多囊卵巢综合征患者血清血管内皮生长因子、内皮抑素水平及对卵巢间质血流的影响研究
刘梅梅,丁 慧,尹晓静,王 珊,于彩虹,李肖肖
·论著·
多囊卵巢综合征患者血清血管内皮生长因子、内皮抑素水平及对卵巢间质血流的影响研究
刘梅梅1*,丁 慧2,尹晓静2,王 珊2,于彩虹2,李肖肖2
目的 探讨多囊卵巢综合征(PCOS)患者血清血管内皮生长因子(VEGF)、内皮抑素(ES)水平及对卵巢间质血流的影响。方法 选取2014年7月—2015年9月在哈尔滨医科大学附属第二医院生殖中心就诊的PCOS患者96例作为PCOS组;选取同期因男方因素不孕而就诊于本院生殖中心的健康女性72例作为对照组。PCOS组根据稳态模型评价的胰岛素抵抗指数(HOMA-IR),分为PCOS胰岛素抵抗组(PCOS-IR组,n=47)和PCOS非胰岛素抵抗组(PCOS-NIR组,n=49)。采用酶联免疫吸附法测定所有受试者血清中的VEGF、ES水平。同时所有患者于卵泡早期应用经阴道彩色多普勒超声监测双侧卵巢间质血流,并计算出血流动力学参数:搏动指数(PI)和阻力指数(RI)。结果 PCOS-NIR、PCOS-IR组VEGF、ES水平高于对照组,PI、RI低于对照组,差异有统计学意义(P<0.05);PCOS-IR组VEGF、ES水平高于PCOS-NIR组,PI、RI低于PCOS-NIR组,差异有统计学意义(P<0.05)。PCOS患者VEGF水平与黄体生成素(LH)、睾酮(T)水平及LH/促卵泡刺激素(FSH)、HOMA-IR呈直线正相关(P<0.05),与PI、RI呈直线负相关(P<0.05);ES水平与LH、T水平及LH/FSH无直线相关性(P>0.05),而与PI、RI呈直线负相关(P<0.05),与HOMA-IR及VEGF水平呈直线正相关(P<0.05)。PCOS患者PI、RI与LH、T水平及LH/FSH、HOMA-IR均呈直线负相关(P<0.05)。多元线性回归分析结果显示,T、VEGF水平及HOMA-IR是PCOS患者PI的影响因素(P<0.05);LH、T、VEGF水平及HOMA-IR是PCOS患者RI的影响因素(P<0.05)。结论 VEGF、ES在PCOS患者血清中呈高表达,二者之间呈直线正相关且均与PCOS患者的HOMA-IR密切相关,同时VEGF的表达水平还与血清LH、T水平密切相关;VEGF与ES的表达失衡及HOMA-IR在PCOS卵巢间质血流异常增多中起主要作用。
多囊卵巢综合征;血管内皮生长因子类;内皮抑素类;卵巢间质血流
刘梅梅,丁慧,尹晓静,等.多囊卵巢综合征患者血清血管内皮生长因子、内皮抑素水平及对卵巢间质血流的影响研究[J].中国全科医学,2017,20(4):448-453.[www.chinagp.net]
LIU M M,DING H,YIN X J,et al.Serum levels of vascular endothelial growth factor and endostatin of patients with polycystic ovary syndrome and their effects on ovarian stromal blood flow[J].Chinese General Practice,2017,20(4):448-453.
