Epidemiology, etiology, and prevention of esophageal squamous cell carcinoma in China
He Liang, Jin-Hu Fan, You-Lin Qiao
Department of Cancer Epidemiology, National Cancer Center/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing 100021, China
Epidemiology, etiology, and prevention of esophageal squamous cell carcinoma in China
He Liang, Jin-Hu Fan, You-Lin Qiao
Department of Cancer Epidemiology, National Cancer Center/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing 100021, China
Esophageal cancer is one of the most fatal diseases worldwide mainly because of its rapid progression and poor prognosis. Although the incidence of esophageal adenocarcinoma has markedly risen in North America and Europe in the past several decades, esophageal squamous cell carcinoma is still the predominant subtype of esophageal cancer, especially in China. It accounts for more than 90% of all esophageal squamous cell carcinoma cases in China. Geographical differentiation is one of the most distinctive characteristics of esophageal cancer. The progression, risk factors, and prognosis of these two subtypes of esophageal cancer differ. This study reviews the epidemiology, etiology, and prevention of esophageal squamous cell carcinoma in China, thereby providing systematic references for policy-makers who will decide on issues of esophageal cancer prevention and control.
Epidemiology; etiology; prevention; esophageal squamous cell carcinoma; review
Introduction
Esophageal cancer is the eighth most common cancer worldwide, with approximately 456,000 new cases in 2012 (3.2%); it is the sixth most common cause of cancer-related death, with an estimated 400,000 cases (4.9%)1. Approximately 80% of the new cases occur in less developed regions in the world, and 60% of these cases occur in China2. Esophageal adenocarcinoma and esophageal squamous cell carcinoma (ESCC) are the two major histological sub-types of esophageal cancer. Esophageal adenocarcinoma has become the predominant type of esophageal cancer in North America and Europe, especially among white men3, whereas ESCC is the predominant subtype in China (more than 90% of the total number of esophageal cancer cases)4. The striking geographical variation implies that environmental and genetic factors play important roles in the development of esophageal cancer.
The incidence and mortality of esophageal cancer in China
Esophageal cancer is the fifth most frequently diagnosedcancer and the fourth leading cause of death from cancer in China, with estimated 286,700 new cases and 211,000 deaths in 2012, according to the National Central Cancer Registry5. In China, incidence is generally higher among males and in rural areas. Age-specific incidence and mortality increase with age. The incidence of esophageal cancer before the age of 40 is relatively low but increases rapidly after the age of 40 (Figure 1). The mortality of esophageal cancer before the age of 45 is also relatively low and increases rapidly after the age of 50 (Figure 2) and peaks between the ages of 80 and 85.
The incidence of esophageal cancer has been steady in recent decades and in most countries. The incidence among males in Asia has generally declined, whereas the incidence slightly increased in Europe. The increasing female incidence rate is lower than in males, especially among people of ages >45 years old. Data provided by National Central Cancer Registry show that age-adjusted incidence rate decreases from 15.93/100,000 to 10.01/100,000 from 2000 to 2011 in China6, particularly in the high-risk areas7,8. From 2000 to 2011, age-adjusted mortality rate decreased from 12.69/100,000 to 7.55/100,000. Age-adjusted mortality rate has dramatically decreased across the three National Retrospective Sampling Survey of Death Causes (1973-1975, 1990-1992 and 2004-2005). Primary prevention, such as lifestyle modification, secondary prevention, such as screening, and improved medical level, may be the main cause for the decline of esophageal cancer incidence in China.
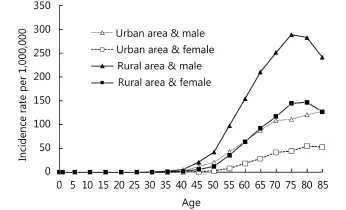
Figure 1 Age-adjusted incidence rates for esophageal cancer according to region and gender in China, 2012.
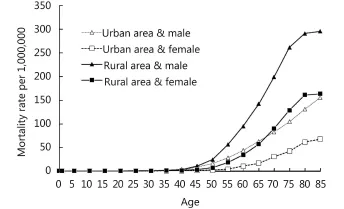
Figure 2 Age-adjusted mortality for esophageal cancer according to regions and gender in China, 2012.
The incidence and mortality of esophageal cancer are also affected by geography. The greatest burden of ESCC occurs in the “Asian Esophageal Cancer Belt,” which extends from northern Iran, east to China, and north to Russia, presents an estimated ESCC of more than 100 cases/100,000 personyears9. The third national census of cancer shows evident regional differences in the incidence of esophageal cancer in China. Provinces with a high incidence of esophageal cancer were Hebei, Henan, Fujian, and Chongqing, followed by Xinjiang, Jiangsu, Shanxi, Gansu, and Anhui10. Provinces with higher rates, where near the Taihang Mountains, and the highest incidence of esophageal and cardiac carcinoma were in Linxian, Henan Province, where esophageal and cardiac carcinoma accounted for 81.4% of all malignant tumors in the region. More than 90% of esophageal patients in China are ESCCs; thus, we focus on ESCC in this review.
