四妙散加味联合左卡尼汀治疗少、弱精症疗效观察
陈其华 赵丹
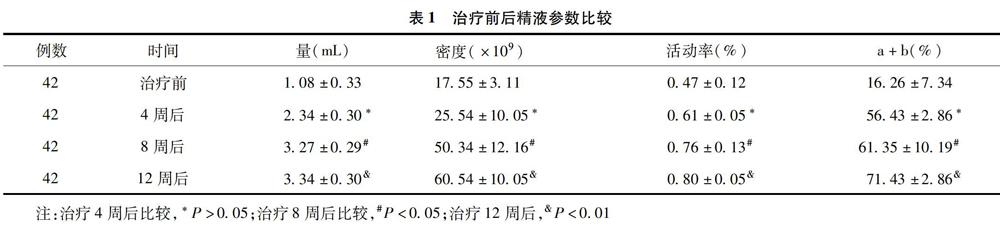
【摘要】目的:观察中药四妙散加味治疗湿热下注证少、弱精症临床疗效。方法:选取符合标准的42例患者,服用四妙散加味和左卡尼汀口服液联合治疗。结果:42例患者治疗后痊愈16例,显效18例,有效4例,无效4例,总有效率为90.48%。治疗4周后自身前后对照精液量、活动率、精子密度、(a+b)级精子含量差异均无统计学意义(P>0.05);治疗8周后差异具有统计学意义(P<0.05);治疗12周后差异具有显著统计学意义(P<0.01)。结论:四妙散加味联合左卡尼汀口服液治疗少、弱精症具有较好临床疗效,值得进一步研究。
【关键词】四妙散;湿热下注证;少、弱精症
【Abstract】Objectives: To observe the clinical curative effect of traditional Chinese medicine (TCM) Simiaosan jiawei in treating asthenozoospermia. Methods: 42 patients meeting the criterion were selected and treated with Simiaosan jiawei combined with l-carnitine. Results: According to the results of 42 patients, there were 16 cured cases after treatment, 18 cases with markedly effect, 4 cases with effective results and 4 invalid cases. The total effective rate was 90.48%. The differences in semen quantity, activity rate, sperm density, and sperm (grade a + b) content between 4 weeks after treatment and before the treatment had no statistical significance (P> 0.05). The difference between 8 weeks after treatment and before the treatment was statistically significant (P< 0.05); The differences between 12 weeks after treatment and before the treatment had statistical significance (P< 0.01). Conclusion: Simiaosan jiawei combined with l-carnitine has good clinical curative effect in the treatment of asthenozoospermia, which is worthy of further investigation.
【Key words】Simiaosan jiawei; Damp-heat syndrome; Asthenozoospermia
【中图分类号】R277.33【文献标志码】A
据统计我国育龄夫妇中不孕不育患者约占10%,其中男方因素占30%3.41 years old, and the pelvic organ prolapse quantification (POP-Q) stage was III~IV stage. Pre- and post-operative symptoms were assessed using the urinary distress inventory (UDI-6) and the incontinence impact questionnaire (IIQ-7), and the international continence society criteria were used for the urodynamic evaluation. Results: Among the total 30 patients, 22 patients underwent partial colpocleisis and another 8 underwent the total colpocleisis. Seven women underwent also a concomitant trans-obturator tension-free (TOT) procedure. Of the patients, 65.7%, 26.8% and 7.5% were ‘very satisfied, ‘satisfied and ‘not satisfied, respectively. After the colpocleisis operations, UDI-6 and IIQ-7 scores were improved significantly (P>0.05). Post-operative urinary retention was not observed and prolapse recurred in one patient. Conclusion: Colpocleisis is a safe and effective surgical technique in treating the pelvic organ prolapse for the elderly female patients, with a high patient satisfaction rate.
