Surgical site infections in orthopedic surgery: incidence and risk factors at an Iranian teaching hospital
Keykhosro Mardanpour, Mahtab Rahbar, Sourena Mardanpour, Nyousha Mardanpour
1 Kermanshah University of Medical Sciences, Kermanshah, Iran
2 Iran University of Medical Sciences, Tehran, Iran
3 Azad University of Medical Sciences, Tehran, Iran
IntroductIon
A surgical site infection is an infection within 30 days if no implant is left in place, or within 12 months of surgery if an implant is left in place after the operation that occurs in the part of the body where the surgery took place. Superficial surgical site infections can involve the skin and subcutaneous only. Deep surgical site infections are more serious and can involve tissues under the skin, organs,or implanted material. Infection is confirmed by at least one of the following: Purulent drainage with or without laboratory confirmation, from the superficial incision or organisms isolated from an aseptically obtained culture of fluid or tissue from the superficial incision. Also, at least one of the following signs or symptoms of infection: pain or tenderness, localized swelling, redness, or heat should be existed. Diagnosis of surgical site infection (SSI) made by a surgeon or an attending physician.1
Surgical Site infections are a common cause of nosocomial infection, accounting for 38 percent of nosocomial infections. Overall risk of SSI is 2–5% percent of the more than 30 million patients undergoing surgical procedures each year.2SSIs are associated with substantial morbidity and mortality, prolonged hospital stay, and increased patient cost.3-6Patients with SSI also utilized more healthcare resources, including outpatient and emergency department visits, radiology, and home health aides. They were also readmitted more frequently. In Iran, the surgical site infection comprises between 17.4% compared with the 14% quoted in literature. In our study SSI is identified by CDC criteria.1Several factors are to be taken into account for SSI. In large study involving 16,291 patients undergoing orthopedic surgery, SSI rate was 2.23% and indicated that advanced age,length of preoperative hospitalization, duration of surgery were main risk factors.7Another research on 1,073 patients indicated 58.7% patients developed postoperative surgical site infection. The main factors associated with complications were age over 40 years, duration of surgery greater than 90 minutes, use of mechanical suture and delay for ambulation.8In a literature review, the authors indicated that the main risk factors for the occurrence of infection in orthopedic surgery are: advanced age, smoking, high BMI,immune impairment and chronic disease.9In orthopedic patients, the surgical site infection prolongs hospital stay on average for two weeks, doubles re-hospitalization rates,and costs can increase by over 300%. In addition, patients may have physical limitations and significant reductions in quality of life.10The aim of this study was to analyze the occurrence and risk factors for surgical site infection in patients undergoing orthopedic surgery.
Methods/desIgn
This study was performed at the Department of Orthopedic Surgery and trauma center in two teaching hospitals of Kermanshah Medical University in Iran. These teaching hospitals have a catchment population of approximately 3 million people in the west of Iran and serves as a reference centers for orthopedy and trauma management. This prospective cohort study was conducted from January 2012 to January 2015. At the time of surgery, each procedure was classi fied by the attending surgeon according to the degree of intrinsic microbial contamination of a surgical site modified by Centers for Disease Control and Prevention (CDC)for use in surgical site infection surveillance (Table 1).
The CDC standardized surveillance criteria for de fining surgical site infections, which involve interpretation of clinical and laboratory findings, were used to detect nosocomial infections. All surgery patients during this period were interviewed and daily observed during their hospitalization by an internal clinician from the surgical team, together with an infection control nurse. When patient faced to clinical suspicion of wound infection (pain or tenderness, localized swelling, redness or heat), a sample was taken of surgical site and transported to the microbiology laboratory for culture. Also, post discharge patients who reported any of the symptoms of wound infection by telephone were asked to return to the hospital for reexamination. Observation of the operating theater during the study found satisfactory sterile techniques, such as surgical hand preparation, sterile gloves, and surgical draps, but there was limited ventilation. Products for cleaning and disinfection of surfaces and equipment were mostly available. There was a lack of hand rub alcohol dispensers and single rooms for isolation of patients colonized or infected with resistant microorganisms.If necessary, cohort isolation was performed, for example,patients colonized/infected with the same organism were grouped together. However, diagnosis of the surgical site infection was made based on positive microbial culture in concordance with the primary surgical team, which also performed the internal control of all clinical data.
