Technology Deployment to Improve Clinical Outcomes
T.M. Judd, L. Jacobs, M. Jansen, B. Birch
1.National Project Director, Clinical Technology, Kaiser Permanente, BRTH Board, Atlanta, GA 30305, USA; 2.Associate Editor-in-Chief, The Permanente Journal, President, BRTH Board, Atlanta, GA 30305, USA; 3.Chief Business Development Specialist, Iron Bow Healthcare Solutions, Atlanta, GA, USA; 4.Innovation Technology Architect, Innovation and Advanced Technology, Kaiser Permanente IT, Oakland, CA, USA
Technology Deployment to Improve Clinical Outcomes
T.M. Judd1, L. Jacobs2, M. Jansen3, B. Birch4
1.National Project Director, Clinical Technology, Kaiser Permanente, BRTH Board, Atlanta, GA 30305, USA; 2.Associate Editor-in-Chief, The Permanente Journal, President, BRTH Board, Atlanta, GA 30305, USA; 3.Chief Business Development Specialist, Iron Bow Healthcare Solutions, Atlanta, GA, USA; 4.Innovation Technology Architect, Innovation and Advanced Technology, Kaiser Permanente IT, Oakland, CA, USA
Improved child, newborn, and maternal health (CNM) is a top priority in developing countries. Many factors must be addressed simultaneously to improve clinical outcomes for CNM. A public-private project in Haiti that will deploy the World Health Organization (WHO) evidence-based medicine (EBM) and essential interventions utilizing CNM healthcare technologies (HT), is expected to be a model for improving national health systems. The CNM mortality rates in Haiti are the highest in the western hemisphere with rates similar to those found in Afghanistan and several African countries. Several factors perpetuating this crisis are noted, as well as the most cost-effective interventions proven to decrease CNM mortality rates in low-and middle-income countries. To create major change in health system infrastructure, two strategies are presented, requiring appropriate and leading-edge health technologies (HT),e.g., wireless cellular-network-based Telemedicine (TM): (1) Development of a countrywide network of geographical“Community Care Grids” to facilitate implementation of frontline interventions; (2) The construction of a central hospital (called Bethesda Referral and Teaching Hospital-BRTH NGO) that will provide secondary and tertiary care for communities throughout the country, including helping local hospitals and clinics practice EBM care. We believe that these strategies-supported by HT will fast track improvement in CNM mortality rates throughout the country and that in a relatively short period of time Haiti’s health care system will be among the leaders in the region. Primary factors contributing to the CNM crisis, all addressed by TM: (1) Limited access: demographics, geography, cost, transportation; (2) Inadequate health care facilities: less than 20 NICU beds for 10 million population; BRTH to provide 80 bed NICU and 40 bed PICU in 225 bed hospital; (3) Health care practitioners: inadequate numbers and training; (4) Low% of skilled attendants now at deliveries; (5) Low % of prenatal and postnatal visits; and (6) High risk deliveries in qualifi ed health facilities: only 25% now. BRTH NGO guiding principles: (1) Partnerships:Internal: Public-Ministry of Health and Private hospitals; External: collaboration with USA-based CNM specialists (on-site at BRTH and via TM); (2) Philanthropic donor model for both capital and operating funds: a leading WHO CNM physician expert says BRTH to provide EBM care for “pennies on the dollar comparatively”; (3) Public-Private Partnership plan for national/regional HT Management Projects and Maintenance Centers; BTRH at new Port; (4) Care processes: to meet Joint Commission International (JCI) Standards; (5) Safety and Security design: addressing seismic issues; (6) Countrywide: hospitals in Haiti’s 10 internal regions/provinces enabled for EBM; and (7) Financial: patient remuneration based on sliding scale for no charge care as needed. EBM and Essential Interventionsutilize HT at every stage of CNM care:(1) Pregnancy; (2) Delivery; (3) Post-Delivery: Mother and Baby; and (4) Infancy and Childhood up to age 5.
evidence-based medicine; essential health technologies; health technology management; telemedicine
0 INTRODUCTION
The World Health Organization (WHO), US Agency for International Development (USAID), United Nations International Children’s Emergency Fund (UNICEF) and other international agencies have published several years of annual child, neonatal, and maternal (CNM) mortality rates for countries around the world. Although the rates and annual trends are important in understanding the extent of a country’s problems, a comparison of the results with regional countries adds valuable information to the understanding of the magnitude of a crisis. This is especially true when Haiti’s mortality rates are compared with elsewhere in the Caribbean as well as other developing nations[1].