【Key words】Colpocleisis; Pelvic organ prolapse; Efficacy; Satisfaction rate
【中图分类号】R713.4【文献标志码】A
盆腔脏器脱垂(pelvic organ prolapse, POP)常因盆底支持组织缺损或松弛而引起,使得盆腔脏器脱离原先正常的解剖位置,包括子宫脱垂、阴道脱垂,同时伴有膀胱、直肠和小肠膨出。该病的临床症状一般表现为慢性盆腔痛、走路或站立时有下坠感或压迫感以及性交不适,影响患者正常生活[1,2]。如今,随着人口老龄化现象的加剧,POP发病率呈上升趋势。妇女健康研究显示已婚妇女子宫脱垂发病率为0.04%~0.14%,51~60岁妇女发病率为0.33%,60岁以上为0.71%。而对于年老体弱、不能耐受较大手术且不需保留性交功能患者,阴道封闭术(包括阴道全封闭术和部分阴道封闭术)是该病的首选治疗方式[3,4]。本研究旨在探讨阴道封闭术治疗盆腔脏器脱垂的有效性及患者的满意度。现报告如下。
1资料与来源
1.1一般资料
纳入标准包括年龄大于66岁小于85岁,平均为(70.58±3.41)岁,其中61~70岁8例,71~80岁15例,81~90岁7例;盆腔脏器脱垂量化评分系统(POP-Q)分期为III~IV期。排除生殖器有恶性病变和有性生活要求的患者。根据以上标准,选取2014年2月至2014年11月于我院行阴道全封闭术或阴道部分封闭术老年妇女患者30例为研究对象。所有患者及家属在术前知悉本实验的研究目的,对选择该手术方式均知情并同意,且签署知情同意书。
1.2研究方法
阴道封闭术手术方式的选择:宫颈柱状上皮异位且脱垂严重者切除子宫后行完全封闭术,即切除从处女膜内2~3cm至阴道穹窿全部的阴道前后壁黏膜上皮,有子宫时同时切除之再将阴道前后壁全长的黏膜下层缝合以关闭阴道。宫颈正常者,行阴道部分封闭术,即切除从处女膜内2~3cm至阴道穹窿处的中间部分阴道前后壁黏膜上皮,两侧保留1~2cm的阴道黏膜上皮以分别形成两个通道,多不切除子宫以阴道前后壁中间部分的黏膜下组织缝合后关闭中间大部分的阴道。30例患者均在夫妻双方同意条件下行阴道封闭手术治疗,其中22例行部分阴道封闭术,8例行全阴道封闭术。在手术前,对所有患者进行标准评估,包括子宫颈涂片检查、子宫内膜取样及经阴道和肾超声检查。在阴道封闭手术前和手术后,利用泌尿生殖系统症状总表(UDI-6)[5]和尿失禁影响问卷(IIQ-7)[6]评估患者的相关症状,并利用国际尿控协会标准[7]对患者进行尿动力学评估。患者的主观满意度分为4个等级:非常满意、满意、不满意和后悔。尿动力学压力性失禁患者同时行伴随经闭孔无张力尿道中段吊带术(TOT),术后患者排尿后膀胱残余尿量(PVR)少于100mL视为正常。
1.3统计学分析
研究产生的数据使用SPSS18.0统计学软件进行分析。计数资料和计量资料组间比较分别采用χ2检验及两独立样本t检验,当统计值P<0.05时,表示两组间差异有统计学意义。
2结果
2.1患者人口统计学资料
本研究中30例患者的术后平均随访时间是(27.4±5.2)个月(12~78个月),患者的人口统计学资料和手术资料见表1。有1例患者有子宫脱垂史曾行经阴道子宫切除术,其他26例无任何子宫脱垂手术史。部分阴道封闭手术中有1例患者接受局部麻醉,其他均接受脊髓麻醉。部分阴道封闭手术(22例)和全阴道封闭手术(8例)的平均用时分别为(25.4±3.6)min和(61.2±3.4)min,无明显术前并发症发生。
2.2患者的尿失禁情况
阴道封闭手术前,有7例患者被诊断为尿动力学压力失禁,对其进行经闭孔无张力尿道中段吊带术,10例患者有逼尿肌过度活跃的尿动力学情况。术后,3例患者有压力性尿失禁症状,即行伴随经闭孔无张力尿道中段吊带术患者中有1例出现尿动力学压力失禁,2例无抗尿失禁措施患者在阴道封闭术术后被诊断为尿动力学压力失禁。所有患者在术后再无逼尿肌过度活跃现象。96.6%(29/30)患者表现出明显的解剖学成功,但是有1例患者盆腔脏器出现脱垂复发。术后,患者排尿后膀胱残余尿量(PVR)均少于100mL,表现正常。
