics
The protocols have been approved by the Ethics Committee of the Harrison International Peace Hospital in China (approval number:20120630). The study follows international and national regulations in accordance with theDeclaration of Helsinkiand relevant ethical principles.
Declaration of patient consent
The authors certify that they will ob tain all appropriate patient consent forms. In the form the patients will give their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Data sharing statement
Datasets analyzed during the current study are available from the corresponding author on reasonable request.
Plagiarism check
Checked twice by iThenticate.
Peer review
Externally peer reviewed.
Open access statement
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under identical terms.
Additional file
Additional file 1: SPIRIT checklist.
1. Yin QS, Xia H, Wu ZH. Transoral Atlantoaxial Reduction and Internal Fixation. Beijing: People's Medical Publishing House. 2010.
2. Rodt T, Schlesinger A, Schramm A, et al. 3D visualization and simu lation of frontoorbital advancement in metopic synostosis.Childs Nerv Syst.2012;23:1313-1317.
3. Zhang M, Wang WL, Wang YQ, et al. Anatomy study and design of the collimator for anterior cannulated odontoid screw.Zhonghua Shiya Waike Zazhi. 2014;31:1141-1143.
4. Wang Y. Department of orthopedics: precise medical applica tion and thinking. Zhonghua Yixie Zazhi. 2015;9:2512-2514.
5. Li ZC, Chen DY, Wu DS, et al. Summary of the Third National Symposium on Cervical Spondylosis.Zhonghua Waike Zazhi.2008;46:1796-1799.
6. Zhuang HM, Guo YY, Lin YB, et al. Clinical analysis on cervi cal anterior compression screw for odontoid fracture.Zhonghua Quanke Yixue. 2012;10:1063-1065.
7. Digioia AM. What is computer assisted orthopaedic surgery?Clin Orthop. 2013;354:2-4.
8. Hao DJ, He BR, Xu ZW, et al. Clinical significance of measurements and classification of atlas pedicles by three-dimensional computertomography and reconstruction.Zhongguo Jizhu Jisui Zazhi. 2012,22:142-146.
9. Duan LQ, Zhang WZ, Shang XF, et al. Anterior fixation for type odontoid fractures with compressive cannulated screw.Linchuang Guke Zazhi.2011;14:244-246.
10. Attias N. Lindsey RW. Starr AJ, et al. The use of a virtual threedimensional model to evaluate the intraosseous space available for percutaneous screw fixation of acetabular fractures.J Bone Joint Surg Br. 2011;87:1520-1523.
11. Yoshiharu K, Masato N, Taketoshi Y, et al. Development of a new technique for pedicle screw and Magerl screw insertion using a 3-dimensional image guide.Spine. 2012;37:1983-1988.
12. Knop C, Oeser M, Bastian L, et al. Development and validation of the Visual Analogue Scale (VAS) Spine Score.Unfallchirurg.2011;104:488-497.
13. Frankel HL, Hancock DO, Hyslop G, et al. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. I.Paraplegia. 1969;7:179-192.
14. He HW, Sui T, Zhao HY, et al. Three dimensional CT study on relevant parameters of atlas pedicle screw insertion.Zhongguo Zuzhi Gongcheng Yanjiu. 2012;16:1526-1529.
15. Mouhsine E, Garofalo R, Borens O, et al. Acute total hip arthroplasty for acetabular fractures in the elderly: 11 patients followed for 2 years.Acta Orthop Scand. 2012;73:615-618.
16. Yin H, Zhao BY. A comparative study on pedicle screw internal fixation to the lower cervical vertebra by three screw place methods.Zhongguo Zuzhi Gongcheng Yanjiu. 2011;15:4040-4044.
17. Stockle U, Konig B, Dahne M, et al. Computer assisted pelvic and acetabular surgery. Clinical experiences and indications.Unfallchirurg. 2013;105:886 -892.
18. Gay SB, Sistrom C, Wang GJ, et al? Percutaneous srew fixation of acetabular fracture with CT guidancerrpreliminary results of a new teachnique.AJR Am J Roentgenol. 2012;158:819.
19. Zhu XT, Wang YP, Xu J. Three dimensional CT construction of atlas ponticulus and pedicle screw insertion.Zhonggu Gu yu Guanjie Waike. 2014;7:451-455.
20. Haidudewych GJ, Scaduto J, Herscovici D Jr. lartogenic nerve injury in acetabular fracture surgery: a comparison of monitored and unmonitored procedures.J Orthop Trauma. 2012;16:297-301.
 Clinical Trials in Orthopedic Disorder2017年4期
Clinical Trials in Orthopedic Disorder2017年4期
- Clinical Trials in Orthopedic Disorder的其它文章
- Exercises interventions in people with rheumatoid arthritis
- Use of incisional negative pressure wound therapy in orthopedics
- Preemptive analgesia in orthopedic surgery: a literature review
- Surgical site infections in orthopedic surgery: incidence and risk factors at an Iranian teaching hospital
- Predicting necrotic femoral head collapse using computed tomographic and X-ray imaging before hip arthroplasty: study protocol and results of a single-center, open-label,diagnostic trial