多囊卵巢综合征(polycystic ovary syndrome,PCOS)是一种病因不明、临床表现极为复杂的内分泌代谢紊乱综合征,在育龄期女性中发病率为5%~10%[1]。卵巢排卵障碍、高雄激素及卵巢多囊样改变是PCOS的三大主要症状,同时还可伴有高胰岛素血症、胰岛素抵抗、肥胖、多毛、不孕及2型糖尿病、心血管疾病高发等特征[1]。研究表明PCOS患者卵巢血管生成异常及间质血流增加[2],因此血管生成失调可能是PCOS发生发展的主要原因之一[3-4]。血管内皮生长因子(vascular endothelial growth factor,VEGF)是目前已知调节血管生成最关键的因素之一,其可促进血管内皮细胞的增殖并调节血管通透性[3]。内皮抑素(endostatin,ES)为VEGF的拮抗因子,能选择性作用于血管内皮细胞抑制内皮细胞的生长,抑制新血管的形成[5]。有研究发现PCOS患者VEGF、ES水平异常升高[3,5],但二者的相关性及与PCOS卵巢间质血流的关系尚不明确。本研究拟通过检测PCOS患者血清中VEGF、ES水平,结合超声下监测卵巢间质血流变化,探讨VEGF、ES对PCOS患者卵巢间质血流的影响。
1 对象与方法
1.1 研究对象 选取2014年7月—2015年9月在哈尔滨医科大学附属第二医院生殖中心就诊的PCOS患者96例作为PCOS组;选取同期因男方因素不孕而就诊于本院生殖中心的健康女性72例作为对照组。PCOS组纳入标准:均符合2003年鹿特丹国际会议制定的诊断标准[6]:(1)稀发排卵或无排卵;(2)高雄激素的临床表现和/或高雄激素血症;(3)超声检查显示卵巢多囊性改变,即单侧或双侧卵巢直径2~9 mm的卵泡≥12个,和/或卵巢容积≥10 ml,同时具备以上3项或2项并排除其他高雄激素病因者即可确诊。对照组纳入标准:(1)因男方不育因素就诊的生育期女性,平素月经规律,无PCOS临床表现;(2)内分泌激素水平正常,超声下子宫及双侧卵巢无异常改变及其他盆腔病变。两组排除标准:(1)全身炎性疾病、甲状腺疾病、高泌乳素血症、肾上腺疾病、高血压、糖尿病等合并症;(2)近6个月内服用过激素类药物。PCOS组根据稳态模型评价的胰岛素抵抗指数(homeostasis model assessment-insulin resistance index,HOMA-IR),分为PCOS胰岛素抵抗组(PCOS-IR组,n=47)和PCOS非胰岛素抵抗组(PCOS-NIR组,n=49)。本研究经本院伦理委员会批准,受试者均被告知本研究的大致流程及意义,并签署知情同意书。
1.2 方法
1.2.1 资料收集 所有受试者于就诊当日记录其年龄,测量其身高及体质量,并计算BMI。
1.2.2 性激素测定 所有受试者于卵泡早期(月经周期第2~4天)或闭经2个月以上,超声检查无优势卵泡,晨起空腹抽取外周静脉血进行性激素测定:黄体生成素(luteinizing hormone,LH)、促卵泡刺激素(follicle stimulating hormone,FSH)、雌二醇(estradiol,E2)、孕激素(progesterone,P)、泌乳素(prolactin,PRL)、睾酮(total testosterone,T),并将余下血清留存于-20 ℃冰箱中备用。本研究以T>0.48 μg/L界定为高雄激素血症。