2.3患者的各项评分情况
30例患者在阴道封闭手术前、后的IIQ-7平均总得分分别为15.18±1.98和3.62±0.66,且差异具有显著统计学意义(P<0.05)。20例无任何抗尿失禁措施患者在手术后IIQ-7总得分、UDI-6刺激性、UDI-6压力性和UDI-6阻塞性子得分均发生降低,且差异具有显著统计学意义,见表2。例如,IIQ-7得分和UDI-6阻塞性得分在手术前后有显著统计学差异(P<0.05)。7例伴随TOT手术患者的这四项得分在行阴道封闭术后也有所降低。所有患者中,93.3%(28/30)对本次治疗表示满意,即66.7%(20/30)和26.7%(8/30)分别表示为非常满意和满意。有2例患者表示后悔,1例是因盆腔脱垂的复发,另1例是因为压力性失禁的发生。
3讨论
随着人口老龄化的加剧,临床上盆腔脏器脱垂及尿失禁日益多见,该病虽不是威胁生命的疾病,但其症状严重影响妇女健康及生活质量,尤其是妨碍妇女工作和日常社会活动,可引发一系列社会和卫生问题。北京大学人民医院曾对北京市房山区某自然村18岁以上常住已婚女性进行问卷调查和妇科检查,结果显示女性尿失禁和盆腔脏器脱垂均较常见,尿失禁患者多合并盆腔脏器脱垂,对生活质量有较大影响[8]。该病的治疗目标是改善患者的生活质量,具体治疗方案的选择须综合多种因素,如患者年龄、临床共病、性功能欲望及复发的危险因素等[9-11]。阴道封闭术适用于年纪较大、合并多种内科合并症的盆腔脏器重度脱垂患者,因术后性功能丧失,术前须与患者及家属充分沟通并排除宫颈或子宫疾患[12]。
本研究中,93.3%(28/30)患者对阴道封闭手术的治疗表示满意,并有96.6%(29/30)患者表现出明显的解剖学成功,这与之前报道的阴道封闭术拥有较高的解剖学成功(91%~100%)相一致[13]。压力性失禁和冲动症状是该病患者常有的麻烦[14]。在本研究中,泌尿生殖系统症状总表(UDI-6)结合尿失禁影响问卷(IIQ-7)用于评估尿失禁对患者生活质量的影响。结果显示行阴道封闭手术患者术后的IIQ-7总得分较手术前发生显著性降低[(15.18±1.98) vs. (3.62±0.66),P<0.05)],表明该手术治疗方式的有效性。另外,不论患者是否行伴随经闭孔无张力尿道中段吊带术,UDI-6阻塞性得分在手术前后均有显著统计学差异(P<0.05)。盆腔脏器脱垂患者有较高的尿潴留发病率,对这些患者实施抗尿失禁手术可能使得尿道流阻塞加剧,但是盆腔的足够修复可以解决阻塞问题。阴道封闭手术前,五分之一患者的PVR值大于100mL,但是术后所有患者的该值均低于100mL,暗示尿道流阻塞问题的缓解。这与之前发现相一致,即阴道封闭术和伴随尿道中段吊索干预可在不引起明显尿潴留的情况下改善患者的尿道症状[15]。尽管阴道封闭术适用于不需要性功能的老年妇女患者,但是一些问题依然存在。如阴道闭塞可能会改变妇女的生殖器解剖和阴道功能,进而严重影响患者的身体意象导致患者不满意甚至产生盆腔脏器脱垂治疗的后悔心理[16]。阴道封闭术后患者的后悔率一般在3%~10%之间,而本研究仅有2例(6.7%)患者有后悔心理。但是,这2例患者主要担心的并非失去的性功能,1例是因盆腔脱垂的复发,另1例是因压力性失禁的发生。本研究的所有患者中,93.3%(28/30)对治疗表示满意,即66.7%(20/30)和26.7%(8/30)分别表示为非常满意和满意。
总的来说,阴道封闭术是一种治疗老年患者盆腔脏器脱垂既安全又有效的手术方式,能显著提高老年妇女患者的生活质量且患者具有较高的主观满意度。
参考文献
[1]Maher CM, Feiner B, Baessler K, et al. Surgical management of pelvic organ prolapse in women: the updated summary version Cochrane review. International Urogynecology Journal, 2011, 22(11): 1445-1457.
