Epidemic trend, screening, and early detection and treatment of cancer in Chinese population
Xiao-Nong Zou
National Cancer Center, Cancer Institute/Hospital, Chinese Academy of Medical Sciences, Peking Union Medical College, Beijing 100021, China
Epidemic trend, screening, and early detection and treatment of cancer in Chinese population
Xiao-Nong Zou
National Cancer Center, Cancer Institute/Hospital, Chinese Academy of Medical Sciences, Peking Union Medical College, Beijing 100021, China
Epidemiological studies showed the incidence mortality rates of cancer were increasing in recent decades in Chinese population. National and regional preventive programs aim to reduce the health hazards of cancer and focuse the population at high risks for specific cancer, particularly in rural areas and to offer the access to early detection for multlple cancers in urban areas. The early screening, early detection and treatment have been put into operation for the population at risks in rural areas at first, and in the urban areas in recent years. To understand the epidemic patterns and trends of cancer, and the experiences in applying early detection strategies in China, selected literatures were reviewed for brief summary. KEYWORDS Epidemiology; screening; early detection; cancer
Introduction
Epidemiological studies show that the incidence mortality rates of cancer have increased in recent decades in the Chinese population1-9. Cancer is the second common cause of deaths among Chinese men and women (the first cause among men and the second cause among women). Early in this century, the leading cause of cancer-related mortality was lung cancer, and its incidence continues to increase1,2. In Zhejiang province, the mortality rates for cancer increased by 23% from 1976 to 19963. Lung cancer ranked first as the cause of mortality among the residents of this province in cities of all sizes. The incidence of mortality increased by 8.5% in 15 years from 1982 to 1997 in an urban (Beijing) population aim to reduce because of increased incidences of lung, colorectal, and female breast cancers4. Increased incidence and mortality rates in various sites were also observed in regional and national death studies5-9. National and regional preventive programs for reducing the health hazards of cancer started from the targeting of residents with high risk for cancer, particularly in rural areas. Strategies of screening and early detection and treatment have been implemented10-13. This review briefly summarizes originaldescriptive studies in literature to understand the patterns and trends of the cancer epidemic, as well as the advances in cancer-prevention programs in China.
National and regional cancer epidemics
Incidence and mortality in urban and rural populations
There were about 3.586 million new cancer cases and 2.187 million people died of cancer in China in 201214. The age standardized (world population15) incidence rates (WSIR) and age standardized (world population) mortality rate (WSMR) per 100,000 were 191.89 and 111.25, respectively (Table 1)14. Men had higher WSIR and WSMR (214.33 and 145.57) than women (163.81 and 78.89). The WSIR was higher in urban areas (190.88) than that in rural areas (183.91), whereas the WSMR was lower in urban areas (106.13) than that in rural areas (117.06). This result indicated different challenges, capacities, and long term effects in preventing and treating cancer in different social economic environments.
Changes of patterns and trends of common cancers
About 20% increase of age standardized (Chinese population)mortality rate (CSMR) per 100,000 for cancer occurred from 75.60 in 1973–1975 to 91.24 in 2004–20051,2. Increased rates were found in lung cancer (from 5.6 to 20.24), liver cancer (from 11.00 to 17.86), female breast cancer (from 2.88 to 3.97), leukemia (from 2.50 to 3.43), brain tumor (from 1.10 to 2.37), malignant lymphoma (from 1.20 to 1.60), and bladder cancer (from 0.50 to 0.85). Decreased mortality rates were found in cancers of the cervix uteri (from 11.10 to 1.89), esophagus (from 17.10 to 9.98), nasopharynx (from 2.00 to 1.01), and stomach (from 17.70 to 16.16) from 1973–1975 to 2004–2005.
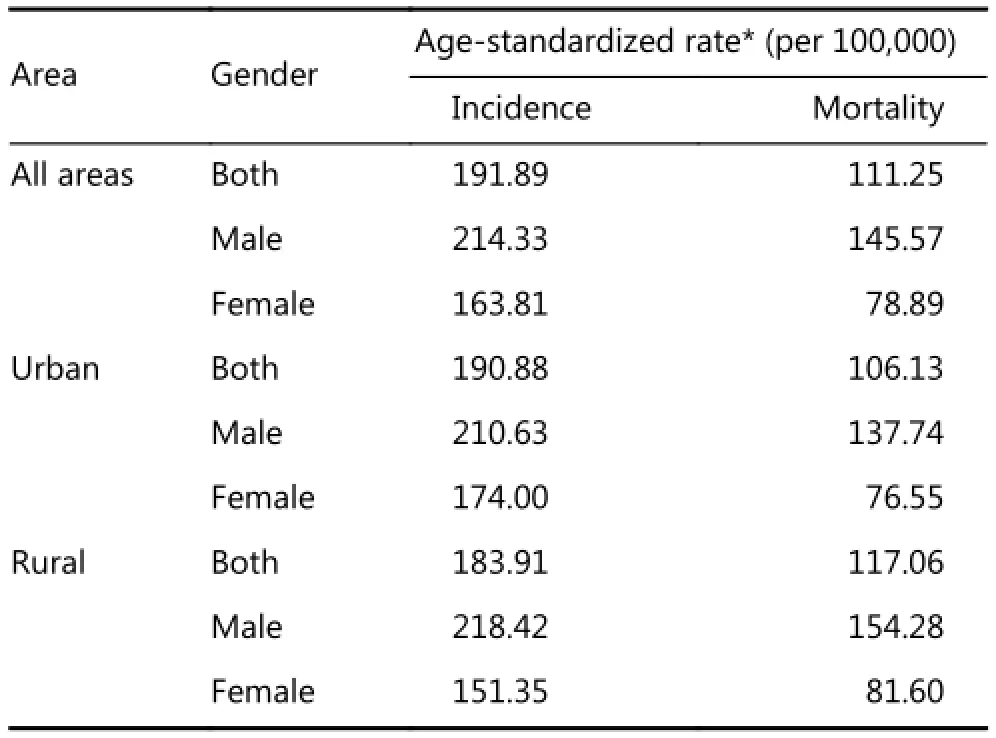
Table 1 Incidence and mortality of cancer in China in 2012
Multicentral and regional patterns and trends
Increased rates in cancers of lung, colorectum, liver, and female breast
Lung cancer mortality showed particularly dramatic increase in recent decades based on the reports of the National Death Surveys as observed in increasing cancer mortality rates in the Chinese population. Lung cancer is the leading cause of mortality surpassing cancers of the esophagus, liver, and stomach observed at the national and some regional levels in China1-3,5-7. The WSMR from lung cancer was 27.62 in 2004–2005, an increase of 20.32 compared with that in 1973–1975 (7.30)2,7. Although differences in WSMRs existed for lung cancer between males and females, urban, and rural populations in each study time period, increases in lung cancer WSMR were seen consistently across the different categories. The increased incidence rates of lung cancer were found not only in the areas with relatively developed social economical status, such as Beijing4, Zhejiang province3, and Dalian in Liaoning province5, but also in the less developed rural areas, such as Ci county in Hebei province6.