Risk factors of ESCC
Smoking and drinking

Figure 3 Trends in incidence rates (ASR) for esophageal cancer in China from 2000 to 2011.

Figure 4 Trends in mortality rates (ASR) for esophageal cancer in China from 2000 to 2011.
According to Die, Nutrition, and the Prevention of Chronic Diseases (WHO, 1990), “epidemiological studies make it clear that drinking and esophageal cancer are related, and smoking can also cause esophageal cancer.” Smoking and alcohol drinking are the main risk factors for ESCC in Western countries, and the risk of ESCC increases by threefold to sevenfold for smokers compared with nonsmokers11. Tobacco smoking is classified by the International Agency for Research on Cancer (IARC) as a cause of esophageal cancer12. Compared with non-alcohol drinkers, ESCC risk increases by 38%, 260%, and 550% among those who drink 1–1.5 units of alcohol per day, 1.5–6 units of alcohol per day, and 6+ units of alcohol per day, respectively13,14. In addition, reports pointed out that smoking and alcohol drinking exert a synergistic effect on ESCC risk. A meta-analysis showed that the combined effect of drinking and smoking is almost double the sum of their effects individually15. However, another meta-analysis showed that the effect of smoking on ESCC is considerably higher in Asian populations than in Western populations. In a prospective study of risk factors for ESCC in Linxian, China, smoking and alcohol drinking were not significantly associated with the more significant risk factors of long-termESCC risk, which is not consistent with results of previous studies in other areas in the world16.
Diet
Lack of fresh fruit and vegetables
In several observational studies, non-frequent consumption of fresh fruits and vegetables is closely associated with a higher risk of ESCC17-21. However, in that report, no distinction was made between ESCC and esophageal adenocarcinoma. A meta-analysis that included several prospective studies suggested that eating fruits and vegetables is significantly associated with reduction in ESCC risk22. A recent population-based case-control study in a rural China population showed that compared with the lowest quartile, the highest quartile of the vegetable and fruit intake was associated with a reduction of ESCC risk by 30%23.
Hot beverage and pickled vegetables
Consumption of high-temperature drinks and pickled vegetables (traditional Asian style) are classified by the World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) as a possible cause of esophageal cancer based on limited evidence. A meta-analysis showed that the consumption of hot food and beverages is associated with an increased risk of esophageal cancer, particularly ESCC24. Several observations indicated that the consumption of hot beverages increased the burden of ESCC among Africans25. A study in China showed that consuming hot and extremely hot beverages rapidly increased the risk of ESCC significantly among the Chinese population26. Eating pickles and sauerkraut was once popular topics in esophageal cancer high-risk studies, and these foods were considered high-risk factors. In addition, another study in China showed that subjects who consumed pickled foods had a 1.76-fold increased risk of ESCC compared with subjects who did not consume pickled foods27. Fungi in pickles induce animal cancer28. However, epidemiological studies on this topic remain controversial.
Red meat, processed meat, and hot maté
Based on limited evidence, consumption of red meat, processed meat, and hot maté has been classified by WCRF/ AICR as a possible cause of esophageal cancer. A metaanalysis showed that ESCC risk is 57% higher in people who consume high amount of red meat and 55% higher in people who consume processed meat compared with those with low meat consumption29. A meta-analysis showed that ESCC risk is 2.6 times higher in maté drinkers versus non-drinkers30. However, a pooled analysis of case-control studies found that the risk of ESCC only increased by 60%31.
Micronutrient deficiency
Deficiency of several vitamins/minerals is proven to be closely associated with high ESCC incidence; the most pronounced effect is observed in developing countries. Several studies revealed the effect of micronutrients, such as beta-carotene, folate, vitamin C, and vitamin E, on ESCC risk32-34. Plasma riboflavin levels are significantly related to the risk and prognosis of ESCC patients, thereby suggesting that moderate supplementation of riboflavin will decrease risk, prevent recurrence of ESCC, and improve the prognosis of ESCC patients35. The Nutrition Intervention Trial that has been conducted among the general population in Linxian showed that consumption of the compound capsule of vitamin B2 and nicotinic acid decreased the incidence of esophageal cancer by 14%. Experimental results show that βcarotene, vitamin E, and selenium intake can reduce esophageal cancer mortality by 17% (RR 0.83, 95% CI: 0.71–0.98) in people less than 55 years old and can also reduce total mortality and mortality caused by stomach cancer; the main type of esophageal cancer is ESCC in this study36. Selenium and zinc nutritional statuses were also inversely related to ESCC risk in China37,38.