[2]Pillalamarri N, Shalom D, Sanidad S, et al. The prevalence of microscopic hematuria in a cohort of women with pelvic organ prolapse. International Urogynecology Journal, 2015, 26(1): 85-90.
[3]Mueller MG, Ellimootil C, Abernethy MG, et al. Colpocleisis: Asafe, minimally invasive option for pelvic organ prolapse. Female Pelvic Medicine & Reconstructive Surgery, 2015, 21(1): 30-33.
[4]Vij M, Bombieri L, Dua A, et al. Long-term follow-up after colpocleisis: regret, bowel, and bladder function. International Urogynecology Journal, 2014, 25(6): 811-815.
[5]Murphy M, Sternschuss G, Haff R, et al. Quality of life and surgical satisfaction after vaginal reconstructive vs obliterative surgery for the treatment of advanced pelvic organ prolapse. American Journal of Obstetrics and Gynecology, 2008, 198(5): 573. e1-573. e7.
[6]Wheeler TL, Richter HE, Burgio KL, et al. Regret, satisfaction, and symptom improvement: analysis of the impact of partial colpocleisis for the management of severe pelvic organ prolapse. American Journal of Obstetrics and Gynecology, 2005, 193(6): 2067-2070.
[7]Gammie A, Clarkson B, Constantinou C, et al. International Continence Society guidelines on urodynamic equipment performance. Neurourology and Urodynamics, 2014, 33(4): 370-379.
[8]王建六,曹冬,张晓红,等.北京郊区女性尿失禁及盆腔脏器脱垂发病情况及其对生活质量影响的抽样调查.中国妇产科临床杂志,2007,8(1):5-9.
[9]Hagen S, Stark D, Glazener C, et al. Individualised pelvic floor muscle training in women with pelvic organ prolapse (POPPY): a multicentre randomised controlled trial. The Lancet, 2014, 383(9919): 796-806.
[10]Wu JM, Matthews CA, Conover MM, et al. Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstetrics & Gynecology, 2014, 123(6): 1201-1206.
[11]Kakos AB, Lovejoy DA, Whiteside JL. Quality of information on pelvic organ prolapse on the Internet. International Urogynecology Journal, 2015, 26(4): 551-555.
[12]Koski ME, Chow D, Bedestani A, et al. Colpocleisis for advanced pelvic organ prolapse. Urology, 2012, 80(3): 542-546.
[13]Abbasy S, Kenton K. Obliterative procedures for pelvic organ prolapse. Clin Obstet Gynecol, 2010(53):86-98.
[14]Catanzarite T, Rambachan A, Mueller MG, et al. Risk factors for 30-day perioperative complications after Le Fort colpocleisis. The Journal of Urology, 2014, 192(3): 788-792.
[15]Abbasy S, Lowenstein L, Pham T, et al. Urinary retention is uncommon after colpocleisis with concomitant mid-urethral sling. Int Urogynecol J, 2009(20):213-216.
[16]Fitzgerald MP, Richter HE, Bradley CS, et al. Pelvic support, and pelvic symptoms and patient satisfaction after colpocleisis. Int Urogynecol J Pelvic Floor Dysfunct, 2008(19):1603-1609.
(收稿日期:2015-10-08)