In 2003 to 2007, breast cancer was the leading cancer in Chinese females, accounting for 19.62% of new cancer cases based on the data from 32 cancer registries16. In urban population, the rates of incidence and mortality of breast cancer were 3.04 times and 1.92 times higher than those in rural areas, respectively. High incidence rates of breast cancer were found in Guangzhou in Guangdong provinces (34.08), Dalian in Liaoning province (31.20), and Shanghai (30.28). In addition, high mortality rates were found in Shanghai (6.44), Guangzhou in Guangdong province (6.43), and Harbin in Heilongjiang province (6.26). All those were relatively industrialized population. The WSIRs of breast cancer increased from 25.81 to 33.96 in women living in urban registration areas of China, and from 9.00 to 15.63 in the rural registration areas from 1998 to 200717.
The increasing incidence and mortality rates of colorectal cancer were observed in 10 Chinese cities from 1988 to 200218. The age-standardized incidence rates (ASIRs) in 1988–1992 and 1998–2002 increased for colon cancer per 100,000 (5.71 and 9.11) and rectal cancer (5.38 and 7.48). Rapid increases of the incidence of colorectal cancer were from the age of 65 years in both men and women. Differences in the age-specific rates became obvious after the age of 60 years, particularly in urban population. In general, the rates for colon cancer were higher than the rates for rectal cancer. Colon cancer was common in the urban areas. Rectal cancer was common in the rural areas.
Analysis on the data of 10,201 cases, including 3,420 cases in 1980–1989, and 6,781 cases in 1990-1999 from 25 hospitals found that the patterns of colorectal cancer were changing19. The percentages of the female patients increased significantly, with the ratios of male to female changing from 1.50:1 to 1.26:1. During the two periods, the proportion of proximal colon cancer, including transverse and ascending colon cancers increased significantly from 10.9% to 15.2%, whereas the proportion of rectal cancer decreased from 72.6% to 66.9%. The proportion of adenocarcinoma increased significantly from 82.1% to 85.6%, whereas mucinous adenocarcinoma decreased from 15.2% to 10.4%.
Decreased rate in cancers of esophagus/stomach and nasopharynx
The WSMRs of esophageal cancer showed a decreasing trend in three national death surveys from 23.20 in 1973–1975 to 13.73 in 2004–200420. Both the WSMRs for men and women decreased from 31.40 and 15.80 in 1973–1975 to 19.66 and 8.02 in 2004–2005. Consistently decreasing CSMRs wereobserved in urban (from 15.50 to 6.48) and rural (from 17.70 to 12.01) areas.
The crude and CSMR of stomach cancer were 24.71 and 16.16, respectively, accounting for 18.19% and ranking third of cancer causes in the national sampling areas of China in 2004–200521. Those crude death rates increased by 42.01%, whereas the age standardized death rate decreased by 8.70% compared with the results in 1973–1975 (17.40 and 17.70). Both decreased by 1.79% and 25.74% from 1990–1992 (25.16 and 21.76), respectively. Among urban residents, the crude and CSMR of stomach cancer were 22.98 and 13.63, accounting for 15.03% of cancer causes in 2004–2005, which increased by 18.21% and decreased by 31.16% from 1973–1975 (19.44 and 19.80), and increased by 18.21% and decreased by 11.15% from 1990–1992 (19.44 and 15.34), respectively. Whereas, for rural residents in the sampling areas, the crude and CSWR were 25.59 and 17.64, accounting for 19.89% of cancer causes. Both increased by 53.97% and 3.765% from 1973–1975 (16.62 and 17.00), and both decreased further by 5.78% and 27.59% from 1990–1992 (27.16 and 24.36), respectively.
In regions covered by the cancer registries in 2009, the crude incidence of nasopharyngeal carcinoma (NPC) was 3.61 (5.08 in males and 2.10 in females; 4.19 in urban areas and 2.42 in rural areas)22. The WSIR and WSMR of NPC were 2.54 and 1.35, respectively. The incidence and mortality of NPC were higher in men than that in women and higher in urban areas than that in rural areas. Both age specific incidence and mortality were relatively low in persons younger than 30 years old. However, these rates dramatically increased. Incidence peaked in the ages 60–64 years and mortality peaked in the ages 85 years and old.
North China
A total of 32, 845 new cases with lung cancer were identified in the central areas in Beijing from 1998 to 200723. The WSIRs increased slightly from 27.70 to 29.10. Changes of survival rate of breast cancer were observed from 62.0% in 1982–1983 to 68.7% in 1987–199224.
The histological subtypes of lung cancer changed in both genders from 2000 to 2012 observed in hospital-based statistics in Beijing25,26. The relative frequencies (RF) of histological subtypes of lung cancer showed similar changes in both genders in the study period. The RF of adenocarcinoma (ADC) increased from 21.96% to 43.36% among men, and from 46.72% to 76.49% among women. Decreased RFs were found in cases with squamous cell carcinoma (SCC) from 39.11% to 32.23% in males and 10.21% to 8.12% in females. The changes were found not only in the cases from the residents of Beijing but also in the cases from other areas, such as Hebei, Shanxi, and Inner Mogolia.
The mortality of esophageal cancer decreased in a 22-year study in Tianjin27. A total of 8, 206 cases of esophageal cancer were reported in Tianjin from 1981 to 2002 with 5, 533 males and 2, 673 females. The age-specific incidence rate for esophageal cancer was very low before 45 years but increased rapidly after 45 years. The crude and ASIR of esophageal cancer decreased in the last 22 years. The ASIR decreased by 5.18% in men and 6.56% in women.
Significant changes in the incidence rates were observed in Ci county of Hebei province, a population with high risk for esophageal cancer28. A total of 12,813 cases, 7,953 among men and 4,860 among women, died of esophageal cancer during 1988 to 2011. Averaged WSMR in the study period was 112.92. The WSMR of esophageal cancer dramatically declined from 183.19 in 1988 to 72.80 in 2011. Another study in Ci county showed obvious increasing trend of lung cancer incidence from 1988 to 20036. For men and women in the Ci county, the incident rates were 25.22 and 14.67 in 1988–1989, 24.01 and 12.17 in 1990–1999, 43.45 and 24.21 in 2001–2003, respectively.
East China
From 1975 to 2005 in Shanghai city, cancer incidence of all sites for males and females was increasing consistently, 46.5% for males and 66.0% for females29. However, the SIR for males decreased by 15.5%, and for females increased by 12.9%. Among common cancers, stomach, liver, prostate, ovary, and cervical cancers decreased consistently. Whereas, lung and thyroid gland cancers had no significant change during the study periods. Liver cancer decreased significantly in urban cities, such as Shanghai30. In male residents of Shanghai, the ASIR for liver cancer decreased yearly by 1.6% and in women by 1.5% during 1972–2001. The rates were higher in the residents in the suburban (34.56) than those in the urban (26.51) areas.