According to UNICEF, Haiti has the highest rates of infant, children under five, and maternal mortality in the Western hemisphere[1]. Since it is estimated that there were 265,000 live births in Haiti in 2013, these rates underscore the magnitude of the number of deaths in each CNM category, shown in Table 1, particularly in comparison to the Dominican Republic (DR-who has same size population) and other Caribbean countries[1].
1 HAITI HEALTHCARE INFRASTRUCTURE
In addition to these medical causes of CNM mortality, there are several other factors that contribute to the inadequacies of the Haitian health care system infrastructure.
1.1 Limited accessibility
Geographical isolation: A high percentage of the Haitian population lives in rural, mountainous areas accessible only by extremely poor roads; very important since rural residents have limited access to care and qualifi ed medical facilities.
Cost barrier: Evidence suggests that the financial barrier is also a key obstacle for pregnant women needing access to obstetric care. 47% of the population lacks access to health care primarily because of these two barriers[1].
1.2 Inadequate health care facilities
The earthquake of January 2010 had terrible consequences for the Haitian society and health sector. Sixty percent of the infrastructure was destroyed including over fifty health institutions with losses and damage in the health sector that exceeded 200% of annual expenditure in health from all sources.
Even before the earthquake, the number and quality of health care facilities were inadequate to care for a population exceeding ten million. Over the years we have learned from our visits to hospitals that a major contributing factor for the CNM deaths in Haiti is the fact that there is a major shortage of neonatal intensive care units (NICUs), pediatric ICUs, and adult ICUs. This dire shortage of NICUs underscores the poor condition of the Haiti health care system[1].
1.3 Health care practitioners - inadequate numbers and training: Low % of skilled attendants at deliveries
Industrialized countries in the early 20th century halved maternal mortality by providing professional midwifery care at childbirth. Births attended by skilled health personnel is a key indicator for improvements in maternal health.
It is not difficult to understand why the neonatal and maternal death rates in Haiti are so high when you understand that 63% of countrywide deliveries and 75% of deliveries in rural settings were not attended by a skilled provider[1].
1.4 Low percentage of prenatal and postnatal visits
Prenatal Care: 40% of pregnant women in Haiti did not have antenatal care visit before their fourth month of pregnancy[1].
1.5 High-risk deliveries in qualifi ed health facilities
Only 25% of Haitian women deliver in institutions, with 78.2% of women in the richest quintile delivering in health centers versus 5.9% of women in the poorest quintile[1].
2 STRATEGIES TO ADDRESS THE CRISIS
To address the CNM health crisis, for the past two years we have begun to implement two primary strategies: (1) The development of a countrywide community care grids, a network of defined geographical population to facilitate the implementation of frontline EBM interventions; and (2) The construction of a 225-bed central referral and teaching hospital that will provide specialty care for communities throughout the country, due to open in 2017[1].
2.1 Overview: bethesda referral & teaching hospital
This private, not-for-profi t specialty teaching hospital will be centrally located near the international airport and Haiti’s capital Port-au-Prince to facilitate transfers from across the country. Although there are many capable hospitals, most focus on primary and emergency care.
BRTH will provide access to care for high-risk infant and maternal patients throughout all of Haiti. High-risk obstetrical and pediatric patients will be triaged and transported from other hospitals to BRTH as necessary.
BRTH staff will consist at any one time of over 100 North American short-term health care volunteers providing one-onone mentoring for physicians, midwives, and nurses from the Haiti medical community, an approach that is not being utilized elsewhere in Haiti[1].
2.2 BRTH at port lafi to
Port Lafi to is a new, private economic zone covering more than 1,000 acres of oceanfront land developed 12 miles north of Port-au-Prince in the town of Lafi teau[3]. Land for BRTH has been donated by GB Group of Miami, one of the leading private industrial groups in the Caribbean. GB Group and BRTH already has become a strong partnership as both organizations have the same vision of expediting improvements in the quality of life for all Haitians. GB group is also making available all of their expanding IT resources at the Port and country-wide.
3 FAST TRACKING IMPROVEMENTS IN CNM
3.1 Implementing EBM interventions in the community
Although the literature is not very robust in identifying evidence-based medicine (EBM) interventions[1], there is sufficient data from several meta-analyses to identify proven interventions, and to propose strategies for Low and Middle Income Countries such as Haiti. We are implementing only EBM-based interventions that have been proven to be costeffective, are culturally relevant, and can be deployed successfully. Examples of HT used in EBM interventions are shown in Table 1.
3.2 Developing “community care grids”
To assist regions throughout Haiti in implementing necessary interventions, and to address the top three causative factors—access, low % of skilled attendants, and low % of prenatal visits—we have created a countrywide networking and community training approach that we call “community care grids,” see Figure 1.