In this study, 1,900 patients in two teaching hospitals underwent orthopedic surgery between January 2012 and January 2015. They were studied for SSI and the factors affecting it. Initially, 1,947 patients were recruited for the study but 47 were excluded of the study because of deficient medical records and accompanying conditions such as diabetes, high arterial blood pressure, kidney or liver failure,malignancy, febrile condition, cardiac disorders, thyroid disorders, blood disease, chronic obstructive pulmonary disease, convulsion, hyperlipidemia, immunological disorders, or had previously undergone surgical operations,multiple trauma. The dependent variable in this study
Strengths and limitations
• This study is the first to report orthopedic surgical site infections in two teaching hospitals in the west of Iran.
• The merit of the study is that it confirmed that active surveillance of surgical site infections might be organized in countries with limited resources.
• Surgical site infections are a considerable problem in orthopedic wards in Iran but incidence rates being lower than those in other developmental countries.was orthopedic surgical site infection. The independent variables were age, sex, body mass index, smoking, administration of prophylactic antibiotics, multiple fractures,type of fracture and operation, duration of operation and hospitalization and even postoperative care. CDC guidance based on a commissioned systematic review concludes that perioperative antimicrobial prophylaxis is one of the most effective measures for the prevention of SSIs.1In this study,3rdgeneration cephalosporins were used for arthroplasty,hand transplantation and 2ndgeneration cephalosporin were used for operation with fixation, operation without fixation such as tendon repair and peripheral nerve microsurgery.The methods used to detect post-discharge SSI were direct observation of the wound by health professional (n= 1,679)and telephone interviews with patients (n= 121). In all patients who had two or more organisms, Staph epidermidis was the common organism. The following prophylactic antibiotics were used: ampicillin, gentamicin, cefoxitin,metronidazole and ceftriaxone. The first line antibiotic that we used for prophylaxis was 2ndgeneration cephalosporin followed by 3rdgeneration cephalosporin, with the trend to use 3rdgeneration cephalosporins in patients undergoing arthroplasty and hand transplantation. However, there was sufficient evidence to suggest that particular generation of cephalosporin is more effective in reduce to SSI.
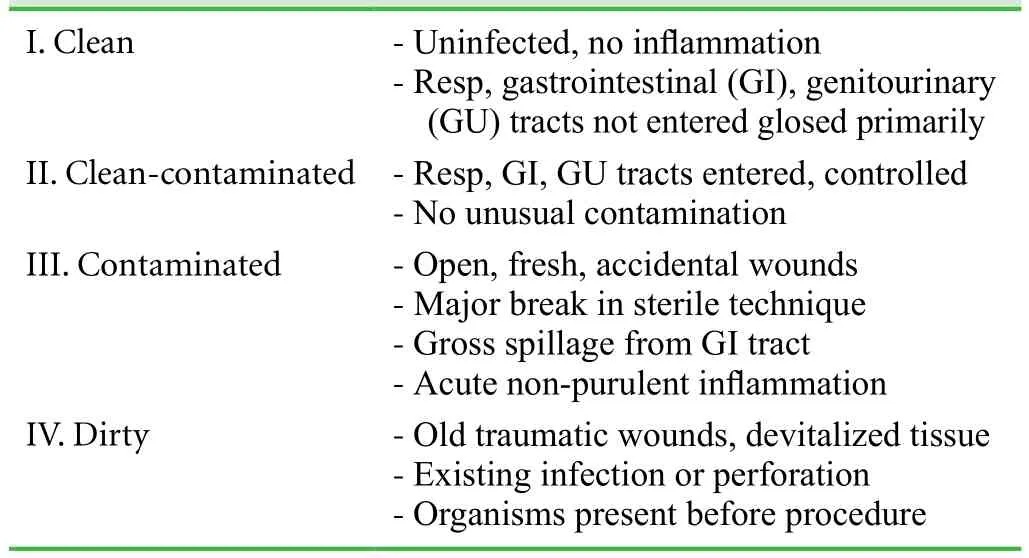
Table 1: Surgical wound classification
In this study, before discharge, all patients were noted for possible signs and symptoms of SSIs. Appropriate informed consent and demographic data obtained for filling 22-item questionnaire and cooperation for serial visits after surgery(Additional Table 1).