In Qidong city of Jiangsu province, the WSMR and the proportions of the cases with lung cancer of all cancer cases were from 8.71% and 8.09% in 1972 increasing to 63.53% and 25.12% in 2008–2011 by 2.04% of annual percent increase from 1972 to 201131.
Increases in cervical cancer incidence rate were reported in the residents of Kunshan in Jiangsu province32. The crude rates increased from 6.34 to 16.84 by 13.1% (95% CI: 0.078-0.184) of annual percent change (APC). In addition, the WSIRs increased from 4.99 to 12.30 by 12.5% (95% CI: 0.068-0.182) of APC from 2006 to 2013. Significant increasewas observed in the ages 25 to 45 years old.
Among the residents in Xiacheng District of Hangzhou in Zhejiang province, the most common cancer included cancers of the lung (16.32%), colorectum (12.93%), stomach (8.96%), breast (8.4%), and liver (7.41%), and the most common deaths from cancer were cancers of the lung (25.16%), colorectum (12.92%), liver (11.79%), stomach (10.80%), and pancreas (7.41%)33. The age-specific incidence rates for lung cancer increased tenfold from ages 15 to 44 years (4.98) to ages 45 to 59 years (58.65), and increased again in ages 60 years and above (251.03).
The WSMR of cancer in Shandong province increased from 87.64 in 1970–1974 to 139.01 in 2004–200534. In the period from 1970–1974 to 2004–2005, increased WSMRs were observed for lung cancer (from 8.23 to 18.39), liver cancer (from 12.11 to 24.96), intestinal cancer (from 4.21 to 5.42), and breast cancer (from 2.91 to 4.11), and decreased WSMRs were for esophageal cancer (from 22.34 to 18.39), and cervical cancer (from 21.11 to 1.16). Lung cancer increased from the fourth rank in 1970 to the first in 2005, whereas cervical cancer dropped from the fifth rank to the eighth place. Esophageal and cervical cancers decreased annually, whereas gastric cancer increased in the early days but decreased later on. The rest of the cancers were on the rise year by year. Rates of lung and breast cancers were higher, whereas gastric and esophageal cancers were lower in the urban than in rural areas.
Increased incidence rates for cancer were observed in rural residents in Feicheng city, Shandong province from 2000 to 201235. The ASIR increased from 159.4 in 2000 to 251.3 in 2012 (from 216.1 to 354.8 in males and from 107.4 to 171.5 in females). In males, average APC of the incidence rates was 7.7% for lung cancer, 3.1% for stomach cancer, 2.5% for esophageal cancer, –1.5% for liver cancer, whereas in females were 10.0% for breast cancer, 8.0% for lung cancer, 2.4% for stomach cancer, 1.1% for esophageal cancer, and –1.5% for liver cancer.
Stomach cancer was observed in a decreasing trend in Changle, a rural county in Fujian province with especially high risk of stomach cancer36. During the time periods from 1973–1975 to 1994–2000, unlike the upward trends observed for cancers of the lung, liver, and colorectum, the mortality rates of stomach and esophageal cancers reduced by 28% and 34.5%, respectively.
Northeast and Northwest China
Epidemic trend of lung cancer incidence in Dalian city of Liaoning province showed that the proportion of SCC of lung cancer decreased from 47.6% in 1991–1995 to 29.46%. ADC increased from 38.46% to 52.61% in 2006–201037.
In a general hospital of Qinghai province in Northwest China, the total numbers and the proportions of malignant cases among all hospital patients increased significantly from 1,555 (7.8% of total patients) in 2000 to 2,402 (13.30%) in 200538. The proportion of cancer cases was 3.07% in 1974–1991 and 7.31% in 1998–1999 to 10.03% in 2000–2005 among the patients in this hospital. Stomach cancer was the most common malignant tumor, followed by cancers of the cervical uteri, lung, esophagus, and liver in 1974–1982. Whereas, the numbers of stomach cancer changed from 1,338 (34.9%) in 1974–1982 to 2,154 (17.9%) in 2000–2005. The number of cases with lung cancer increased from 470 (12.3%) in 1974–1982 to 1,738 (14.5%), ranked as the second most common cancer followed stomach cancer in 2000–2005.
In Liangzhou District of Wuwei county, a rural area in Gansu province, about 80% of malignant diseases occurred in the digestive tract39. The WSIRs for cancer increased from 312.2 to 491.6 in men, and from 166.7 to 184.1 in women from 2001 to 2010. Among men, increased rates were found in cancers of the stomach (from 86.2 to 142.8), esophagus (from 40.6 to 61.9), lung (from 6.1 to 20.6), liver (from 14.5 to 19.6), and colorectum (from 5.5 to 14.4). Among women, increased rates were found in cancers of the stomach (from 29.4 to 44.1), esophagus (from 15.1 to 22.2), lung (from 3.0 to 12.1), breast (from 7.0 to 17.8), and liver (from 7.0 to 7.8) in the same time periods.
The standardized mortality rate of malignant tumors was 97.79 in Yuzhong county in Gansu province from 1997 to 2006, ranked second in all causes of death40. The male-tofemale ratio was 1.57:1. The age distribution of death from malignancy revealed a relatively low death rate in the less than 40-year-old group, whereas the mortality gradually increased along with age in the greater than 40-year-old group. The top five malignant tumors regarding the mortality rate in the decade were gastric, liver, lung, esophageal, and colorectal cancer, accounting for 82.90% of all death cases because of malignancy. The mortality rate was contributed mainly by gastrointestinal tumors, according to the epidemiological analysis of major malignancies, whereas the mortality of liver and lung cancers presented to be increasing by year.
Central China and South China
During the period of 1974 to 1999, marked changes have taken place in the Henan province in cancer mortality rates of certain sites41. Esophageal and cervix carcinoma showed a marked decline. Esophageal cancer mortality rates decreasedover the period studied for males from 43.55 in 1974–1976 to 26.47 in 1996–1998, and for females from 22.47 in 1974–1976 to 15.63 in 1996–1998. Mortality rates for cervix cancer decreased during the period studied from 10.78 in 1974–1976 to 3.18 in 1996–1998. Stomach cancer mortality rates did not change substantially during the period studied. Liver cancer mortality rates for males have increased clearly over the last two decades from 11.39 in 1974–1976 to 20.79 in 1996–1998, and for females from 5.12 in 1974–1976 to 10.08 in 1996–1998. Lung cancer mortality rates for males increased nearly three times over the period studied from 5.96 in 1974–1976 to 17 in 1996–1998, and for females from 2.52 in 1974–1976 to 7.78 in 1996–1998. Total cancer mortality rates declined recently but not significantly. Cancers of the esophagus, stomach, liver, and lung account for over 85% of all cancer deaths in men. Whereas, the leading cancers of women include cervical and breast cancers in addition to the four common cancers in men, making up to 84%.