1.2.3 卵巢间质血流测定 于采血当日经阴道彩色多普勒超声监测患者双侧卵巢间质血流,计算并记录血流指数:搏动指数(pulsatility index,PI)和阻力指数(resistance index,RI)。所有受试者卵巢间质血流的监测均由同一人完成,每侧卵巢间质血流重复量取3次并取其平均值,同时由于患者左、右侧卵巢间质血流间无明显差异,故取所有受试者左、右侧卵巢间质血流的平均值。
1.2.4 葡萄糖耐量试验(oral glucose tolerance test,OGTT)及胰岛素释放试验(insulin releasing test,IRT) 试验 所有受试者于禁食8 h后,分别于8:00及口服75 g葡萄糖粉后30、60、120 min抽取肘部静脉血,测定血清葡萄糖水平及胰岛素水平,并计算HOMA-IR。HOMA-IR=(空腹血糖×空腹胰岛素)/22.5,以HOMA-IR≥2.69为PCOS-IR组,HOMA-IR<2.69为PCOS-NIR组。
1.2.5 血清VEGF、ES水平测定 取上述备用血清,采用酶联免疫吸附法,按试剂盒说明书要求检测所有受试者血清中VEGF、ES水平。

2 结果
2.1 3组受试者年龄、BMI及性激素水平比较 3组受试者年龄、BMI及FSH、E2、P、PRL水平间差异无统计学意义(P>0.05),而LH、T水平及LH/FSH间差异有统计学意义(P<0.05,见表1)。
2.2 3组受试者PI、RI、HOMA-IR及VEGF、ES水平比较 3组受试者PI、RI、HOMA-IR及VEGF、ES水平间差异均有统计学意义(P<0.05,见表2)。
2.3PCOS患者VEGF、ES水平与其他指标的相关性分析PCOS患者VEGF水平与LH、T水平及LH/FSH、HOMA-IR呈直线正相关(P<0.05),与PI、RI呈直线负相关(P<0.05);ES水平与LH、T水平及LH/FSH无直线相关性(P>0.05),而与PI、RI呈直线负相关(P<0.05),与HOMA-IR及VEGF水平呈直线正相关(P<0.05,见表3)。
2.4PCOS患者PI、RI与其他相关指标的相关性分析PCOS患者PI、RI与LH、T水平及LH/FSH、HOMA-IR均呈直线负相关(P<0.05,见表4)。
2.5PCOS患者卵巢间质血流影响因素的多元线性回归分析 分别以PI、RI为因变量,以LH、LH/FSH、T、HOMA-IR、VEGF、ES为自变量进行多元线性回归分析,结果显示,T、VEGF水平及HOMA-IR是PCOS患者PI的影响因素(P<0.05);LH、T、VEGF水平及HOMA-IR是PCOS患者RI的影响因素(P<0.05,见表5)。
表2 3组受试者PI、RI、HOMA-IR及VEGF、ES水平比较
Table2ComparisonofPI,RI,HOMA-IRandVEGFaswellasESlevelsinthethreegroups
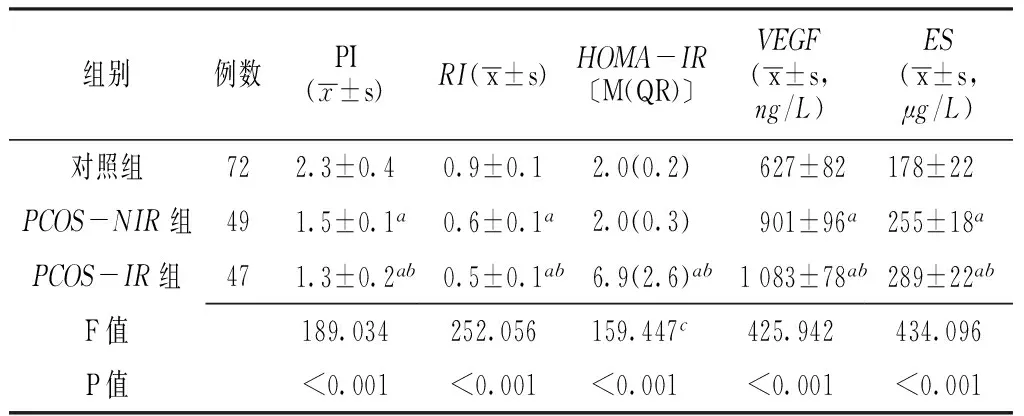
组别例数PI(x±s)RI(x±s)HOMA-IR〔M(QR)〕VEGF(x±s,ng/L)ES(x±s,μg/L)对照组722.3±0.40.9±0.12.0(0.2) 627±82178±22PCOS-NIR组491.5±0.1a0.6±0.1a2.0(0.3) 901±96a255±18aPCOS-IR组471.3±0.2ab0.5±0.1ab6.9(2.6)ab1083±78ab289±22abF值189.034252.056159.447c425.942434.096P值<0.001<0.001<0.001<0.001<0.001