Chemical factors
High doses of polycyclic aromatic hydrocarbons (PAH) and nitrosamine exposure may cause ESCC in a high-risk region. In Northeast Iran, two studies reported the urinary levels of a PAH metabolite that indicated exposure to PAH in >41% of the individuals tested39. Studies in Brazil and China presented similar results. Nitrosamine is a broad-action carcinogen, and its precursors are nitrate nitrogen, nitrite nitrogen, and secondary amines that exist in air, water, and food. The amount of nitrite amine in drinking water and food is higher in high-risk than in low-risk regions40. After the interaction of NMBzA (a common carcinogen in Linxian) with human fetal esophageal epithelium transplanted into the mesentery of nude mice, squamous cell carcinoma, (including Alu sequence in humans) appeared in the draft site. NMBzA can induce human ESCC; and result of this study is considered the most conclusive evidence of nitrite amine as a contributor to the etiology of ESCC in Linxian country41.
Infections
The association between HPV infection and ESCC remainscontroversial. A recent systematic review of the relationship between HPV infection (types 16 and 18) and esophageal cancer worldwide found that HPV is closely associated with esophageal cancer in China, and in other countries, with an integrated OR=1.62 (95% CI: 1.33–1.98)42. The highest HPV prevalence was found in Africa and Asia; notably, this result was obtained among Chinese studies from provinces with high ESCC incidence rates43. However, three consecutive studies demonstrated that HPV infections are independent of ESCC44-46. A large prospective study does not support the major role for HPV 16, HPV 18, and HPV 73 in the etiology of ESCC. In a high-risk area in China, the infection of esophageal cells with high-risk HPV types occurs in 13% of asymptomatic adults with no evidence of squamous dysplasia and a similar proportion of individuals with mild, moderate, or severe dysplasia. The relationship between ESCC and HPV still requires further validation.
Family history of esophageal cancer
Esophageal cancer presents significant family aggregation. ESCC risk may be higher in people with a positive family history of esophageal cancer47. In a large population-based case-control study, strong association between a family history of esophageal cancer and the risk of ESCC was found. The risk of ESCC increased with increasing number of affected relatives. In particular, cases of both parents being affected render an eightfold risk of ESCC for their offspring48. Previous epidemiological studies conducted in endemic areas (including mainly Linxian and Shanxi) in China demonstrated that individuals with a family history of esophageal cancer present a higher risk of such cancer49,50. However, a multicenter population-based case-control study performed in the United States did not find any familial link for ESCC51. A Swedish case-control study also revealed no association between a history of esophageal cancer in firstdegree relatives and the risk of ESCC52.
Genetic changes
Previous epidemiological studies showed familial aggregation of the disease in families and higher frequency of allelic loss in ESCC cases with a positive family history. The genetic and environmental interactions may play a certain crucial role in ESCC progression53,54. In addition, evidence has shown that RNA expression differs by family history status and that 152 genes present different expression patterns between persons with positive versus a negative family history of upper gastrointestinal cancer55. The current etiology of esophageal cancer genetics has made substantial achievements in molecular theory, but these findings still need validation through clinical trials. Exome sequencing has been conducted on 113 tumor-normal pairs and has yielded a mean of 82 non-silent mutations per tumor and eight cell lines. The mutational profile closely resembles those of squamous cell carcinomas of other tissues but differs from that of esophageal adenocarcinoma56. Whole-genome and whole-exome sequencing in Chinese patients with ESCC identified eight significantly mutated genes; among these genes, six are well-known tumor-associated genes (TP53, RB1, CDKN2A, PIK3CA, NOTCH1, and NFE2L2), and two are novel genes in ESCC (ADAM29 and FAM135B)57. Three genome-wide association studies examined ESCC, and two subsequent analyses used combinations of these three studies to report as many as 12 loci associated with ESCC risk. A locus in the HLA class II region at 6p21.32 (rs35597309) achieved genome-wide significance in the two populations at the highest risk for ESSC58.
Other factors
Socioeconomic status (SES) was associated with a higher risk of ESCC in both low- and high-risk areas worldwide59. A study in Taixing, China, comparing different SES indicators and composite wealth scores found an inverse association between low SES and ESCC60. The poor nutritional status of the Linxian population in 1984, as reflected by the dietary data and the low BMI record in study16, is a serious matter. Efforts to improve diet, particularly the availability of a greater variety of affordable foods, continue to be a public health priority in Linxian. These efforts to improve the SES of the Linxian population are likely to exert substantial beneficial effects on the health of the people living in the area, and these effects may already be evident in recent reports, which suggested a decline in the rates of ESCC in this area61.
Several epidemiological studies have reported an increased risk of ESCC or its precursor lesions in those with poor oral hygiene16. Studies from China in the 1970s led to the hypothesis that high risk of ESCC could also result from poor oral health, poor oral hygiene practices, or tooth loss40. Recently, a study in China showed that toothbrushing exerts protective effects against ESCC and that tooth loss is associated with an elevated risk for ESCC62. Furthermore, in South America, Europe, and Japan, case-control studies have shown that tooth loss can increase the risk of ESCC63. However, the association between ESCC with poor oral hygiene and tooth loss can be confounded by other related factors, such as low SES, smoking, and drinking.