The patterns of esophageal cancer incidence in male residents in Zhongshan city, Guangdong province of South China were quite different from most other domestic areas and a continuous and obviously increasing trend was reported for male incidence rates in 1970–2007 in the population living in this area42. SCC was the major pathological type, accounting for 70.6% of all new cases, whereas adenocarcinoma was relatively low and accounted for 2.66% throughout the period.
In Guangxi of South China, liver cancer was the leading cause of cancer accounting for 40.82% of cancer death in 1973–197543. In nine cities/counties, the sampling population of Guangxi in the national death survey, liver cancer contributed to 22.73% to 59.40% of cancer deaths in males and 18.63% to 53.19% of cancer deaths in females in 1990–1992. The ASMRs of liver cancer increased from 16.49 in 1973–1975 to 24.43 in 1990–1992 in Guangxi. These changes were consistently found in males (from 24.67 to 38.01) and females (from 6.73 to 9.96). In Fusui county of Guangxi, the ASIRs of liver cancer were particularly high, 51.03 in 1988 and 57.64 in 1997. Slight reduction of ASMR for liver cancer in men was observed this early century (from 81.12 to 79.95)44.
Five major cancers including liver, lung, gastric, nasopharyngeal, and colorectal cancers account for 60% of all the cancer deaths in Guangxi, a provincial area in South China45. Cancers with growing mortality rates over the past 30 years include lung, colorectal, liver, and female breast cancer, of which lung cancer is associated with the sharpest rise in mortality with more than 600% increase in both men and women. Cancer death in Guangxi residents occurs mainly in the elderly population above 45 years of age, especially in people over the age of 65. The areas with the highest mortality rates for liver cancer and NPC, which feature regional high incidences, include Chongzuo and Wuzhou. The WSMR of cancer increased from 58.04 per 100, 000 in 1971–1973 to 108.85 in 2004–2005 in Guangxi. Dramatic increases were observed in the CSMRs of liver cancer (from 28.02 to 41.97), lung cancer (from 2.85 to 22.22), and stomach cancer (from 7.52 to 12.06) among men, and lung cancer (from 1.28 to 9.38) among women during 1971–1973 to 2004–2005.
Southwest China
In Chongqing, the mean crude mortality of malignant tumor in 2004–2005 was 145.28. The standardized mortality was 78.84. The mortality from 35 to 64 years old was 126.29, and the accumulative rate was 11.24%46. The malignant tumor ranked as the first cause of all deaths, and its proportion in all deaths was 23.13%. The top five causes of death in all malignant tumors were cancer of the lung, liver cancer, carcinoma of the colon and rectum, carcinoma of the stomach, and carcinoma of the esophagus. The male and female standard mortality was 105.20 and 52.03, respectively. Lung cancer was the first cause of death among residents in urban areas, accounting for 37.17% of all malignant tumors. The standard malignant tumor mortality in 2004–2005 among the urban areas in Chongqing decreased from that in 1990–1992 (173.85). The lung cancer mortality in 2004–2005 was lower than the mortality in 1990–1992 (58.74) and the average mortality in 1991–2000 (63.44).
Hospital data showed that 71% of the patients with lung cancer was male, and the ratio of male to female was 2.45:1 (7,335/2,996) during 2005–2015 in Yunnan province47. The majority of the patients (60.46%, 6246/10,331) was between 50 and 69 years old. A statistical significant difference was observed in pathological types between males and females. Lung cancer foci occurred most often in the upper lobe and ADC (35.60%) was the most pathological type exceeding SSC (24.65%).
Yanting county of Sichuan province was a high risk area for esophageal cancer. A total of 20,926 persons had developed esophageal cancer and 15,204 people died from esophageal cancer during 1969–200348. The average WSIR for esophageal cancer was 173.81 in men and 77.90 in women, and WSMR was 119.21 in men and 77.90 in women in 1969–1973. The WSIRs were reduced from 156.43 in 1969–1973 to 96.36 in 1999–2005 in males, and from 94.96 in 1968–1973 to 57.71 in 1999–2003 in females. The WSWRs showed similar declining trends from 108.02 to 73.65 in men,and from 70.61 to 47.39 in women during the same time period.
Screening and early detection and treatment
The promotion strategies for early detection of cancer were enhanced in China since 200511. The in-depth interpretation included the following aspects, the guidelines, recommendations, the progress of demonstration centers for early detection of cancer, and the programs of cancer early detection subsidized by the central government. Evaluation study reported promising results from Screening, Early Diagnosis, and Early Treatment (SEDET) program introduced to high risk population in rural areas12. Cancer at early stages was identified and diagnosed, 94% of cervical cancer, 70% of esophageal cancer, 80% of stomach cancer, 90% of colorectal cancer, 63% of liver cancer, 92% NPC, and 51% of lung cancer (Table 2)12. After a thorough discussion of the challenges and countermeasures in implementation of sustainable early cancer detection and intervention, the goal of future program had been developed and advanced into practice and research49-52. These programs have been expanded to the urban areas focusing on the population at high risks for cancer and the management method has been released by the National Ministry of Health in 201313. The cancers of the lung, breast, colorectum, uppergastrointestinal tract, and liver, the most common cancers occurring in Chinese population, are included in the program of urban SEDET.
Screening for esophageal and gastric cancers
Severe dysplasia and some moderate dysplasia were found in the esophagus and considered as precancerous lesions10. Field studies suggested that if these precancerous lesions can be detected and treated, the cancerization risk of target population will reduce dramatically and the incidence of esophageal cancer will be decreased.
A total of 4,800 subjects from a high risk area of esophageal cancer in Linzhou city, Henan province were examined by endoscopy from 1985 to 199052. Among them, 132 cases were diagnosed as early esophageal cancer. Based on the criteria, the lesions were endoscopically diagnosed as superficial mucosal lesions and histopathologically confirmed by biopsy as carcinoma in situ, intramucosal carcinoma or squamous cell carcinoma. A total of 48 of the 132 patients, who refused treatment, were followed up at the end of 2005. Among them, 43 died, 5 lived, and 40 patients were reexamined for one to four times by endoscopy during the follow-up. A total of 48 patients have been followed up for 20 years. Up to 38 (79.2%) cases died of esophageal squamous cell carcinoma, five (10.4%) died of esophageal squamous carcinoma, and five (10.4%) were surviving. Approximately 37 patients had survived for over 5 years. The 5-, 10-, 15-, and 20-year survival rates were 77.1%, 39.6%, 25.0%, and 10.4%, respectively.