注:与对照组比较,aP<0.05;与PCOS-NIR组比较,bP<0.05,c为经对数转换后进行单因素方差分析;PI=搏动指数,RI=阻力指数,HOMA-IR=稳态模型评价的胰岛素抵抗指数,VEGF=血管内皮生长因子,ES=内皮抑素

表1 3组受试者年龄、BMI及性激素水平比较±s)
注:与对照组比较,aP<0.05;与PCOS-NIR组比较,bP<0.05;LH=黄体生成素,FSH=促卵泡刺激素,E2=雌二醇,P=孕激素,PRL=泌乳素,T=睾酮,PCOS=多囊卵巢综合征,PCOS-IR组=PCOS胰岛素抵抗组,PCOS-NIR组=PCOS非胰岛素抵抗组
表3 PCOS患者VEGF、ES水平与其他指标的相关性分析
Table 3 Correlation analysis of VEGF,ES levels and other indicators of PCOS patients
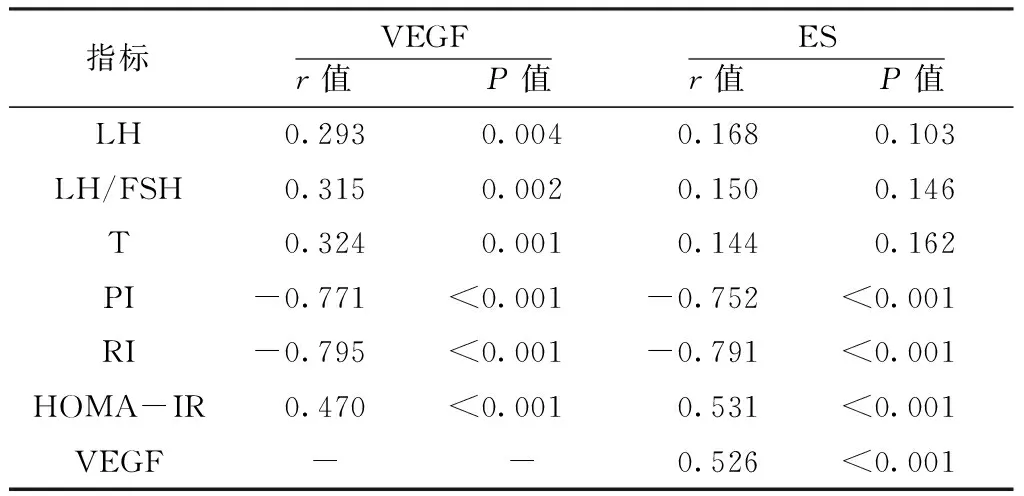
指标VEGFr值 P值ESr值 P值LH0.2930.0040.1680.103LH/FSH0.3150.0020.1500.146T0.3240.0010.1440.162PI-0.771<0.001-0.752<0.001RI-0.795<0.001-0.791<0.001HOMA-IR0.470<0.0010.531<0.001VEGF--0.526<0.001
注:-代表与自身不进行相关分析
表4 PCOS患者PI、RI与其他相关指标的相关性分析
Table 4 Correlation analysis of PI,RI and other indicators of PCOS patients
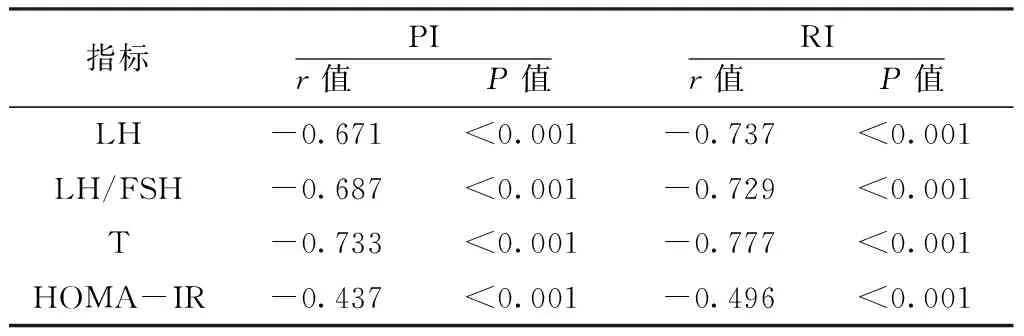
指标PIr值 P值RIr值 P值LH-0.671<0.001-0.737<0.001LH/FSH-0.687<0.001-0.729<0.001T-0.733<0.001-0.777<0.001HOMA-IR-0.437<0.001-0.496<0.001
表5 PCOS患者卵巢间质血流影响因素的多元线性回归分析
Table 5 Multiple linear regression of the influencing factors of ovarian stromal blood flow
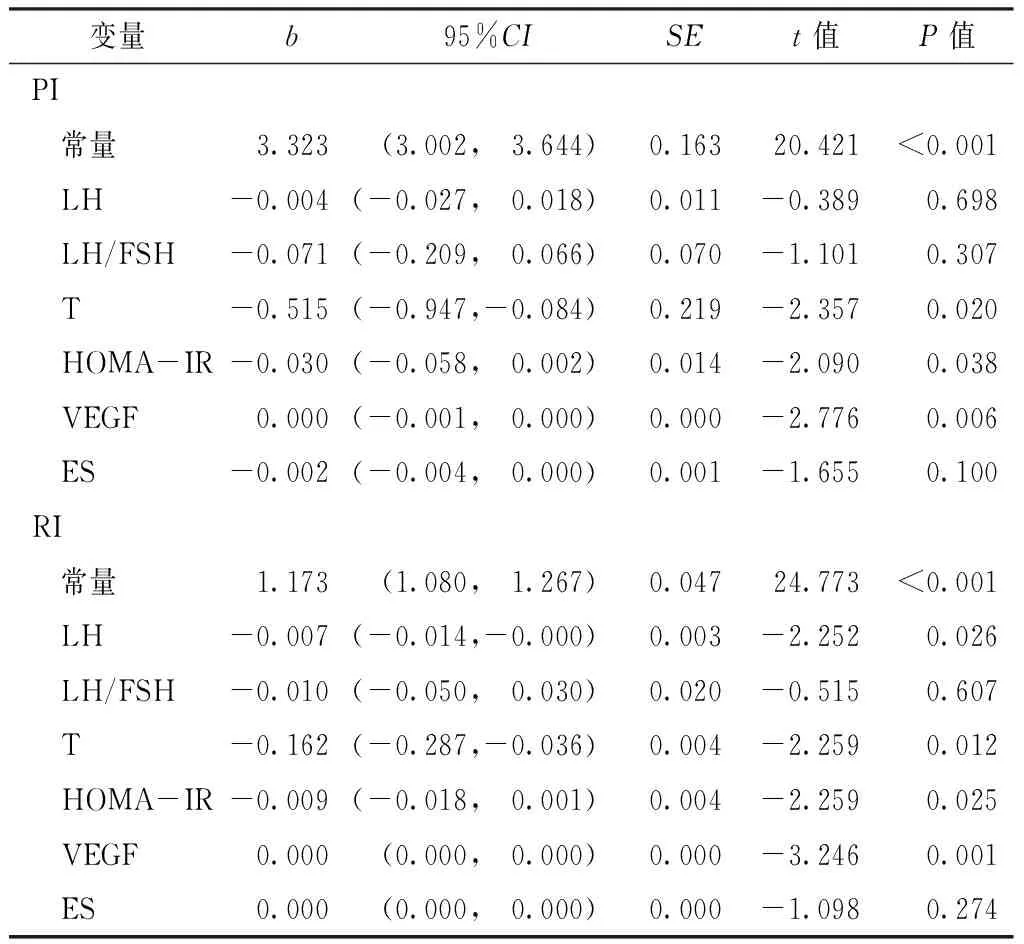
变量b95%CISEt值P值PI 常量3.323(3.002, 3.644)0.16320.421<0.001 LH-0.004(-0.027, 0.018)0.011-0.3890.698 LH/FSH-0.071(-0.209, 0.066)0.070-1.1010.307 T-0.515(-0.947,-0.084)0.219-2.3570.020 HOMA-IR-0.030(-0.058, 0.002)0.014-2.0900.038 VEGF0.000(-0.001, 0.000)0.000-2.7760.006 ES-0.002(-0.004, 0.000)0.001-1.6550.100RI 常量1.173(1.080, 1.267)0.04724.773<0.001 LH-0.007(-0.014,-0.000)0.003-2.2520.026 LH/FSH-0.010(-0.050, 0.030)0.020-0.5150.607 T-0.162(-0.287,-0.036)0.004-2.2590.012 HOMA-IR-0.009(-0.018, 0.001)0.004-2.2590.025 VEGF0.000(0.000, 0.000)0.000-3.2460.001 ES0.000(0.000, 0.000)0.000-1.0980.274
