急性冠状动脉综合征患者治疗后出血的相关因素分析
牛光美 郑容梅
[摘 要] 目的:探讨急性冠状动脉综合征(Acute coronary syndrome,ACS)患者治疗后出血的相关因素,为预防出血提供参考。方法:对我科收治的955例ACS患者进行回顾性分析,按照其治疗后出血发生情况分为出血组、未出血组,统计出血发生率,比较两组患者临床资料并归纳影响ACS患者治疗后合并出血的相关因素,探讨防治策略。结果:955例患者中,共有48例患者发生治疗后出血,发生率为5.03%。Logistic多因素回归分析示,年龄≥65岁、非ST段抬高型心肌梗死、既往出血事件、既往CABG手术史、合并肾衰、合并心衰、合并血小板减少、接受氯吡格雷治疗、接受糖蛋白Ⅱb/Ⅲa受体拮抗剂治疗是影响ACS患者治疗后合并出血的独立危险因素。结论:ACS患者治疗后合并出血发生风险较高,年龄、既往史、合并症、治疗方案均可影响出血事件发生率,应早期评估患者出血风险,制定个体化治疗方案。
[关键词] 急性冠状动脉综合征;出血;影响因素
中图分类号:R541.4 文献标识码:B 文章编号:2095-5200(2016)06-021-03
DOI:10.11876/mimt201606008
Analysis on correlation factors of hemorrhage after treatment in patients with acute coronary syndrome NIU Guangmei,ZHENG Rongmei. (Department of cardiologyThe,Third People,s Hospital of Guangyuan,Guangyuan 628400 China)
[Abstract] Objective: This study aimed to investigate the related factors of hemorrhage in patients with acute coronary syndrome (ACS) after treatment, and to provide reference for the prevention of bleeding. Methods: 955 cases of patients with ACS were retrospectively analyzed, and divided into bleeding group and non-bleeding group according to the occurrence of bleeding after treatment, bleeding incidence was stastically analyzed, clinical data were compared between the two groups, the related factors influencing the hemorrhage of ACS patients after treatment, and the prevention and treatment strategies were discussed. Results: Among 955 patients, there were 48 patients with hemorrhage after treatment, the incidence rate was 5.03%. Logistic regression analysis showed that age more than 65 years old, non-ST-elevation