In three years, 36,154 people were screened, and 16,847 (46.60%) cases were found to have precancerous lesions in the population at high risk for esophageal/gastric cancer in Henan province53. Screening showed that the gastric precancerous lesions occur in 23.23% of the population, gastric cardio precancerous lesions occur in 23.36% of the population and various esophageal, gastric cardia, and gastric carcinoma occur in 2.42% of the population in which 84.46% of cases are early stage cancer. In all the male and female cancer patients, the incidence of in situ/high-grade neoplasia, mucosal carcinoma, submucosal carcinoma, and invasive carcinoma is 1.42%, 0.41%, 0.21%, and 0.38%, respectively. The detection rate of esophageal and gastric carcinomas in the group of 40–44 years old is 2.34%, accounting for 9.41% of the total population screened.
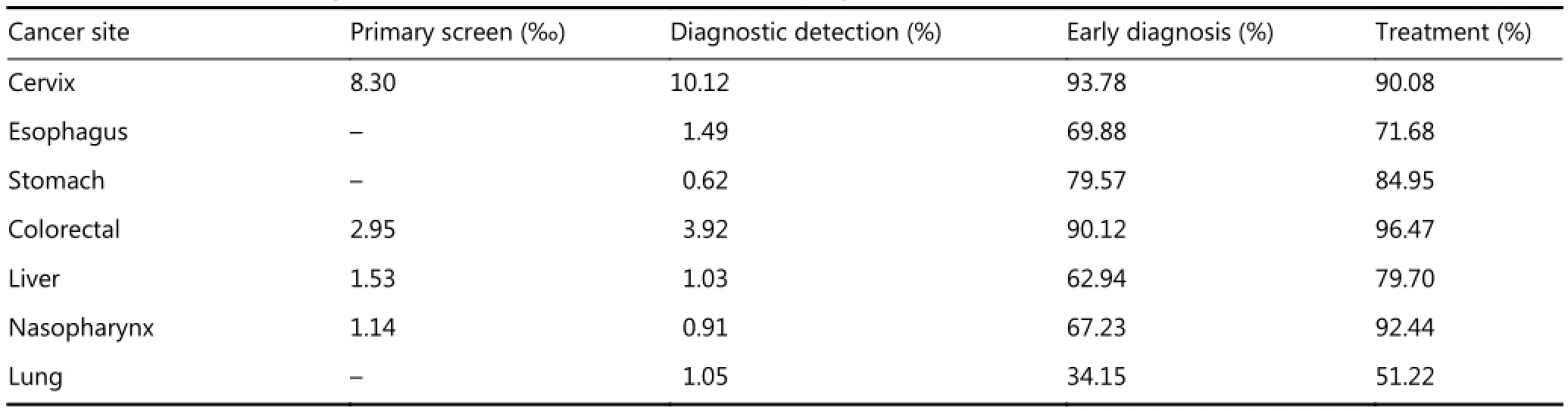
Table 2 Rates of screen, diagnosis, and treatment for cancer in SEDET programs
Random cluster sampling was used to select a proportion of natural villages from six towns in Yanting, and residents aging 40–69 years old were invited for screening54. Participants were screened using endoscopy with iodine staining and then confirmed by histological examinations. The overall detection rates of low-grade hyperplasia (LH), moderate hyperplasia (MH), high-grade hyperplasia (HH), carcinoma in situ, intramucosal carcinoma (IC), and invasive carcinoma (INC) were 5.33%, 1.28%, 0.68%, 0.15%, 0.06%, and 0.29%, respectively. The detection rates of LH, MH, HH, and INC increased with age, reaching the peak among those aged 60–65 years. The prevalence of LH and MH was higher among men than among women. In addition, the detection rates of hyperplasia were much higher in mountainous than in hilly areas.
Endoscope-assisted iodine staining and indicative biopsy screening were adopted in a random screening program in Bazhong city, a high risk area of esophageal cancer in Sichuan province55. The detecting rate of esophagus inflammation, mild, moderate, and severe esophageal hyperplasia, and esophageal cancer were7.81% (513/6,571), 5.63% (370/6,571), 1.99% (131/6,571), 0.79% (52/6,571), and 0.21% (14/6,571), respectively. The detecting rates of esophageal lesions at various grades in males were higher than those in females. The analysis depending on different age scopes found that the composition of the detecting rate of each grade of esophageal lesion between different age groups was significantly different. Combined with the age distribution figure, the detecting rate of esophageal inflammation and mild and moderate hyperplasia showed an increasing tendency with age.
Screening for colorectal cancer
Screening for colorectal cancer was recommended by the Chinese Cancer Foundation in high risk areas of China. In Haicang District of Xiamen in Fujian province, 81.06% of 1,035 high risk people obtained by questionnaires and fecal occult blood test (FOBT) accepted complete colonoscopy56. Positive incidence of colorectal cancer and adenomatous polyps and other lesions were 1.67% and 23.96%, respectively. Colorectal cancer detection rate was higher in the participant positive to both questionnaires and FOBT than those positive to questionnaire or FOBT alone. Colorectal cancer detection rate was slightly higher in FOBT twice positive than once positive or negative. Linear relationship was observed between times of detection rate in FOBT positive and colorectal cancer, and adenomatous polyps and other lesions detected.
At 19 screening sites in Wuhan, 63,961 residents were recruited as target population according to the sequential fecal occult blood test (SFOBT) between 2005 and 200857. Residents aged over 40 years old received SFOBT. Those with positive SFOBT underwent colonoscopy. Among the 25,837 people aged over 40 years, 7,784 participants received SFOBT screening with a medium age of 56 years old. The positive rate of SFOBT was 12.3% (956 persons). Of the 956 persons, 240 participants underwent colonoscopy. Colorectal cancer was found in 14 cases (6.5%), gastric cancer in 2 cases (0.9%), colorectal adenoma in 53 cases (24.8%), colorectal inflammation in 80 cases (37.3%), and hemorrhoids in 65 cases (30.4%). Study showed that the prevalence of colorectal cancer is relatively high in Wuhan and the SFOBT is available and feasible in screening early changes of colorectal cancer.
Screening for cervical cancer and breast cancer
In Xiangyuan county of Shanxi province, a total of 1, 530 women were enrolled in a combined screening of cervical cancer, breast cancer, and reproductive tract infections (RTI), including cervicitis, trichomona vaginitis, and bacterial vaginitis58. The prevalence of cervical precancerous lesions, suspicious breast cancer, suspicious benign breast disease, and RTIs was 1.4% (21/1,530), 0.2% (3/1,530), 14.0% (214/1,530), and 54.3% (831/1,530), respectively. Dividing the cervical lesions by histopathology stage, the prevalence of cervical intraepithelial neoplasia (CIN) grade 1, CIN grade 2, and CIN grade 3 was 1.1% (17/1,530), 0.2% (2/1,530), and 0.1% (1,530) for the participants, respectively. The most commonly perceived cervical cancer risk factors among participants included the numbers of sexual partners (67.9%), of abortions (60.6%), of pregnancies (59.0%), the age of sexual debut (49.7%), and infection with high risk human papilloma virus (HPV) (20.9%). For breast cancer, the most commonly perceived risk factors were personal characteristics (43.5%), smoking and drinking (43.3%), age (43.1%), obesity (43.1%), and breastfeeding (42.1%). Risk factors of reproductive tract infections, multiple sexual partners (68.6%), and multiple abortions (61.7%) gain the highest perceived rate. In addition, the frequency of vaginal cleaning (56.5%) and vagina-specific cleaning basin and towels (54.3%) were also recognized as common perceived risk factors. Combined screening program showed to be more effective and popular than single disease screening project.