Prevention and screening
ESCC is a common cancer worldwide with a poor prognosis because of the lack of symptoms at early stages. Most patients are diagnosed too late for curative treatment. In China, the survival rate is less than 10% when diagnosed at an advanced stage but can be as high as 85% if detected at an earlier stage64. The mortality of ESCC can be reduced through identifying modifiable risk factors and reducing the exposure to these factors (primary prevention) or early diagnosis of precancerous lesions and early cancer treatment (secondary prevention).
Etiological studies still cannot verify which factors play a dominant role in the pathogenesis of esophageal cancer, and the targeted prevention and control measures for primary prevention are deficient. As with other chronic diseases, for the primary prevention strategies for ESCC, we strongly recommend for people to eliminate risk factors, such as quitting alcohol, drinking, and smoking, increasing the consumption of vegetables and fruits, reducing nitrosamine and its precursor PAH intake, and changing lifestyle.
At present, no international specification or recommendation for esophageal cancer screening, early diagnosis, and treatment is available. Countries with a high prevalence of ESCC have initiated screening programs because early detection is associated with better outcomes. Similar to all population-based screening programs, screening for the early detection of ESCC must be costeffective. Endoscopy with iodine (Lugol’s solution) staining of the esophageal mucosa, known as chromoendoscopy, is the gold standard for the diagnosis of abnormal esophageal mucosal lesions in studies from Korea, Japan, and China. However, this method may be too expensive and invasive in several high-risk communities. Therefore, Iran utilizes nonendoscopic methods. Several new endoscopic imaging modalities, such as narrow-band imaging, cannot be used inappropriately at the population level because of its questionable validity and cost-effectiveness for large populations65-68.
Since the 1970s, several screening methods have been developed and tested in the high-risk areas of China, such as balloon cytology with smears69-72, liquid-based balloon cytology73, occult blood detection74,75, and endoscopic examination with iodine staining and biopsy76,77. Studies have indicated that endoscopy with iodine staining and indicative biopsy can increase the sensitivity and specificity ofesophageal cancer screening. A population-based prospective cohort study with buffer regions control in Cixian showed a reduction in cumulative incidence, the risk of further cancer, and cumulative mortality. Risk was reduced by 29.47%, 39%, 33.56%, and 55% in the intervention group versus control group after a 10-year follow-up period among > 45,000 people aged 40–69 years old78. This study is the first in the world to demonstrate that the use of endoscopic screening with iodine staining can reduce incidence and mortality of esophageal cancer in high-risk areas. This study provides scientific evidence for the early diagnosis and treatment of upper gastrointestinal disease in high-risk areas in China.

Table 1 Screening strategy of esophageal cancer in high-risk areas of China
China presents a high incidence of esophageal cancer, especially in rural areas. Over the past half-century, many cancer studies have been carried out in these high-risk areas. Based on domestic and international research and transfer of“the early diagnosis and treatment of cancer” program in China, endoscopic iodine staining and biopsy have been recommended in areas with a high incidence of esophageal cancer. For patients (40–60 years old) in areas with high incidence rate of esophageal cancer, the screening and treatment of early abnormal lesions prevent progression to esophageal cancer. All lesions were diagnosed on the basis of histopathological examination (Table 1)79. The program of screening and the early diagnosis and treatment of esophageal cancers are effective in high-risk areas in China. In non-high risk areas, this large-scale population screening is not aligned with China's national conditions. In non-high risk urban areas, a high-risk population assessment may be carried out. Screening of high-risk groups may be more costeffective. However, this method needs to be verified in more cohort studies.
Conclusions
The treatment and prevention of esophageal squamous cell carcinoma are among the most important public health issues in China. During the last three decades, socioeconomic development, medical level improving, lifestyle changing and screening, and mortality from esophageal cancer decreased in China. However, the burden of this fatal disease is considerable due to the immense scale of the Chinese population. Effective preventive actions, such as health education, nutritional intervention, and screening, should be enhanced, especially in high-risk areas.
Conflict of interest statement
1.International Agency for Research on Cancer. GLOBOCAN 2012, Estimated Cancer Incidence, Mortality and Prevalence Worldwide in 2012. Geneva: World Health Organization, 2012.
2.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: Globocan 2008. Int J Cancer. 2010; 127: 2893–917.
3.Enzinger PC, Mayer RJ. Esophageal cancer. N Engl J Med. 2003; 349: 2241–52.
4.Zhao J, He YT, Zheng RS, Zhang SW, Chen WQ. Analysis of esophageal cancer time trends in China, 1989–2008. Asian Pac J Cancer Prev. 2012; 13: 4613–7.