myocardial infarction, previous bleeding, previous coronary artery bypass grafting surgery (CABG) surgery, complicated with renal failure, heart failure and thrombocytopenia, accepting clopidogrel therapy and glycoprotein II b/ III a receptor antagonist therapy were independent risk factors of the hemorrhage after treatment of ACS patients. Conclusions: There is high risk bleeding incidence in ACS patients after treatment, age, past history, complication, treatment therapy affect the incidence of bleeding events, the risks of hemorrhage in ACS patients should be early assessed for making individualized treatment decisions.
[Key words] acute coronary syndrome; hemorrhage; influencing factors
急性冠状动脉综合征(Acute coronary syndrome,ACS)发病率及死亡率均处于较高水平,在全球范围内造成了极大的医学及社会经济负担[1]。经皮冠脉介入治疗(Percutaneous coronary intervention,PCI)可通过重新开放狭窄甚至闭塞的冠脉管腔,改善心肌血流灌注,在近年来ACS的临床治疗中得到了广泛应用[2]。但随着急诊溶栓、PCI及冠脉搭桥术的广泛开展及抗凝、抗血小板药物的大量应用,近年来ACS患者治疗后出血的发生风险不断上升,影响患者预后质量[3]。因此,寻求临床治疗及预防出血的平衡点,可提高ACS治疗效果。本研究选取955例ACS患者进行回顾性分析,旨在明确患者治疗后合并出血相关因素。
1 资料与方法
1.1 纳入标准与排除标准
于我院2012年5月至2016年5月收治的ACS患者中进行筛选。纳入患者参照文献相关标准确诊ACS[4]:①心电图2个或以上相邻导联ST段下移≥0.1 mV;②可见典型急性心肌梗死心电图演变;③心肌损伤标志物上升;④冠脉造影结果示至少1支主要血管管腔狭窄程度≥75%。符合上述任意1条标准即可确诊。临床资料保存完整。排除合并肥厚型心肌病、合并血液系统疾病或高危出血倾向、合并严重肝、肾功能不全、合并阿司匹林、氯吡格雷使用禁忌证、合并恶性肿瘤。共955例符合标准者纳入分析。
1.2 分析方法
1.2.1 出血事件分析 出血评价方法[5]:重度:出现颅内出血或心脏填塞,血红蛋白(Hb)下降>50 g/L
或血细胞比容(PCV)下降>15%。;中度:出血部位明确,Hb下降30~50 g/L,PCV下降>10%,或出血部位不明确,Hb下降40~50 g/L,PCV下降12%~15%;轻度:临床、影像学可见明显出血表现,Hb下降<30 g/L,PCV下降<9%。将治疗后出血者纳入出血组,将未出血者纳入未出血组,计算患者治疗后出血事件发生率。