3 讨论
3.1 PCOS卵巢间质血流变化 卵巢组织的血流灌注随着卵泡的发育及激素水平的周期性变化而呈现相应的周期性改变,这对卵泡的发育、排卵及后续黄体的形成及退化有着至关重要的作用[7]。PI、RI是反映卵巢动脉血流阻力的血流动力学参数,其值越低表明卵巢间质血流的灌注越丰富。本研究结果显示,PCOS患者卵泡期卵巢间质血流较健康女性明显增多,表现为RI、PI值的明显降低,超声下显示卵巢间质血流丰富、波峰较为圆钝,呈高速低阻力型,这与其他学者的研究结果相一致[1-2,8]。有报道称PCOS患者卵巢间质血流的变化与体内的高LH、T及胰岛素水平相关[9],本研究结果与其一致,即PI、RI与PCOS患者血清LH、T水平及HOMA-IR呈直线负相关,还与LH/FSH呈直线负相关。由此表明,PCOS卵巢间质血流的异常灌注与机体内分泌紊乱密切相关,其可能是PCOS发生排卵障碍的重要原因。血管异常生成与调节血管生成的各细胞因子密切相关。本研究结果显示,PCOS患者血清中的促血管生成因子VEGF与抑制血管生成因子ES均呈高表达,并与卵巢间质血流丰富程度相一致,且二者的表达与HOMA-IR呈直线正相关,而VEGF作为一主要因素与卵巢间质血流密切相关。由此本研究认为PCOS患者卵巢间质血流异常灌注与其血清中血管因子的表达失衡及机体的胰岛素抵抗状态具有相关性。
3.2 VEGF与PCOS VEGF为一种高效促血管生成因子,通过酪氨酸激酶受体产生作用,促进血管内皮细胞分裂,使组织血管生成增加[10]。有研究认为女性生殖系统是体循环中VEGF的主要来源,其可维持卵泡周围血流,通过增加毛细血管的通透性使血浆蛋白外渗导致卵巢基质增大影响卵泡的发育与成熟[11-12]。本研究结果显示,PCOS患者血清VEGF水平明显升高,并与卵巢间质血流RI、PI呈直线负相关,这与以往的研究结论相一致[11]。另外,本研究结果显示,VEGF水平与LH、T水平呈直线正相关,这与部分研究结果相吻合[12],而AGRAWAL等[13]却认为其三者之间并无相关性。有研究发现VEGF mRNA的动态表达模式与LH相平行[14],高水平的LH可加强胰岛素样生长因子-1在PCOS患者中促VEGF合成的作用[15]。而高水平的雄激素可作用于颗粒细胞导致卵巢分泌VEGF增加[16]。当给予PCOS患者腹腔镜下卵巢打孔术后,伴随着血清LH、T水平的明显下降,VEGF也明显降低,卵巢间质血流明显改善[12],说明VEGF具有一定的激素依赖性。另有报道称VEGF在PCOS患者卵巢颗粒细胞和间质细胞中也呈高表达,并与卵巢间质血流的增加相一致[11,17]。据此本研究推测PCOS患者血清VEGF水平的升高在一定程度上解释了超声下所显示的卵巢多囊样改变及间质高度血管化,增加的血管也可能是由卵巢过度表达VEGF刺激所致。