Statistical analysis
The collected data were analyzed by the SPSS 16 software package (SPSS, Chicage, IL USA). Differences between groups were tested by use of Student′st-test, Fisher′s exact test, or Wilcoxon rank sum test, as appropriate.P< 0.05 was considered to be statistically significant.
results
A total of 73 of 1,900 patients who had orthopedic operations contracted an SSI. The incidence of SSI was 3.84%.There were 1,329 males and 571 females (male to female ratio: 2.3/1) with an average age of 42.32 ± 17.71 years.All patients set in three age groups as follow; less than 25,between 25 to 50 and more than 50 years old. Distribution of patients based on the type of operation and SSI Incidence have been mentioned inTable 2.
Of the 1,900 patients who had undergone orthopedic surgery 73 (3.84%) suffered from SSI as defined inTable 2.Clean wound (class I) was in 7 cases (2.3%), clean-contaminated wounds (class II) in 15 cases (3%), contaminated wounds (class III) in 44 cases (3.8%) and dirty infected wounds (class IV) in 7 cases (4.8%) (P< 0.04). The body mass index (BMI) for 469 patients (24.7%) was equal and above 25. About 33 (7%) of those suffered from SSI after surgery (P< 0.01). The distribution of SSI on the basis of the following independent variables; age, sex, body mass index, smoking, emergency operation ,administration of prophylactic antibiotics, multiple fractures, type of fracture and operation, duration of operation and hospitalization and type of wounds has been mentioned inTable 3. To the best of our ability, this study presented correlations between SSI incidence with advance age, male sex, high BMI, smoking,emergency operation, type of prophylactic antibiotic administered before operation and comminuted fracture with using fixation device were all significant atP< 0.00 to 0.05 (Table 3). Also heavy and large operations such as multiple fracture,artheroplasty or transplantation are time-consuming and lead to prolong duration of operation and hospitalization which threaten the patient for SSI.
The distribution of infective organisms in our population presented inTable 4.
The most common isolated infective organism wasStaphylococcus speciesincluding Methicillin ResistantStaphylococcus aurous(MRSA) in 32 patients (43.8%),Staph epidermidisin 17 (23.2%),Acinetobacter speciesin 11 (15.0%),Pseudomonas speciesin 7 (9.6%),Enterococcus speciesin 3 (4.1%),Escherichia coliin 2 (2.7%)andKlebsiellaspeciesin 1 (1.4%). There were 53 patients(72.6%) infected by a single organism, 16 (21.9%) by two infecting organisms, and 4 (5.5%) patients infected by more than two organisms. In all patients who had two or moreorganisms,Staph epidermidiswas the common organism.The following prophylactic antibiotics were used: ampicillin, gentamicin, cefoxitin, metronidazole and ceftriaxone. In our study, the first line using prophylactic antibiotic was 2ndgeneration cephalosporin followed by 3rdgeneration cephalosporin, with the trend to use 3rdgeneration cephalosporins in patients undergoing arthroplasty and hand transplantation. However, there was sufficient evidence to suggest that particular generation of cephalosporin is more effective in reduce to SSI.