5.Chen WQ, Zheng RS, Zhang SW, Zeng HM, Zuo TT, Jia MM, et al. Report of cancer incidence and mortality in China, 2012. China Cancer. 2015; 25: 1–8.
6.Zuo TT, Zheng RS, Zeng HM, Zhang SW, Chen WQ, He J. Incidence and trend analysis of esophageal cancer in China. Chin J Oncol. 2016; 38: 703–8.
7.Sun XB, Liu ZC, Liu SZ, Li BY, Dai DX, Quan PL, et al. Descriptive analysis of incidence and time trends of esophageal and gastric cancers in Linzhou City. Chin J Oncol. 2007; 29: 764–7.
8.Chen ZF, Song GH, Hou J, Chen C, Qiao CY, Ji HX, et al. Esophageal and gastric cancer incidence trend in Cixian from 1988 to 2007. Chin J Clin Oncol. 2011; 38: 839–42.
9.Glenn TF. Esophageal cancer. Facts, figures, and screening. Gastroenterol Nurs. 2001; 24: 271–3; quiz 274–5.
10.Zhou MG, Wang XF, Hu JP, Li GL, Chen WQ, Zhang SW, et al. Geographical distribution of cancer mortality in China, 2004–2005. Chin J Prev Med. 2010; 44: 303–8.
11.Kamangar F, Chow WH, Abnet CC, Dawsey SM. Environmental causes of esophageal cancer. Gastroenterol Clin North Am. 2009; 38: 27–57.
12.International Agency for Research on Cancer, volumes 1 to 105⋆. List of Classifications by Cancer Sites with Sufficient or Limited Evidence in Humans July, 2014.
13.Bagnardi V, Rota M, Botteri E, Tramacere I, Islami F, Fedirko V, et al. Light alcohol drinking and cancer: A meta-analysis. Ann Oncol. 2013; 24: 301–8.
14.Islami F, Fedirko V, Tramacere I, Bagnardi V, Jenab M, Scotti L, et al. Alcohol drinking and esophageal squamous cell carcinoma with focus on light-drinkers and never-smokers: A systematic review and meta-analysis. Int J Cancer. 2011; 129: 2473–84.
15.Prabhu A, Obi KO, Rubenstein JH. The synergistic effects of alcohol and tobacco consumption on the risk of esophageal squamous cell carcinoma: A meta-analysis. Am J Gastroenterol. 2014; 109: 822–7.
16.Tran GD, Sun XD, Abnet CC, Fan JH, Dawsey SM, Dong ZW, et al. Prospective study of risk factors for esophageal and gastric cancers in the Linxian general population trial cohort in china. Int J Cancer. 2005; 113: 456–63.
17.Freedman ND, Park Y, Subar AF, Hollenbeck AR, Leitzmann MF, Schatzkin A, et al. Fruit and vegetable intake and esophageal cancer
No potential conflicts of interest are disclosed.in a large prospective cohort study. Int J Cancer. 2007; 121: 2753–60.
18.Launoy G, Milan C, Day NE, Pienkowski MP, Gignoux M, Faivre J. Diet and squamous-cell cancer of the oesophagus: A French multicentre case-control study. Int J Cancer. 1998; 76: 7–12.
19.Jessri M, Rashidkhani B, Hajizadeh B, Jacques PF. Adherence to mediterranean-style dietary pattern and risk of esophageal squamous cell carcinoma: A case-control study in Iran. J Am Coll Nutr. 2012; 31: 338–51.
20.Steevens J, Schouten LJ, Goldbohm RA, van den Brandt PA. Vegetables and fruits consumption and risk of esophageal and gastric cancer subtypes in the Netherlands Cohort Study. Int J Cancer. 2011; 129: 2681–93.
21.Vingeliene S, Chan DSM, Aune D, Vieira AR, Polemiti E, Stevens C, et al. An update of the WCRF/AICR systematic literature review on esophageal and gastric cancers and citrus fruits intake. Cancer Causes Control. 2016; 27: 837–51.
22.Liu J, Wang J, Leng Y, Lv CX. Intake of fruit and vegetables and risk of esophageal squamous cell carcinoma: A meta-analysis of observational studies. Int J Cancer. 2013; 133: 473–85.
23.Liu XD, Wang XR, Lin SH, Lao XQ, Zhao J, Song QK, et al. Dietary patterns and the risk of esophageal squamous cell carcinoma: A population-based case-control study in a rural population. Clin Nutr. 2015. Doi: 10.1016/j.clnu.2015.11.009.
24.Andrici J, Eslick GD. Hot food and beverage consumption and the risk of esophageal cancer: A meta-analysis. Am J Prev Med. 2015; 49: 952–60.
25.McCormack VA, Menya D, Munishi MO, Dzamalala C, Gasmelseed N, Leon Roux M, et al. Informing etiologic research priorities for squamous cell esophageal cancer in Africa: A review of setting-specific exposures to known and putative risk factors. Int J Cancer. 2017; 140: 259–71.