A total of 69,532 women participated in a questionnaire survey for high-risk of breast cancer in Changsha city59. Up to 13,805 women were rated as high-risk group accounting for 19.9%. Among those a total of 1,906 persons received screening by ultrosound alone, and 4,133 received screeningby ultrasound combined with X-ray photograph. Positive detection rate of ultrasound was 774 per 100,000, and that with X-ray photography was 560 per 100, 000. Consistency analysis showed that kappa coefficient of the two methods was 0.394.
In 2012, screening on two cancer (cervical and breast) programs was conducted among the women in Xinjiang, Northwest China60. Women aging 35 to 64 years in those areas were invited to participate for screening on cervical cancer in 84 counties, whereas 46 counties were selected for breast cancer. The prevalence of common gynecologic disease was 56.10% and the detection rate in Tacheng Prefecture ranked first (74.56%), followed by Aksu Prefecture (64.35%) and Yili (61.42%). A total of 5,365 (1.50%) women were diagnosed as IIb cases, 6,329 (1.77%) as atypical dysplasia, 1,139 (0.32%) as low-grade squamous intraepithelial lesions (LSIL), 437 (0.12%) as high-grade squamous intraepithelial lesions, and 28 (0.01%) as squamous carcinoma among 13,360 women considered as candidates for colposcopy exam during diagnostic test in primary screening. The early cases contributed to 85.05% of the cervical cancer. For screening on breast cancer, the average detection rate in primary screening was 0.05% considered as early cases.
The prevalence of high-risk HPV, low-risk HPV, and total HPV was 7.25%, 1.59%, and 8.27% respectively in Uygur women in Yutian county of Xingjiang61. The prevalence of above CIN II and cervical cancer was 1.93% and 0.23%. The ratio of high-risk HPV in ASCUS, LSIL, and HSIL was13.46%, 64.71%, and 90.00%, respectively. Lower prevalence rate was found in the women of Uyghur than that in Han nationality.
Screening for lung cancer
Low-dose computed tomography had been applied in screening for early cancer of the lung in people at high risks. Among the 4,690 asymptomatic persons, those ≥ 40 years old underwent chest low dose spiral CT at the Cancer Hospital, Chinese Academy of Medical Sciences. The percentages of positive results of baseline CT were 27.0%, 19.3%, and 11.3% in various risk status groups of the participants62. A total of 26 participants (11 men and 15 women) were diagnosed as early cases of lung cancer, including 1 as limited disease and 25 within stage I. The surgical resection rate was 88.5% (23/26).
Screening for major cancers in urban areasbeen initiated in urban areas in recent years. A report from Hunan province showed the feasibility and basic data. The implementation of high-risk assessment for cancer had identified 1,279 persons (12.62%) with precancerous lesions in urban population of Changsha63. The detective rates for precancerous lesion were 28.01% for the lung, 0.13% for the liver, 11.86% for the breast, 2.26% for the upper digestive tract, 14.48% for the colorectum, and 0.47% for lung cancer, 0.29% for liver cancer, 0.78% for breast cancer, 0.20% for upper digestive tract, and 0.68% for colorectal cancer. Although limited information had been gathered, the preliminary results showed that the program had been progressing well.
Epidemiological investigation and cancer risk evaluation were launched among 40~60-year-old residents in Hangzhou and Ningbo cities64. Of the 41,547 residents, 5,838 were assessed with high risks for lung cancer, 5,228 for liver cancer, 9,672 for upper digestive cancer, 2,727 for female breast, and 4,911 for colorectal cancer. The detective rates of confirmed/suspected cancers included 2.42% (72/2,975) from the lung (suspected), 6.71% (103/1,534) from the breast (BI-RADS grades 4–5), 0.32% (6/1,891) from the upper digestive tract, 0.04% (1/2,570) from the liver, and 0.75% (8/1,068) from the colorectum.
Conclusions
The patterns and trends of cancer epidemics had been changing in recent decades in Chinese population. Increased cancer incidence and mortality rates, particularly lung cancer, were consistently reported from the studies in urban and rural areas and in national and regional levels. The promotion strategies for early detection of cancer have been enhanced with promising advances. Follow-up and evaluation studies should be strengthened and focused on effective screening frameworks and techniques to reach the target populations and individuals. Stratified and precise preventive and control strategies should be developed for the populations with various natural and social-economic resources and the challenges from specific cancer epidemics.
Conflict of interest statement
No potential conflicts of interest are disclosed.
Targeting on several sites in one framework of screening has
1.
Chen Z. Report on Third National Retrospective Sampling Survey on Causes of Death in China. Beijing: Chinese Union MedicalUniversity Press. 2008: 10–7.
2.Chen WQ. Lung cancer. In: The National Office for Cancer Prevention and Control, National Central Cancer Registry, Disease Prevention and Control Bureau, Ministry of Health of the People's Republic of China, eds. Report of Cancer Death in China-Three National Retrospective Sampling Death Surveys. People’s Health Press: Beijing. 2010: 24-36.
3.Mao WM, Shu Y, Chen WY. The trend on morbidity and mortality of lung cancer during recent 30 years in Zhejiang province. Bull China Cancer. 2002; 11: 216–7.
4.Wang QJ, Zhu WX, Xin XM, Li L. The trend of cancer incidence in urban Beijing from 1982 to 1997. Bull China Cancer. 2001; 10: 507–9.
5.Zhang LM, Lin H, Mei H, Zhou YQ, Lv DX. An analysis of epidemic trends of lung cancer from 1991 to 2005 in Dalian City, Liaoning province. Bull China Cancer. 2008; 17: 84–7.
6.He YT, Hou J, Chen ZF, Song GH, Meng FS, Qiao CY, et al. Analysis of incidence trend of lung cancer in Ci county for 16 years. Modern Prev Med. 2008; 35: 3256–9.
7.Zhi XY, Zou XN, Hu M, Jiang Y, Jia MM, Yang GH. Increased lung cancer mortality rates in the Chinese population from 1973-1975 to 2004-2005: an adverse health effect from exposure to smoking. Cancer. 2015; 121: 3107–12.
8.Li QH, Ma WL, Yao KY. An analysis of incidence trend of female breast cancer in Jiashan county, Zhejiang province, 1988-2012. China Cancer. 2015; 46: 22–6.
9.Zhu C, Li HZ, Du LB, Mao WM, Wang XH, Yu CD, et al. An analysis of cancer incidence and mortality from Zhejiang cancer registries in 2011. China Cancer. 2015; 24:170–80.