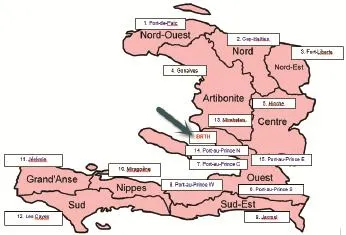
Figure 1 Community care grids.

Table 1 The magnitude of the number of deaths in each child, neonatal, and maternal category
3.3 Increase number & skills of health care professionals
As a specialty teaching hospital, there will be extensive learning opportunities for Haitian health care personnel, including but not limited to, physicians, midwives, nurses, nurse practitioners, residents, and students from all disciplines. Also included in training will be X-ray and laboratory technicians, hospital administrators, clinical engineering staff, hospital food preparation, security, and facilities maintenance personnel. Care processes will be conducted according to JCI standards[4].
3.4 Providing affordable, quality health care
The underlying poverty in Haiti is a major barrier for mothers and children in accessing health care. As a short-term solution, community care grid team members will take steps to make certain that cost will not be barrier to care and thatservices will be provided regardless of the ability to pay.
3.5 Leveraging communications and technology
BRTH communications center: The hospital will provide a 24/7 central hub for the fl ow of information from the many Community Care Grid sites throughout the country.
Technology: BRTH will leverage state-of-the-art telemedicine capabilities from any location in the country to provide“e-consults” with colleagues at BRTH and or with experts across North America[5]. Real-time telemedicine (TM) for ultrasonography and cardiac assessments, will help determine the most appropriate CNM interventions:
(1) Care grids with TM use case overview in Figure 2[5]. (2) Grid portable TM: remote monitoring; ‘All in Scope’ -full patient examination; bluetooth TM; TM ultrasound.
(3) Portable TM unit to monitor patients at central grid site,e.g., Virtual Care Clinic (VCC), with live TM hookups.
‘Live hookup’ means consultation in real-time.
For others, clinical team will go to the ‘local’ patient site, with “store and forward” using portable TM for later viewing and consultation.

Figure 2 Care grids with telemedicine use case overview.
Enabling the telemedicine network: Question: How will this Haiti TM venture succeed where many like it before have not in other developing countries? Answer: With the Port as an economic driver and use of emerging health IT tools:
(1) BRTH: land for hospital is donated; has use of all Port IT resources.
(2) Port IT resources: provides a supporting Tier 3 IT Data Center with expansion capability, a 25 MW Power grid, and an economic free zone attracting new industry and related increasing IT resources. The Port Data Center uses fiberoptic inputs from Haiti cell providers Digicel and Natcom, and also microwave. Now 15 Mbps bandwidth, expanding to 100 Mbps for BRTH[6].
(3) Improving communication infrastructure: The country has growing wireless cell coverage, typically with 4G in the regional capitals.
(4) Virtual care clinics (VCC): For TM, the VCC located at regional sites will have dedicated fiberoptic T-1 lines and sufficient bandwidth for clinical video transmission, and to enable ongoing patient remote monitoring utilizing mobile TM kits and cellular phone-based patient communications,e.g., texting care reminders to expectant mothers[5].
(5) BRTH’s electronic health record (EHR) platform:allows integration of remote monitoring and other Haitian hospital networks’ data via physician and patient portals, fax, direct-messaging, HL7&CCDA[7].
4 HEALTH TECHNOLOGY MANAGEMENT (HTM)
BRTH will be very medical device oriented. Not only will the initial investment in HT be important, but ongoing equipment management (HTM) and support will be critical. This will involve not only a talented clinical engineering (CE) group at BRTH, working in collaboration with other health IT teams, but also requirements for partnership with other public and private hospitals around the country to ensure that many can successfully deliver EBM CNM care.
There have been several private and public initiatives underway to build HTM capacity in Haiti, but there is a long way to go. Houston Rotary (USA-private hospitals) and the Tripartite group (Cuba-public) have facilitated the largest biomedical equipment technician (BMET) training. There have many other efforts such as from Pan American Health Organization (WHO-PAHO), USA-based Partners in Health, TriMedx Foundation, IMEC America, Catholic Relief Services, as well as entities from other countriesand NGOs for many hospitals in Haiti; together combining for over 100 BMETs educated. However, past initial training, there is the challenge of ongoing medical device learning and support.
There was a January 2013 Haiti HTM assessment with twenty private hospital leaders; these needs were identifi ed:
(1) BMET workspace, tools, and test equipment.
(2) Repair, parts, and supplies challenges.
(3) Device inventory management tools.
(4) Equipment donations’ issues.
(5) Ongoing management (hospital leader) and BMET training.
(6) Hospital leader partnerships (regional/national) for HTM.
A similar meeting of public hospital leaders in October 2013, facilitated by PAHO[8], yielded similar logistics’ results:
(1) Lack of (fully) trained BMETs; need for more focused training.