26.Wu M, Liu AM, Kampman E, Zhang ZF, Van't Veer P, Wu DL, et al. Green tea drinking, high tea temperature and esophageal cancer in high- and low-risk areas of Jiangsu Province, China: A population-based case-control study. Int J Cancer. 2009; 124: 1907–13.
27.Wang QZ, Zhou XB, Teng HS. Meta-analysis on the relationship between dietary factors and esophageal neoplasm in China. Bull Chin Cancer. 2007; 16: 3–7.
28.Rossini ARAL, Hashimoto CL, Iriya K, Zerbini C, Baba ER, Moraes-Filho JPP. Dietary habits, ethanol and tobacco consumption as predictive factors in the development of esophageal carcinoma in patients with head and neck neoplasms. Dis Esophagus. 2008; 21: 316–21.
29.Choi Y, Song S, Song Y, Lee JE. Consumption of red and processed meat and risk for esophageal squamous cell carcinoma based on a meta-analysis. World J Gastroenterol. 2013;19: 1020-9.
30.Andrici J, Eslick GD. Maté consumption and the risk of esophageal squamous cell carcinoma: A meta-analysis. Diseases of the esophagus: official journal of the International Society for Dis Esophagus. 2013; 26: 807–16.
31.Lubin JH, De Stefani E, Abnet CC, Acosta G, Boffetta P, Victora C, et al. Maté drinking and esophageal squamous cell carcinoma in South America: Pooled results from two large multicenter casecontrol studies. Cancer Epidemiol Biomarkers Prev. 2014; 23: 107–16.
32.Galeone C, Pelucchi C, Levi F, Negri E, Talamini R, Franceschi S, et al. Folate intake and squamous-cell carcinoma of the oesophagus in italian and swiss men. Ann Oncol. 2006; 17: 521–5.
33.Aune D, Deneo-Pellegrini H, Ronco AL, Boffetta P, Acosta G, Mendilaharsu M, et al. Dietary folate intake and the risk of 11 types of cancer: A case-control study in uruguay. Ann Oncol. 2011; 22: 444–51.
34.World Cancer Research Fund/American Institute For Cancer Research. Food, Nutrition, Physical Activity and the Prevention of Cancer: A Global Perspective. Washington, DC: AICR, 2007.
35.Li SS, Xu YW, Wu JY, Tan HZ, Wu ZY, Xue YJ, et al. Plasma riboflavin level is associated with risk, relapse, and survival of esophageal squamous cell carcinoma. Nutr Cancer. 2016; 69: 21–8.
36.Qiao YL, Dawsey SM, Kamangar F, Fan JH, Abnet CC, Sun XD, et al. Total and cancer mortality after supplementation with vitamins and minerals: Follow-up of the Linxian general population nutrition intervention trial. J Natl Cancer Inst. 2009; 101: 507–18.
37.Lin YS, Totsuka Y, He YT, Kikuchi S, Qiao YL, Ueda J, et al. Epidemiology of esophageal cancer in Japan and China. J Epidemiol. 2013; 23: 233–42.
38.Li PW, Xu JM, Shi Y, Ye Y, Chen K, Yang J, et al. Association between zinc intake and risk of digestive tract cancers: A systematic review and meta-analysis. Clin Nutr. 2014; 33: 415–20.
39.Kamangar F, Strickland PT, Pourshams A, Malekzadeh R, Boffetta P, Roth MJ, et al. High exposure to polycyclic aromatic hydrocarbons may contribute to high risk of esophageal cancer in northeastern Iran. Anticancer Res. 2005; 25: 425–8.
40.Yang CS. Research on esophageal cancer in china: A review. Cancer Res. 1980; 40: 2633–44.
41.Lu SH, Chui SX, Yang WX, Hu XN, Guo LP, Li FM. Relevance of n-nitrosamines to oesophageal cancer in China. IARC Sci Publ. 1991; 11–7.
42.Wang J, Zhao L, Yan H, Che JJ, Huihui L, Jun W, et al. A metaanalysis and systematic review on the association between human papillomavirus (types 16 and 18) infection and esophageal cancer worldwide. PLoS One. 2016; 11: e0159140.
43.Petrick JL, Wyss AB, Butler AM, Cummings C, Sun X, Poole C, et al. Prevalence of human papillomavirus among oesophageal squamous cell carcinoma cases: Systematic review and metaanalysis. Br J Cancer. 2014; 110: 2369–77.
44.Kamangar F, Qiao YL, Schiller JT, Dawsey SM, Fears T, Sun XD, et al. Human papillomavirus serology and the risk of esophageal and gastric cancers: Results from a cohort in a high-risk region in China. Int J Cancer. 2006; 119: 579–84.