10.Wang GQ. 30-year experiences on early detection and treatment of esophageal cancer in high risk areas. Acta Acaed Med Sin. 2001; 23: 69–72.
11.Dong ZW, Qiao YL, Kong LZ, Wang GQ, Meng XZ. The strategy and implementation for early detection of cancer in China. Bull China Cancer. 2008; 17: 256–63.
12.Dong ZW, Qiao YL, Wang GQ, Zhang SZ, You WC, Qian GS, et al. Evaluation of early diagnosis and early treatment of cancer. Chin J Oncol. 2012; 34: 637–40.
13.Ministry of Health, People’s Republic of China. Management Method for the program of early diagnosis, early treatment of cancer in the urban (trail implementation). Chin Prac J Rural Doctor. 2013; 20: 1–2.
14.Chen WQ, Zheng RS, Zhang SW, Zeng HM, Zuo TT, Jia MM, et al. Report of cancer incidence and mortality in China, 2012. China Cancer. 2016; 25: 1–8.
15.Boyle P, Parkin DM. Statistical methods for registries. In: Jensen OM, Parkin DM, MacLennan R, Muir CS, Skeet RG, eds. Cancer Registration: Principles and Methods. IARC: Lyon. 1991: 126–58.
16.Huang ZZ, Chen WQ, Wu CX, Zheng RS, Chen JG, Yang NN, et al. Incidence and mortality of female breast cancer in China–a report from 32 Chinese cancer registries, 2003-2007. Tumor. 2012; 32: 435–9.
17.Li N, Zheng RS, Zhang SW, Zou XN, Zeng HM, Dai Z, et al. Analysis and prediction of breast cancer incidence trend in China. Chin J Prev Med. 2012; 46: 703–7.
18.Lei T, Chen WQ, Zhang SW, Lei TH, Ying Q, He ZY, et al. Prevalence trend of colorectal cancer in 10 cities and counties in China from 1988 to 2002. Chin J Oncol. 2009; 31: 428–33.
19.Li M, Gu J. Changing patterns of colorectal cancer over the recent two decades in China. Chin J Gastrointest Surg. 2004; 7: 214–7.
20.Wei WQ. Esophageal cancer. In: The National Office for Cancer Prevention and Control, National Central Cancer Registry, Disease Prevention and Control Bureau, Ministry of Health of the People's Republic of China, eds. Report of Cancer Death in China-Three National Retrospective Sampling Death Surveys. People’s Health Press: Beijing. 2010; 63-76.
21.Zou XN, Duan JJ, Hufu XM, Chen WQ, Zhao P. Analysis of stomach cancer mortality in the national retrospective sampling survey of death causes in China, 2004-2005. Chin J Prev Med. 2010; 44: 390–7.
22.Xu ZJ, Zheng RS, Zhang SW, Zou XN, Chen WQ. Nasopharyngeal carcinoma incidence and mortality in China in 2009. Chin J Cancer. 2013; 32: 453–60.
23.Wang N, Chen WQ, Zhu WX, Xin XM, Lu AP, Yang L. Incidence trends and pathological characteristics of lung cancer in urban Beijing during period of 1998-2007. Chin J Prev Med. 2011; 45: 249–54.
24.Wang QJ, Zhu WX, Xing XM. Analysis of the incidence and survival of female breast cancer in Beijing during the last 20 years. Chin J Oncol. 2006; 28: 208–10.
25.Zou XN, Lin DM, Wan X, Chao A, Feng QF, Dai Z, et al. Histological subtypes of lung cancer in Chinese males from 2000 to 2012. Biomed Environ Sci. 2014; 27: 3–9.
26.Zou XN, Lin DM, Chao A, Wan X, Feng QF, Li JL, et al. Histological subtypes of lung cancer in Chinese women from 2000 to 2012. Thoracic Cancer. 2014; 5: 447–54.
27.Cao ML, Song FJ, He M, Dong SF, Chen KX. Trends in incidence and mortality of esophageal cancer from 1981 to 2002 in Tianjin. Chin J Dig. 2008; 28: 221–4.
28.Cao Y, Li DF, Chen ZF, Song GH, Hou J, Chen C, et al. 1988-2011 mortality trend of esophageal cancer in Ci county. Chin J Cancer Prev Treat. 2016; 23: 142–5.
29.Zheng Y, Wu CX, Jin F, Gu K, Bao PP, Wang CF, et al. Cancer incidence trends from 1973 to 2005 in Shanghai. J Diagn Concepts Pract. 2009; 8: 25–32.
30.Zheng Y, Li DL, Shen YZ, Xiang YM, Bao PP. Epidemiologic trends and patterns of primary liver cancer in Shanghai. J Surg Concepts Pract. 2004; 9: 292–4.
31.Zhu J, Chen JG, Zhang YH, Chen YS, Ding LL. Trend on mortality changes for lung cancer during 1972-2011 in Qidong, Jiangsu. Chin J Epidemiol. 2012; 33: 933–6.
32.Hu WB, Shi JG, Zhang T, Qin W. Temporal trend analysis of cervical cancer incidence during 2006-2013 in Kunshan, Jiangsu Province. Chin J Cancer Prev Treat. 2015; 22: 1658–61.
33.Zhao Q, He BH. Morbidity and mortality analysis on malignant tumor from 2006 to 2011 in Xiacheng District of Hangzhou city. Shanghai J Prev Med. 2013; 25: 169–72.
34.Li H, Diao YT, Ma JX, Xu AQ, Li HQ, Ma Q, et al. Time trends on the prevalence of cancer during 1970-2005 in Shandong province. Chin J Epidemiol. 2009; 30: 592–5.
35.Yi L, Ma HM, Li YY, Sun YW, Zhao DL, Li XQ, et al. Trend analysis for cancer incidence in rural areas of Feicheng, Shandong province between 2000 and 2012. Chin J Cancer Prev Treat. 2015; 22: 1861–4.
36.You JW, Xie GP. Cancer mortality in the residents of Changle city, Fujian province. Chin J Cancer Prev Treat. 2001; 8: 196–8.
37.Zhang LM, Zhang PQ. Epidemic trend of lung cancer incidence from 1991 to 2010 in Dalian city. Chin J Cancer Prev Treat. 2015; 22: 567–73.
38.Guo ZC, Wei M, Fan HN. Statistical and dynamic analysis of preceding in 30 years on 11975 cases of malignant tumors in Qinghai province. J Qinghai Med College. 2006; 27: 116–8.
39.Luo HZ, Liang XY, Li XJ, Liu XQ. An analysis on incidence rates of cancer in Liang Zhou district of Wu Wei city from 2001 to 2010. Chin Primary Health Care. 2012; 26: 72–5.
40.Duan XZ, Bai PL, Wang SM. Population-based screening of cervical cancer and precancerous lesions among women from eastern area of Inner Mongolia. Chin J Clin Obstet Gynecol. 2012; 13: 190–3.