(2) Inventory capture & ongoing equipment manage-ment challenges.
(3) Access to spare parts in a timely manner.
(4) Scope of HTM; what breadth of services provided and how.
(5) Donations: how to best use: if not used storage; accessories.
(6) Hospital directors are frustrated with HTM status; lack funding, need in-kind sharing of resources; need clear HTM job roles.
(7) Logistics: storage space for device awaiting repair; if share unused devices with regional service center, can they get credit?
(8) Self-suffi ciency unrealistic for single hospital HTM.
(9) Optimize existing HTM resource: more experienced HTM leaders to serve as Advisors to national/regional service centers; where resources can be pooled and shared,e.g., noted in items 1-8 above.
More recently there have been two encouraging initiatives:(1) two Haitian HTM experts participated in the WHO-led global best practice HTM seminar in June 2015[9]; and (2) there was an August 2015 meeting of in-country HTM leaders both from the public and private sectors, indicating growing interest in finding creative ways in which to partner. Other countries have demonstrated that such partnerships can be successful[10]. A follow-up country-wide gathering including vendors is planned for November 2015. An earlier plan from 2013[8]shows one possible path forward:
Desired HTM initiatives over the next 5 years:
Equipment support: (1) Make best use of existing trained BMETs; additional training to be determined by public/private hospital demand. BMET training only without Management Support component is not sustainable[11]; (2) Develop HT Unit (Service Center) with public-private partnership, and regional satellites; utilizing at least a break-even business model; (3) National Center would have a paid HT Manager, and volunteer BMETs “on-loan” from local hospitals, as would Satellite units; (4) Best practice HTM developed jointly by paid HTM Coordinator (USA-based) and Haiti HT Manager, under Partnership Advisory Board oversight. In return for sharing BMETs, centers would allow ongoing learning of support solutions benefi ting all.
Management support: (1) Maintain network of public & private health leaders to guide HT units; with rotating volunteer BMETs, guided by Partnership Advisory Board; (2) Develop and enable ongoing training for health leaders and BMETs.
Project support: Support hospital technology projects as encouraged by Partnership Advisory Board;e.g., BMET staffing, equipment user training, eHealth-mobile health, donation guidelines, etc.
5 CONCLUSION
This paper discusses the rare opportunity to apply EBM care for high priority CNM conditions combining essential health technologies and health IT tools. It demonstrates the potential to raise the level of care across a country in need, through a model of collaborative relationships and best use of technology, to deliver improved clinical outcomes.
6 ACKNOWLEDGMENTS
The contribution of many volunteers for the BRTH project is gratefully acknowledged, from individuals and companies.
[1] Jacobs L,Judd T,Bhutta Z.Addressing the Child and Maternal Mortality Crisis in Haiti.Permanente Journal,2015.
[2] World Health Organization 2015.Interagency list of medical devices for essential interventions for reproductive, maternal, newborn and child health.
[3] Port Lafito 2015 Available from:http://gbgroup.com/ourbusinesses/infrastructure/port-lafito/.
[4] JCI Standards 2015.Available from: http://www.jointcommissioninternational.org/.
[5] Jansen M,Birch B.BRTH Telemedicine,Health IT and Electronic Health Record(EHR)planned functionality.Iron Bow,Inc., Kaiser Permanente,2015.
[6] USA Health IT 2015.Available from:www.healthit.gov/ providers-professionals/faqs/what-recommended-bandwidthdifferent-types-health-care-providers.
[7] CCDA is Consolidated Clinical Document Architecture for EHRs.Available from:www.healthit.gov/policy-researchersimplementers/consolidated-cda-overview.
[8] Judd T.HTM Country Initiatives:Developing HTM Capacity for Haiti.WHO 2ndGlobal Forum for Medical Devices,2013. Available from:www.who.int/medical_devices/en.
[9] Judd T.Global HTM Seminar Report,ACCE News,2015. Available from:www.accenet.org.
[10] Worm A,Schofield R.How THET partnership model different; 2 years of medical partnerships in 5 African countries,2014. THET.Available from: www.thet.org.
[11] Hernandez A,Judd T,Castañeda M,et al.ACCE Advanced CE/HTM Workshops,WHO 2ndGlobal Forum for Medical Devices,2013.
R197.39 [Document code] A
10.3969/j.issn.1674-1633.2016.01.001
1674-1633(2016)01-0001-05
Thomas Judd, MS, CCE, CPHQ, CPHIMS, FACCE, FHIMSS, National Project Director, Clinical Technology, Kaiser Permanente, 1821 Jacksons Creek Point, Atlanta, GA 30305, USA.
E-mail: judd.tom@gmail.com