45.Gao GF, Roth MJ, Wei WQ, Abnet CC, Chen F, Lu N, et al. No association between HPV infection and the neoplastic progression of esophageal squamous cell carcinoma: Result from a crosssectional study in a high-risk region of China. Int J Cancer. 2006; 119: 1354–9.
46.Lu SX, Luo FQ, Li HC. Detection of human papilloma virus in esophageal squamous cell carcinoma and adjacent tissue specimens in Linxian. Chinese J Oncol. 1995; 17: 321–4.
47.Ji JG, Hemminki K. Familial risk for esophageal cancer: An updated epidemiologic study from Sweden. Clin Gastroenterol Hepatol. 2006; 4: 840–5.
48.Chen TT, Cheng HW, Chen XD, Yuan ZY, Yang XR, Zhuang MQ, et al. Family history of esophageal cancer increases the risk of esophageal squamous cell carcinoma. Sci Rep. 2015; 5: 16038.
49.Gao Y, Hu N, Han XY, Giffen C, Ding T, Goldstein A, et al. Family history of cancer and risk for esophageal and gastric cancer in Shanxi, China. BMC Cancer. 2009; 9: 269.
50.Hu N, Dawsey SM, Wu M, Bonney GE, He LJ, Han XY, et al. Familial aggregation of oesophageal cancer in Yangcheng County, Shanxi Province, China. Int J Epidemiol. 1992; 21: 877–82.
51.Dhillon PK, Farrow DC, Vaughan TL, Chow WH, Risch HA, Gammon MD, et al. Family history of cancer and risk of esophageal and gastric cancers in the united states. Int J Cancer. 2001; 93: 148–52.
52.Lagergren J, Ye WM, Lindgren A, Nyren O. Heredity and risk of cancer of the esophagus and gastric cardia. Cancer Epidemiol Biomarkers Prev. 2000; 9: 757–60.
53.Hu N, Roth MJ, Emmert-Buck MR, Tang ZZ, Polymeropolous M, Wang QH, et al. Allelic loss in esophageal squamous cell carcinoma patients with and without family history of upper gastrointestinal tract cancer. Clin Cancer Res. 1999; 5: 3476–82.
54.Qu Y, Zhang S, Cui L, Wang K, Song C, Wang P, et al. Two novel polymorphisms in PLCE1 are associated with the susceptibility to esophageal squamous cell carcinoma in Chinese population. Dis Esophagus. 2016;
55.Su H, Hu N, Shih J, Hu Y, Wang QH, Chuang EY, et al. Gene expression analysis of esophageal squamous cell carcinoma reveals consistent molecular profiles related to a family history of upper gastrointestinal cancer. Cancer Res. 2003; 63: 3872–6.
56.Gao YB, Chen ZL, Li JG, Hu XD, Shi XJ, Sun ZM, et al. Genetic landscape of esophageal squamous cell carcinoma. Nat Genet. 2014; 46: 1097–102.
57.Song YM, Li L, Ou YW, Gao ZB, Li EM, Li XC, et al. Identification of genomic alterations in oesophageal squamous cell cancer. Nature. 2014; 509: 91–5.
58.Wu C, Wang ZM, Song X, Feng XS, Abnet CC, He J, et al. Joint analysis of three genome-wide association studies of esophageal squamous cell carcinoma in Chinese populations. Nat Genet. 2014; 46: 1001–6.
59.Blot WJ, McLaughlin JK, Fraumeni JF. Esophageal cancer. In: Schottenfeld D, Fraumeni JF, editors. Cancer Epidemiology and Prevention. New york: Oxford University Press; 2006. p.697–706.
60.Zhang L, Cheng HW, Zhou YC, Yuan ZY, Chen TT, Chen XD, et al. Association between socioeconomic status and esophageal squamous cell carcinoma in the population of Taixing area, Jiangsu province. Chin J Epidemiol. 2014; 35: 147–50.
61.Ke L. Mortality and incidence trends from esophagus cancer in selected geographic areas of China circa 1970–90. Int J Cancer. 2002; 102: 271–4.
62.Chen XD, Yuan ZY, Lu M, Zhang YC, Jin L, Ye WM. Poor oral health is associated with an increased risk of esophageal squamous cell carcinoma - a population-based case-control study in China. Int J Cancer. 2017; 140: 626–35.
63.Guha N, Boffetta P, Wünsch Filho V, Eluf Neto J, Shangina O, Zaridze D, et al. Oral health and risk of squamous cell carcinoma of the head and neck and esophagus: Results of two multicentric casecontrol studies. Am J Epidemiol. 2007; 166: 1159–73.
64.Wang GQ, Jiao GG, Chang FB, Fang WH, Song JX, Lu N, et al. Long-term results of operation for 420 patients with early squamous cell esophageal carcinoma discovered by screening. Ann Thor Surg. 2004; 77: 1740–4.