3.3 ES与PCOS ES是一种特异性的抑血管生成因子,其主要通过促进内皮细胞凋亡、抑制血管内皮增殖及血管内皮细胞的迁移等途径有效抑制新生血管的形成[18]。本研究结果显示,PCOS患者血清ES水平明显升高,并与RI、PI呈直线负相关,由此间接证明了PCOS患者存在血管生成增多的状态。本研究结果还显示,ES的表达与HOMA-IR呈直线正相关。胰岛素具有刺激血管内皮细胞活动的作用,其能增加血清中内皮素、VEGF的水平,促使肾素-血管紧张素-醛固酮系统(renin-angiotensin-aldosterone system,RAAS)过度活跃,导致脂肪组织合成激素及细胞因子发生异常[3,19]。这可能是导致PCOS患者血清ES表达增高的一个重要原因。近期,有学者对高脂饮食诱导的肥胖小鼠模型研究发现,给予ES治疗后小鼠胰岛素抵抗及糖耐量受损的代谢紊乱状态得到明显改善,并认为这可能与ES的抑血管生成及抗脂肪形成有关[20]。这更充分地证实了ES在PCOS病理生理中的重要作用,也有望成为治疗PCOS的新途径。
3.4 VEGF与ES 有研究提示ES能够阻断VEGF通路所促成的血管形成作用,特异性抑制血管内皮细胞的增殖[21]。ES还能抑制内皮细胞一氧化氮(NO)合酶(eNOS)的磷酸化,诱使eNOS失活,明显减少VEGF 诱导的NO合成,从而抑制VEGF介导的血管新生和血管通透性的增加[22]。本研究结果显示,PCOS患者血清ES水平与VEGF水平呈直线正相关,表明二者在调节血管形成方面有着重要相关性。由于异常升高的VEGF促进机体血管生成,为维持内环境稳定,大量的血管生成抑制剂ES代偿性分泌以抗衡高水平的血管生成趋势,故而导致ES在PCOS患者机体内明显增多。但这种代偿作用并不能使机体内环境达到正常生理状态,最终可能因调节失衡导致卵巢间质异常血管化及血流灌注的增加。
此外,血清VEGF、ES水平均与HOMA-IR呈直线正相关。由此本研究推测高胰岛素血症对PCOS卵巢间质异常的血管生成有一定的影响,这与其他学者的观点一致[11,19]。有研究发现PCOS患者接受二甲双胍治疗后,血清VEGF表达水平明显下降,卵巢间质血流明显减少[4,23]。DI等[4]对PCOS大鼠模型研究发现卵巢组织中VEGF呈高表达,血管密度增加;经二甲双胍治疗后,伴随着大鼠体内的胰岛素水平的下降,VEGF也明显降低,卵巢间质血管密度下降。研究结果说明胰岛素抵抗可能对PCOS患者血管因子的异常表达有着重要影响。
4 小结
本研究发现VEGF、ES在PCOS患者血清中呈高表达,并均与HOMA-IR呈直线正相关,且与卵巢间质血流的增加相平行。由此推测血管生成调节异常与PCOS卵巢间质血流的异常化具有直接相关性,可能是PCOS发生排卵障碍及代谢紊乱的病因之一。虽然目前卵巢间质血流灌注异常并未纳入PCOS的诊断标准,但弄清血管生成调节障碍在PCOS卵巢间质血流的异常变化中的具体机制,抗血管生成治疗有望成为其新的治疗靶点。
作者贡献:刘梅梅为本研究课题的第一负责人,提供了具体的试验方法及试验步骤,并参与文章的部分撰写及后续的修改、审校与质量控制;丁慧主要负责本试验大部分数据的收集与整理、统计学分析及文章初稿的撰写;尹晓静、王珊、于彩虹、李肖肖参与本试验所涉及的血清学指标的检测、小部分临床试验数据的收集及部分试验数据的统计学分析。
本文无利益冲突。
[1]OZDEMIR O,SARI M E,KALKAN D,et al.Comprarison of ovarian stromal blood flow measured by color Doppler ultrasonography in polycystic ovary syndrome patients and healthy women with ultrasonographic evidence of polycystic[J].Gynecol Endocrinol,2015,31(4):322-326.