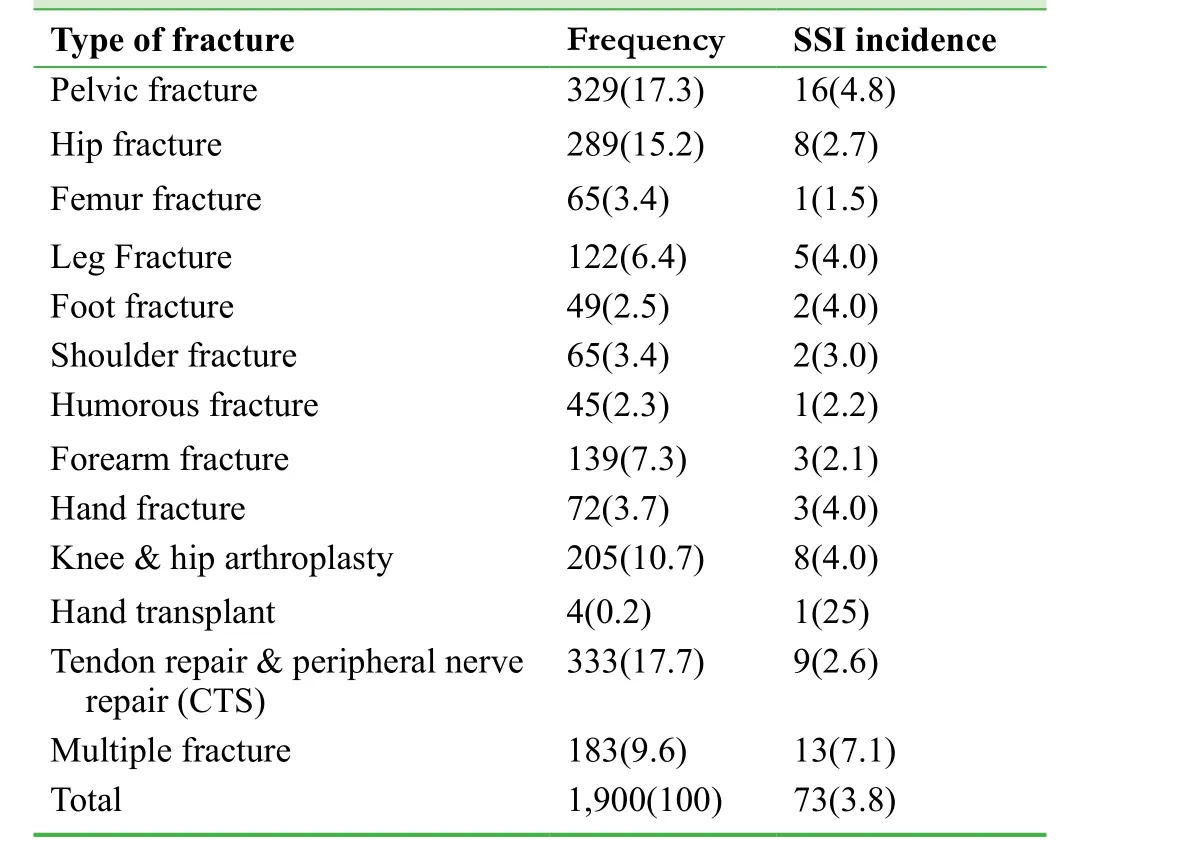
Table 2: Distribution of patients based on the type of fracture and surgical site infection (SSI) incidence

Table 3: Distribution of surgical site infection (SSI) on the basis of the following independent variables
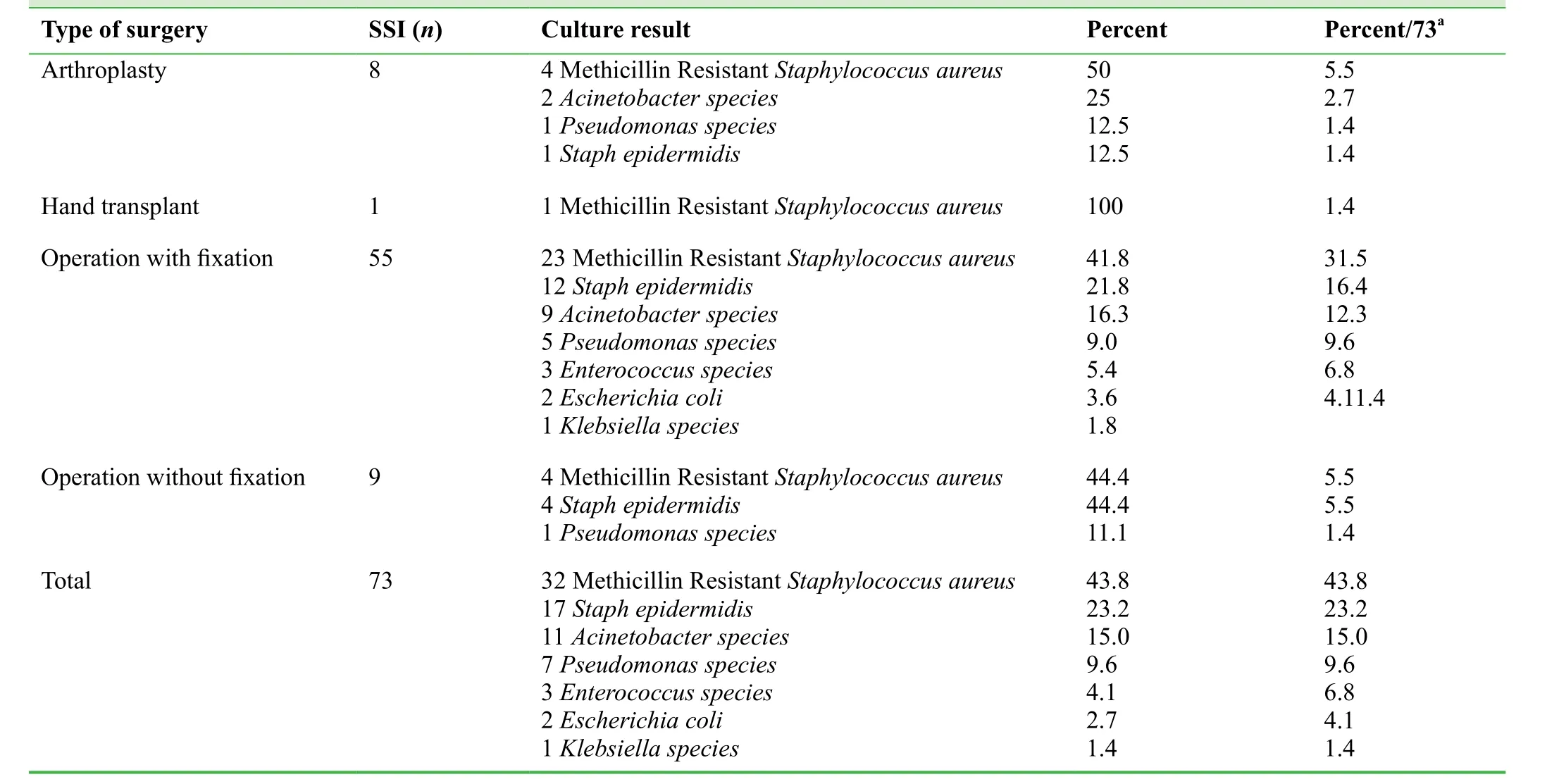
Table 4: Distribution of infective organisms in the present population
DIscussIon
The increasing rates of orthopedic surgery across many countries emphasize the importance of implementing strategies to minimize the risk of surgical site infection.11,12In this study,the SSI was reported 3.8%, which is below the reported worldwide incidence of 2.6% to 41.9%.13,14There are several known risk factors that play a role in the development of SSIs in orthopedic surgery. Although all factors increasing risk of SSI are unable to modify, identify and understand the interplay between them is critical to the formulation of prevention strategies. The staggering population rise in obesity is a good case in point, with research published in the last year emphasizing the excess risk of orthopedic infection associated with obesity.15Optimizing clinical factors such as type of prophylactic antibiotic administered before operation or make short time of surgery and hospitalization reduce the chance of SSI. Our study similar to the literature showed that SSI was more common in patients of over 50 years of age.14Data from the United Kingdom quantify the impact of being overweight or obese on the risk of infection in knee and hip replacement, with elevation in SSI rates from 0.4% to 1%.15In our study incidence of SSI in patients with high BMI was developed from 2.8% to 7%. The other independent risk factors for patients developing orthopedic SSI included an emergency operation and prolonged surgery and hospitalization.16,17