41.Lu JB, Sun XB, Dai DX, Lian SY, Chang QL, Liu SZ, et al. Prevalence trends of esophageal cancer in Henan in 1974-1999. Chin J Cancer Prev Treat. 2002; 9: 118–20.
42.Wei KR, Liang ZH. Obviously increasing incidence trend for males but stable pathological proportions for both genders: esophageal cancer in Zhongshan of China from 1970-2007. Asian Pacific J Cancer Prev. 2012; 13: 1783–6.
43.Huang TR, Yu JH, Zhang ZQ, Shi JJ, Liu JL, He ZF, et al. Analysis on epidemic feature and secular trend of primary liver cancer in Guangxi. Guangxi Med J. 2000; 22: 677–9.
44.Huang TR, Wei ZL, Wang KB, Liang RX, Zhang ZQ, Deng W. An analysis on morbidity of liver cancer in the period of 1997-2003 in Fushui, Guangxi. Guangxi Med. 2006; 28: 1336–9.
45.Deng W, Long L, Li JL, Zhang D, Yu JH, Zhang CY, et al. Mortality of major cancers in Guangxi, China: sex, age and geographical differences from 1971 and 2005. Asian Pacific J Cancer Prev. 2014; 15: 1567–74.
46.Mao DQ, Feng LG, Pan CB, Wang XL, Wang Q, Zhang CG, et al. Epidemiology and variation trend of the malignant tumor mortality among residents of urban in Chongqing municipal. Chongqing Med. 2009; 38: 1715–7.
47.Zhao M, Zhang JH, Xu XB, Zhang JP, Huang YC. Dynamic analysis of 10331 cases of hospitalized inpatient cases of lung cancer in Yunnan tumor hospital from 2005 to 2014. Chin J Cancer Prev Treat. 2015; 22: 1731–4.
48.Chen JZ, Du HZ, Gu YK, Du XH. From 1969 to 2003 the epidemic tendency analysis of esophageal cancer in Yanting county Sichuan. Sichuan Med J. 2005; 26: 3–4.
49.Li JB, Qiao YL. Exploration of cervical cancer preventive experiences in city–10 years of cervical cancer prevention in Shenzhen. China Cancer. 2015; 24: 971–2.
50.Zhi H, Ou B, Xiao XY, Peng YL, Wang Y, Liu LS, et al. Ultrasound elastography of breast lesions in Chinese women: a multicenter study in China. Clin Breast Cancer. 2013; 13: 392–400.
51.Wang BH, He MF, Chao A, Engelgau MM, Saraiya M, Wang LM, et al. Cervical cancer screening among adult women in China, 2010. Oncologist. 2015; 20: 627–34.
52.Wang GQ, Wei WQ, Hao CQ, Zhang JH, Lü N. Natural progression of early esophageal squamous cell carcinoma. Chin J Oncol. 2010; 32: 600–2.
53.Lu YF, Liu ZC, Li ZH, Ma WH, Wang FR, Zhang YB, et al. Esophageal/gastric cancer screening in high-risk populations in Henan province, China. Asia Pacific J Cancer Prev. 2014; 15: 1419–22.
54.Wang X, Fan JH, Wang XR, Leng Y, Li J, Bao Y, et al. Epidemiology of esophageal cancer in Yanting–regional report of a national screening programme in China. Asian Pacific J Cancer Prev. 2013; 14: 2429–32.
55.Wang ZQ, Zhu D, Tan LR, Song Y, Zhang YJ, Yang F, et al. Analysis of the screening results of esophageal cancer in Bazhong, Sichuan from 2010 to 2013. J Cancer Contr Treat. 2014; 27: 81–4.
56.Huang LJ, Yuan YT, He J, Zhang J, Yan SL, Li XH, et al. Analysis of colorectal screening results in the Haicang district of Xiamen city. Pract Oncol J. 2013; 27: 406–9.
57.Lu ZM, Chen JG, Zhang YX, Wang Q, Xu J, Chen C, et al. Preliminary report about the screening program for colorectal cancer by sequential fecal occult blood in Wuhan area for 4 years. Chin J Gastrointest Surg. 2009; 12: 474–6.
58.Li ZF, Wang SM, Shi JF, Zhao FH, Ma JF, Qiao YL, et al. Combined screening of cervical cancer, breast cancer and reproductive tract infections in rural China. Asian Pacific J Cancer Prev. 2012; 13: 3529–33.
59.Shi ZH, Liao XZ, Xu KK, Zou YH, Zhu SL, Xiao JF, et al. Results of breast cancer screening from 2012 to 2015 in Changsha city, Hunan province, China Cancer. 2015; 24: 1003–6.
60.Wang SL, Shi JC, Gulinuer A, Chen YH, Wang L. Analysis of the results of cervical cancer and breast cancer screening for rural women in Xinjiang in 2012. Chin J Women Child Health Res. 2014; 25: 418–21.
61.Mayineur N, Li L, Chen F, Zhang WH, Zhu KC, Liu XW, et al. epidemiological survey of the relationship between HPV and cervical cancer in Xinjiang Uygur women. Chin Clin Oncol. 2011; 16: 322–5.
62.Tang W, Wu N, Huang Y, Wang J, Zhao J, Zhao S, et al. Results of low-dose computed tomography (LDCT) screening for early lung cancer: prevalence in 4 690 asymptomatic participants. Chin J Oncol. 2014; 36: 549–54.
63.Xie QM, Liu K, Chen S. Early cancer screening and treatment in Changsha, China: assessment for 2012-2013. Chin J Oncol Prev Treat. 2014; 6: 243–6.
64.Li HZ, Du LB, Sun JH, Gao YM, Lv L, Wang XH, et al. An analysis on the result of early detection and treatment of cancer in Zhejiang urban population. Zhejiang Prev Med. 2015; 27: 1189–93.
Cite this article as:Zou X. Epidemic trend, screening, and early detection and treatment of cancer in Chinese population. Cancer Biol Med. 2017; 14: 50-9. doi: 10.20892/j.issn.2095-3941.2016.0047
Xiao-Nong Zou
E-mail: xnzou@cicams.ac.cn
Received June 6, 2016; accepted July 18, 2016. Available at www.cancerbiomed.org
Copyright © 2017 by Cancer Biology & Medicine
 Cancer Biology & Medicine2017年1期
Cancer Biology & Medicine2017年1期
- Cancer Biology & Medicine的其它文章
- Overdiagnosis of breast cancer in population screening: does it make breast screening worthless?
- Epidemiology of ovarian cancer: a review
- Epidemiology, etiology, and prevention of esophageal squamous cell carcinoma in China
- DNA methylation assay for colorectal carcinoma
- Association of genotypes of rs671 within ALDH2 with risk for gastric cardia adenocarcinoma in the Chinese Han population in high- and low-incidence areas
- A pilot study of radiologic measures of abdominal adiposity: weighty contributors to early pancreatic carcinogenesis worth evaluating?