[2]ALCAZAR J L,KUDLA M J.Ovarian stromal vessels assessed by spatiotemporal image correlation high definition flow in women with polycystic ovary syndrome:a case-control study[J].Ultrasound Obstet Gynecol,2012,40(4):470-475.
[3]TAL R,SEIFER D B,ARICI A.The emerging role of angiogenic factor dysregulation in the pathogenesis of polycystic ovarian syndrome[J].Semin Reprod Med,2015,33(3):195-207.
[4]DI PIETRO M,PARBORELL F,IRUSTA G,et al.Metformin regulates ovarian angiogenesis and follicular development in a female polycystic ovary syndrome rat model[J].Endocrinology,2015,156(4):1453-1463.
[5]周青,彭朝龙,肖帆,等.PCOS患者卵巢组织中VEGF、ES的表达变化及意义[J].山东医药,2011,51(30):9-10. ZHOU Q,PENG C L,XIAO F,et al.Expression change and significance of VEGF and ES in ovarians of polycystic ovarian syndrome[J].Shandong Medicine Journal,2011,51(30):9-10.
[6]Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group.Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome[J].Fertil Steril,2004,81(1):19-25.
[7]QIN J J,LIU Y L,LIN M H,et al.Ovarian interstitial blood flow changes assessed by transvaginal color Doppler sonography:predicting ovarian endometrioid cyst-induced injury to ovarian interstitial vessels[J].Arch Gynecol obstet,2012,285(2):427-433.
[8]BATTAGLIA C,BATTAGLIA B,MOROTTI E,et al.Two-and three-dimensional sonographic and color Doppler techniques for diagnosis of polycystic ovary syndrome.The stromal/ovarian volume ratio as a new diagnostic criterion[J].J Ultrasound Med,2012,31(7):1015-1024.
[9]CARMINA E,LONGO A,LOBO R A.Does ovarian blood flow distinguish between ovulatory and anovulatory patients with polycystic ovary syndrome? [J].Am J Obstet Gynecol,2003,189(5):1283-1286.
[10]FERRARA N,DAVIS-SMYTH T.The biology of vascular endothelial growth factor[J].Endocr Rev,1977,18(1):4-25.
[11]ABD EI AAL D E,MOHAMED S A,AMINE A F,et al.Vascular endothelial growth factor and insulin-like growth factor-1 in polycystic ovary syndrome and their relation to ovarian blood flow[J].Eur J Obstet Gynecol Reprod Biol,2005,118(2):219-224.
[12]EI BEHERY M M,DIAB A E,MOWAFY H,et al.Effect of laparoscopic ovarian drilling on vascular endothelial growth factor and ovarian stromal blood flow using 3-dimensional power Doppler[J].Int J Gynaecol Obstet,2011,112(2):119-121.
[13]AGRAWAL R,SLADKEVICIUS P,ENGMANN L,et al.Serum vascular endothelial growth factor concentrations and ovarian stromal blood flow are increased in women with polycystic ovaries[J].Hum Reprod,1998,13(3):651-655.
[14]GEVA E,JAFFE R B.Role of vascular endothelia growth factor in ovary physiology and pathology[J].Fertil Steril,2000,74(3):429-438.
[15]BABITHA V,YADA V,CHOUHAN V S.Luteinizing hormone,insulin like growth factor-1,and epidermal growth factor stimulate vascular endothelial growth factor production in cultured bubaline granulosa cells[J].Gen Comp Endocrinol,2014,198:1-12.
[16]TROPEA A,LANZONE A,TIBERI F,et al.Estrogens and androgens affect human luteal cell function[J].Fertil Steril,2010,94(6):2257-2263.
[17]STANEK M B,BORMAN S M,MOLSKNESS T A.Insulin and insulin-like growth factor stimulation of vascular endothelial growth factor production by luteinized granulosa cells:comparison between polycystic ovarian syndrome(PCOS) and non-PCOS women[J].J Clin Endocrinol Metab,2007,92(7):2726-2733.
[18]王韧,侯立军.VEGF和内皮抑素对血管生成作用的研究进展[J].重庆医学,2011,40(25):2582-2584. WANG R,HOU L J.The advance of VEGF and endostatin effect on angiogenesis[J].Chongqing Medicine,2011,40(25):2582-2584.DOI:10.3969lj.issn.1671-8348,2011.25.042.
[19]MANCINI F,CIANCIOSI A,REGGIANI G M,et al.Endothelial function and its relationship to leptin,homocystenine,and insulin resistance in lean and overweight eumenorrheic women and PCOS patients:a pilot study[J].Fertil Steril,2009,91(6):2537-2544.
[20]WANG H,CHEN Y,LU X A,et al.Endostatin prevents dietary-induced obesity by inhibiting adipogenesis and angiogenesis[J].Diabetes,2015,64(7):2442-2456.