Our study showed prolonged time of surgery and hospitalization led to increased risk of SSI. The incidence rates of SSIs stratified by wound classes exceeded those reported by other studies.18In our study, contaminated and dirty or infected wounds might contribute to the high incidence of surgical site infections. It is reported that the majority of surgical site infections occur after discharge from the hospital.19Our study showed that low percentage (5.5%) of surgical site infections was probably the result of a relatively short postoperative period of hospitalization (less than 10 days).Our study supports some previously published results that infection following the surgical intervention prolongs the length of hospitalization and is costly.5,20Staphylococcus aureusand gram negative bacteria are the most common causative agents, as in other studies in a similar setting,18,21though mupirocin is effective for eradication ofStaphylococcus aureusnasal carriage and leads to reduce surgical site infections rates only in some studies.22
This study is the first study of orthopedic surgical site infections in two teaching hospitals in the west of Iran.
The merit of the study is that it confirmed that active surveillance of surgical site infections might be organized in countries with limited resources. Surgical site infections are a considerable problem in orthopedic wards in Iran but incidence rates being lower than those in other developmental countries. Identification of risk factors for surgical site infections has encouraged the development of national recommendations for prevention.
Author contributions
KM designed and directed the study, analyzed and organized the data. MR performed data collection and data analysis. SM contributed to the manuscript writing and organized tables. NM was involved in organization of data and manuscript. All authors read and approved the final manuscript.