1.2.2 相关因素分析 比较两组患者一般临床资料差异,计数资料以(n/%)表示,并采用χ2检验,计量资料以(x±s)表示,将存在统计学差异的因素纳入Logistic多因素回归分析,总结影响ACS患者治疗后合并出血的相关因素,并分析预防策略。
2 结果
2.1 出血事件发生率
955例患者中,共有48例患者发生治疗后出血,发生率为5.03%。出血患者中,颅内出血15例,脏器出血11例,体表出血22例,出血事件分度:重度5例,中度31例,轻度12例。
2.2 一般资料比较
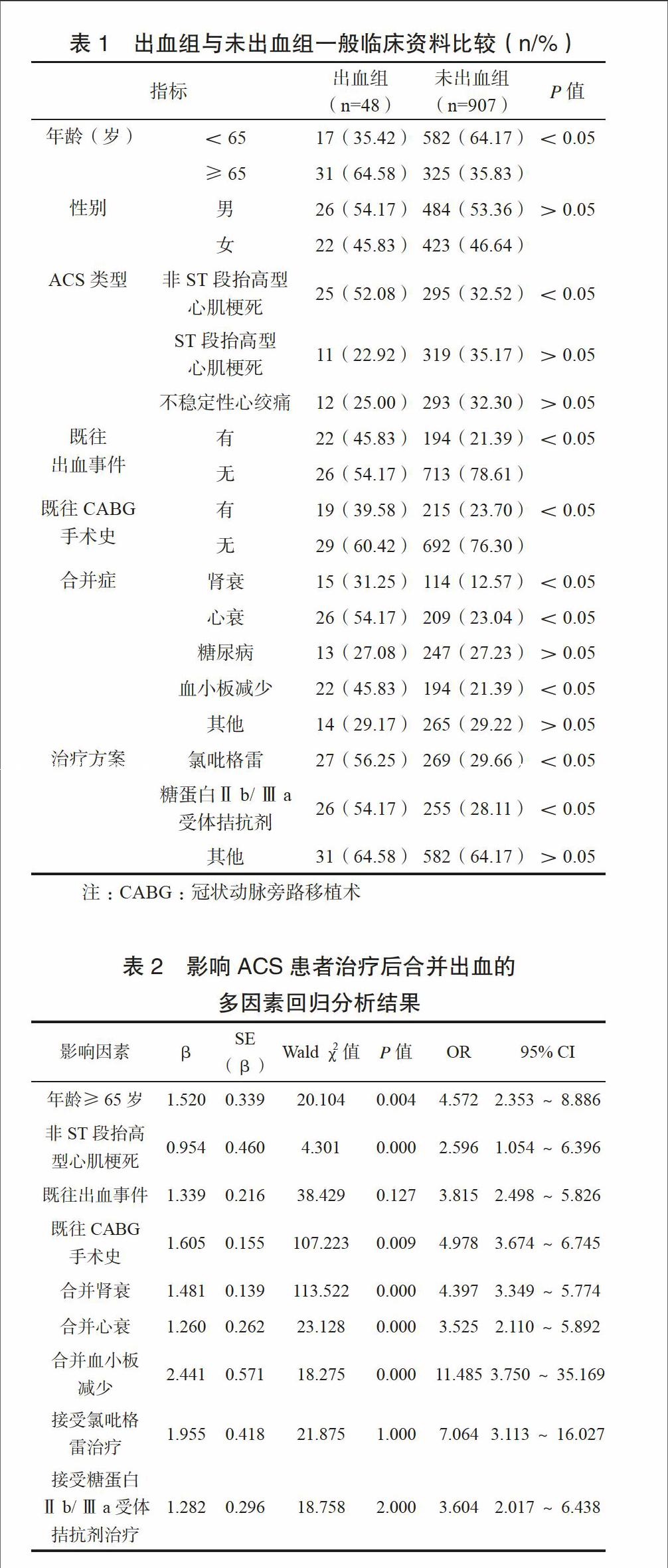
一般资料单因素分析可见年龄、ACS类型、既往出血时间、既往CABG手术史、合并心衰等、治疗方案比较,差异有统计学意义(P<0.05),见表1。
2.3 Logistic多因素回归分析
将单因素分析有统计学差异指标纳入Logistic多因素回归分析,如表2所示:年龄≥65岁、非ST段抬高型心肌梗死、既往出血事件、既往CABG手术史、合并肾衰、合并心衰、合并血小板减少、接受氯吡格雷治疗、接受糖蛋白Ⅱb/Ⅲa受体拮抗剂治疗是影响ACS患者治疗后合并出血的独立危险因素(P<0.05)。
3 讨论
本研究955例患者治疗后出血发生率达5.03%,ACS患者治疗后出血事件往往具有进展快、治疗矛盾、后果严重等特点[6],因此,在ACS患者的临床治疗中,如何寻求预防缺血及引发出血的平衡,早期识别治疗后合并出血高危人群十分关键[7-8]。
研究表明,年龄每增加10岁,患者出血风险即上升1%[9],加之老年患者往往伴有高血压、心脑血管系统疾病、慢性呼吸系统疾病等合并症,常年服用阿司匹林等非甾体抗炎药,药物对血小板凝血功能的影响及胃粘膜的损伤大大增加了脏器出血发生风险。Xian等[10]认为,老年人群血管硬化、心功能下降、循环功能衰退、新陈代谢下降等病理生理改变亦导致脏器储备代偿功能不良、组织粘膜保护能力下降,增加出血事件风险。非ST段抬高型心肌梗死患者病情往往较重,需接受更大剂量溶栓、抗凝、抗血小板药物治疗,药物对患者凝血功能的影响可导致其出血风险上升。既往有出血事件及CABG手术史患者,其凝血功能往往不够理想,加之过往出血、抗凝治疗的矛盾与复杂病变的长期介入操作,均在增加出血机会中扮演了重要角色[11-12]。Mega等[13]发现,合并严重肾功能不全患者,其出血风险较残存肾功能患者增加4倍,而合并心衰患者均处于血容量减少、心肌耗氧量增加状态,血管长期受损,出血不易终止,大出血发生风险更高[14]。
本研究显示氯吡格雷可导致出血发生率增加,但亦有学者指出,氯吡格雷不会导致致命性出血、失血性休克发生风险增加,安全性仍值得肯定[15-16]。作为冠心病的二级预防用药,糖蛋白Ⅱb/Ⅲa受体拮抗剂单独应用不会导致ACS患者治疗后出血风险升高,但由于多数患者均接受肝素抗凝治疗,糖蛋白Ⅱb/Ⅲa受体拮抗剂联合大剂量肝素可导致严重出血并发症风险急剧上升[17]。
因此,在今后的临床实践中,应早期意识到老年ACS患者治疗后合并出血风险,严格控制抗凝、抗血小板药物的剂量及使用时间,针对存在危险因素的患者提倡出血事件的早预防、早发现、早治疗[18],避免潜在、不必要出血事件的发生。
参 考 文 献
[1] Alexopoulos D, Stavrou K, Koniari I, et al. Ticagrelor vs prasugrel one-month maintenance therapy: impact on platelet reactivity and bleeding events[J]. Thromb Haemost, 2014, 112(3): 551-557.
[2] 孙静. 介入治疗对高龄急性冠状动脉综合征患者预后的影响[D]. 承德:承德医学院, 2015.