[21]DIGTYAR A V,POZDNYAKOVA N V,FELDMAN N B,et al.Endostatin:current concepts about its biological role and mechanisms of action[J].Biochemistry(Mosc),2007,72(3):235-246.
[22]HAJITOU A,GRIGNCT C,DEVY L,et al.The antitumoral effect of endostatin and angiostatin is associated with a down-regulation of vascular endothelial growth factor expression in tumor cells[J].FASEB J,2003,16(3):1802-1804.
[23]KOCER D,BAYRAM F,DIRI H.The effects of metformin on endothelial dysfunction,lipid metabolism and oxidative stress in women with polycystic ovary syndrome[J].Gynecol Endocrinol,2014,30(5):367-371.
(本文编辑:崔沙沙)
Serum Levels of Vascular Endothelial Growth Factor and Endostatin of Patients with Polycystic Ovary Syndrome and Their Effects on Ovarian Stromal Blood Flow
LIUMei-mei1*,DINGHui2,YINXiao-jing2,WANGShan2,YUCai-hong2,LIXiao-xiao2
1.DepartmentofObstetricsandGynecology,theSecondAffiliatedHospitalofHarbinMedicalUniversity,Harbin150086,China2.TheSecondClinicalCollegeofHarbinMedicalUniversity,Harbin150086,China
Objective To discuss the serum levels of vascular endothelial growth factor(VEGF) and endostatin(ES) of patients with polycystic ovary syndrome(PCOS),and their effects on ovarian stromal blood flow.Methods A total of 96 patients with PCOS,who sought medical treatment in the reproductive center of the Second Affiliated Hospital of Harbin Medical University from July 2014 to September 2015,were selected as PCOS group;72 healthy women who came to our hospital due to male infertility at the same time were selected as the control group.According to the insulin resistance index of homeostasis model assessment(HOMA-IR),PCOS group was divided into PCOS insulin resistance group(PCOS-IR group,n=47)and PCOS non-insulin resistance group(PCOS-NIR group,n=49).The serum level of VEGF and ES of all the participants were measured by enzyme linked immunosorbent assay(ELISA) method.The bilateral ovarian stromal blood flow at early follicular phase of all the patients was detected by transvaginal color doppler ultrasound,the hemodynamic parameters including pulsatility index(PI) and resistance index(RI) were calculated.Results The levels of VEGF and ES in PCOS-NIR and PCOS-IR groups were significantly higher than those in the control group(P<0.05);while their PI and RI were significantly lower than those in the control group(P<0.05);the levels of VEGF and ES in PCOS-IR groups were significantly higher than those in the PCOS-NIR group(P<0.05);while PI and RI were significantly lower than those in the PCOS-NIR group(P<0.05).The level of VEGF of PCOS patients was linearly positively correlated with the level of luteinizing hormone(LH),testosterone(T) and LH/ follicle-stimulating hormone(FSH) and HOMA-IR(P<0.05),and was linearly negatively correlated with PI and RI(P<0.05).There was no significant linear correlation between ES levels and LH,T levels as weel as LH/FSH(P>0.05),but ES levels were linearly negatively correlated with PI and RI(P<0.05) and linearly positively correlated with HOMA-IR and VEGF level(P<0.05).PI and RI of PCOS patients were linearly negatively correlated with levels of LH,T,as well as LH/FSH and HOMA-IR(P<0.05).Multiple linear regression analysis revealed that the levels of T,VEGF and HOMA-IR were the influencing factors of PI of PCOS patients(P<0.05).The levels of LH,T,VEGF and HOMA-IR were the influencing factors of RI of PCOS patients(P<0.05).Conclusion VEGF and ES are highly expressed in the serum of PCOS patients,and there was a positive linear correlation between them.VEGF and ES are closely related with HOMA-IR.The expression level of VEGF is also correlated with serum levels of LH and T.The imbalance of expression of VEGF and ES and HOMA-IR play an important role in the abnormal increasing of PCOS ovarian stromal blood flow.
Polycystic ovary syndrome;Vascular endothelial growth factors;Endostatins;Ovarian stromal blood flow
黑龙江省自然科学基金资助项目(H201392)
R 711.75
A
10.3969/j.issn.1007-9572.2017.04.014
2016-09-12;
2016-12-22)
1.150086黑龙江省哈尔滨市,哈尔滨医科大学附属第二医院妇产科
2.150086黑龙江省哈尔滨市,哈尔滨医科大学第二临床医学院
*通信作者:刘梅梅,副教授,硕士生导师;E-mail:mm7723@163.com
*Correspondingauthor:LIUMei-mei,Associateprofessor,Mastersupervisor;E-mail:mm7723@163.com