Conflicts of interest
None declared.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Data sharing statement
No data is reported in the article.
Plagiarism check
Checked twice by iThenticate.
Peer review
Externally peer reviewed.
Open access statement
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under identical terms.
Additional file
Additional Table 1: 22-item questionnaire and cooperation with informed consent.
1. Lewis SS, Moehring RW, Chen LF, Sexton DJ, Anderson DJ.Assessing the relative burden of hospital-acquired infections in a network of community hospitals.Infect Control Hosp Epidemiol. 2013;34:1229-1230.
2. Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG.CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections.Am J Infect Control. 1992;20:271-274.
3. Poulsen KB, Bremmelgaard A, Sorensen AI, Raahave D, Petersen JV. Estimated costs of postoperative wound infections.A case-control study of marginal hospital and social security costs.Epidemiol Infect. 1994;113:283-295.
4. Boyce JM, Potter-Bynoe G, Dziobek L. Hospital reimbursement patterns among patients with surgical wound infections following open heart surgery.Infect Control Hosp Epidemiol.1990;11:89-93.
5. Whitehouse JD, Friedman ND, Kirkland KB, Richardson WJ,Sexton DJ. The impact of surgical-site infections following orthopedic surgery at a community hospital and a university hospital: adverse quality of life, excess length of stay, and extra cost.Infect Control Hosp Epidemiol. 2002;23:183-189.
6. Perencevich EN, Sands KE, Cosgrove SE, Guadagnoli E,Meara E, Platt R. Health and economic impact of surgical site infections diagnosed after hospital discharge.Emerg Infect Dis.2003;9:196-203.