[3] Ducrocq G, Schulte P J, Becker R C, et al. Association of spontaneous and procedure-related bleeds with short-and long-term mortality after acute coronary syndromes: an analysis from the PLATO trial[J]. EuroIntervention, 2015, 11(8): 737-745.
[4] 许俊堂, 胡大一. 对急性冠状动脉综合征分型的看法[J]. 中华心血管病杂志, 2001, 29(09):566-568.
[5] Mega J L, Braunwald E, Murphy S A, et al. Rivaroxaban in Patients Stabilized After a ST-Segment Elevation Myocardial Infarction: Results From the ATLAS ACS-2–TIMI-51 Trial [J]. J Am Coll Cardiol, 2013, 61(18): 1853-1859.
[6] Kaul P, Tanguay J F, Newby L K, et al. Association between bleeding and mortality among women and men with high-risk acute coronary syndromes: insights from the Early versus Delayed, Provisional Eptifibatide in Acute Coronary Syndromes (EARLY ACS) trial[J]. Am Heart J, 2013, 166(4): 723-728.
[7] 曾秋棠, 彭昱东. 关注急性冠状动脉综合征抗栓和出血的平衡[J]. 临床心血管病杂志, 2013, 29(5): 321-323.
[8] Chhatriwalla A K, Amin A P, Kennedy K F, et al. Association between bleeding events and in-hospital mortality after percutaneous coronary intervention[J]. JAMA, 2013, 309(10): 1022-1029.
[9] 张予. 急性冠状动脉综合征相关研究[D]. 武汉:华中科技大学, 2014.
[10] Xian Y, Wang T Y, McCoy L A, et al. Association of Discharge Aspirin Dose With Outcomes After Acute Myocardial Infarction Insights From the Treatment with ADP Receptor Inhibitors: Longitudinal Assessment of Treatment Patterns and Events after Acute Coronary Syndrome (TRANSLATE-ACS) Study[J]. Circulation, 2015, 132(3): 174-181.
[11] Tang X F, Fan J Y, Meng J, et al. Impact of new oral or intravenous P2Y12 inhibitors and clopidogrel on major ischemic and bleeding events in patients with coronary artery disease: a meta-analysis of randomized trials[J]. Atherosclerosis, 2014, 233(2): 568-578.
[12] 何菲, 殷跃辉, 李芝峰, 等. 不同性别急性冠脉综合征患者的临床特征分析:480例回顾性研究[J]. 解放军医学杂志, 2014, 39(6): 489-493.
[13] Mega J L, Braunwald E, Wiviott S D, et al. Comparison of the Efficacy and Safety of Two Rivaroxaban Doses in Acute Coronary Syndrome (from ATLAS ACS 2–TIMI 51)[J]. Am J Cardiol, 2013, 112(4): 472-478.
[14] Krantz M J, Kaul S. The ATLAS ACS 2–TIMI 51 Trial and the Burden of Missing Data:(Anti-Xa Therapy to Lower Cardiovascular Events in Addition to Standard Therapy in Subjects With Acute Coronary Syndrome ACS 2–Thrombolysis In Myocardial Infarction 51)[J]. J Am Coll Cardiol, 2013, 62(9): 777-781.
[15] 张伟, 孙中华, 米杰, 等. 三联抗血小板对急性冠脉综合征患者经皮冠状动脉介入术后30天内的作用[J]. 中华急诊医学杂志, 2013, 22(7): 721-725.
[16] Levine G N, Jeong Y H, Goto S, et al. Expert consensus document: World Heart Federation expert consensus statement on antiplatelet therapy in East Asian patients with ACS or undergoing PCI[J]. Nat Rev Cardiol, 2014, 11(10): 597-606.
[17] Tantry U S, Bonello L, Aradi D, et al. Consensus and update on the definition of on-treatment platelet reactivity to adenosine diphosphate associated with ischemia and bleeding[J]. J Am Coll Cardiol, 2013, 62(24): 2261-2273.
[18] Klingenberg R, Heg D, R?ber L, et al. Safety profile of prasugrel and clopidogrel in patients with acute coronary syndromes in Switzerland[J]. Heart, 2015, 101(11): 854-863.