65.Choi KS, Jun JK, Park EC, Park S, Jung KW, Han MA, et al. Performance of different gastric cancer screening methods in Korea: A population-based study. PLoS One. 2012; 7: e50041.
66.Yokoyama A, Ohmori T, Makuuchi H, Maruyama K, Okuyama K, Takahashi H, et al. Successful screening for early esophageal cancer in alcoholics using endoscopy and mucosa iodine staining. Cancer. 1995; 76: 928–34.
67.Ide E, Carneiro FOAA, Frazão MSV, Chaves DM, Sallum RAA, de Moura EGH, et al. Endoscopic detection of early esophageal squamous cell carcinoma in patients with achalasia: Narrow-band imaging versus lugol's staining. J Oncol. 2013; 2013: 736756.
68.Roshandel G, Nourouzi A, Pourshams A, Semnani S, Merat S, Khoshnia M. Endoscopic screening for esophageal squamous cell carcinoma. Arch Iran Med. 2013; 16: 351–7.
69.Shu YJ. Cytopathology of the esophagus. An overview of esophageal cytopathology in China. Acta Cytol. 1983; 27: 7–16.
70.Shen O, Wang DY, Liu SF, Cao J, Zhou B, Cao SG, et al. Cytologic screening for esophageal cancer: Results from 12, 877 subjects from a high-risk population in China. Int J Cancer. 1993; 54: 185–8.
71.Dawsey SM, Shen Q, Nieberg RK, Liu SF, English SA, Cao J, et al. Studies of esophageal balloon cytology in Linxian, China. Cancer Epidemiol Biomarkers Prev. 1997; 6: 121–30.
72.Roth MJ, Liu SF, Dawsey SM, Zhou B, Copeland C, Wang GQ, et al. Cytologic detection of esophageal squamous cell carcinoma and precursor lesions using balloon and sponge samplers in asymptomatic adults in Linxian, China. Cancer. 1997; 80: 2047–59.
73.Pan QJ, Roth MJ, Guo HQ, Kochman ML, Wang GQ, Henry M, et al. Cytologic detection of esophageal squamous cell carcinoma and its precursor lesions using balloon samplers and liquid-based cytology in asymptomatic adults in Linxian, China. Acta Cytol. 2008; 52: 14–23.
74.Qin DX, Wang GQ, Zuo JH, Zhang XH, Yuan FL, Li MS, et al. Screening of esophageal and gastric cancer by occult blood bead detector. Cancer. 1993; 71: 216–8.
75.Qin DX, Wang GQ, Yuan FL, Tang MZ, Li MS, Zhang ZL. Screening for upper digestive tract cancer with an occult blood bead detector investigation of a normal North China population. Cancer. 1988; 62: 1030–4.
76.Dawsey SM, Wang GQ, Weinstein WM, Lewin KJ, Liu FS, Wiggett S, et al. Squamous dysplasia and early esophageal cancer in thelinxian region of China: Distinctive endoscopic lesions. Gastroenterology. 1993; 105: 1333–40.
77.Dawsey SM, Lewin KJ, Liu FS, Wang GQ, Shen Q. Esophageal morphology from Linxian, China. Squamous histologic findings in 754 patients. Cancer. 1994; 73: 2027–37.
78.Wei WQ, Chen ZF, He YT, Feng H, Hou J, Lin DM, et al. Longterm follow-up of a community assignment, one-time endoscopic screening study of esophageal cancer in China. J Clin Oncol. 2015; 33: 1951–7.
79.Dong ZW. Technical plan for early detection and treatment of cancer screening in China. Beijing: Peking University Medical Press. 2009;45-85.
Cite this article as: Liang H, Fan J, Qiao Y. Epidemiology, etiology, and prevention of esophageal squamous cell carcinoma in China. Cancer Biol Med. 2017; 14: 33-41. doi: 10.20892/j.issn.2095-3941.2016.0093
Jin-Hu Fan and You-Lin Qiao
E-mail: fanjh@cicams.ac.cn and qiaoy@cicams.ac.cn
Received November 10, 2016; accepted December 23, 2016. Available at www.cancerbiomed.org
Copyright © 2017 by Cancer Biology & Medicine
 Cancer Biology & Medicine2017年1期
Cancer Biology & Medicine2017年1期
- Cancer Biology & Medicine的其它文章
- Erratum to Bcl-2 expression is a poor predictor for hepatocellular carcinoma prognosis of andropause-age patients
- Metformin prevents hormonal and metabolic disturbances and 1,2-dimethylhydrazine-induced colon carcinogenesis in non-diabetic rats
- Truth telling for patients with esophageal squamous cell carcinoma in Henan, China
- Roles of Rap1 signaling in tumor cell migration and invasion
- Estimation of lung cancer burden in Australia, the Philippines, and Singapore: an evaluation of disability adjusted life years
- A pilot study of radiologic measures of abdominal adiposity: weighty contributors to early pancreatic carcinogenesis worth evaluating?