7. Habte-Gabr E, Gedebou M, Kronvall G. Hospital-acquired infections among surgical patients in Tikur Anbessa Hospital,Addis Ababa, Ethiopia.Am J Infect Control. 1988;16:7-13.
8. Lecuona M, Torres-Lana A, Delgado-Rodriguez M, Llorca J,Sierra A. Risk factors for surgical site infections diagnosed after hospital discharge.J Hosp Infect. 1998;39:71-74.
9. Nyström PO, Jonstam A, Höjer H, Ling L. Incisional infection after colorectal surgery in obese patients.Acta Chir Scand.1987;153:225-227.
10. Leaper DJ, van Goor H, Reilly J, et al. Surgical site infection- a European perspective of incidence and economic burden.International wound journal. 2004;1:247-273.
11. Kassavin DS, Pascarella L, Goldfarb MA. Surgical site infections: incidence and trends at a community teaching hospital.Am J Surg. 2011;201:749-753.
12. Pronovost P, Needham D, Berenholtz S, et al. An intervention to decrease catheter-related bloodstream infections in the ICU.N Engl J Med. 2006;355:2725-2732.
13. Lilani SP, Jangale N, Chowdhary A, Daver GB. Surgical site infection in clean and clean-contaminated cases.Indian J Med Microbiol. 2005;23:249-252.
14. Skarzyńska J, Cienciala A, Madry R, et al. Hospital infections in general surgery wards.Przegl Epidemiol. 2000;54:299-304.
15. Skoufalos A, Clarke JL, Napp M, et al. Improving awareness of best practices to reduce surgical site infection: a multistakeholder approach.Am J Med Qual. 2012;27:297-304.
16. Bachoura A, Guitton TG, Smith RM, Vrahas MS, Zurakowski D, Ring D. Infirmity and injury complexity are risk factors for surgical-site infection after operative fracture care.Clin Orthop Relat Res. 2011;469:2621-2630.
17. Culver DH, Horan TC, Gaynes RP, et al. Surgical wound infection rates by wound class, operative procedure, and patient risk index. National Nosocomial Infections Surveillance System.Am J Med. 1991;91:152s-157s.
18. Thu LT, Dibley MJ, Ewald B, Tien NP, Lam LD. Incidence of surgical site infections and accompanying risk factors in Vietnamese orthopaedic patients.J Hosp Infect. 2005;60:360-367.
19. Taylor EW, Duffy K, Lee K, et al. Telephone call contact for post-discharge surveillance of surgical site infections. A pilot,methodological study.J Hosp Infect. 2003;55:8-13.
20. Vegas AA, Jodra VM, Garcia ML. Nosocomial infection in surgery wards: a controlled study of increased duration of hospital stays and direct cost of hospitalization.Eur J Epidemiol.1993;9:504-510.
21. Al-Mulhim FA, Baragbah MA, Sadat-Ali M, Alomran AS,Azam MQ. Prevalence of surgical site infection in orthopedic surgery: a 5-year analysis.Int Surg. 2014;99:264-268.
22. Kalmeijer MD, Coertjens H, van Nieuwland-Bollen PM, et al.Surgical site infections in orthopedic surgery: the effect of mupirocin nasal ointment in a double-blind, randomized, placebocontrolled study.Clin Infect Dis. 2002;35:353-358.
 Clinical Trials in Orthopedic Disorder2017年4期
Clinical Trials in Orthopedic Disorder2017年4期
- Clinical Trials in Orthopedic Disorder的其它文章
- Exercises interventions in people with rheumatoid arthritis
- Use of incisional negative pressure wound therapy in orthopedics
- Preemptive analgesia in orthopedic surgery: a literature review
- Efficacy and safety of a digital navigation template combined with cervical pedicle screw implantation: study protocol for a prospective, single-center, self-controlled, clinical trial
- Predicting necrotic femoral head collapse using computed tomographic and X-ray imaging before hip arthroplasty: study protocol and results of a single-center, open-label,diagnostic trial
