降钙素原和C反应蛋白在诊断脓毒症中的意义
李炅子,张术华,全 艳
(1.重庆市上清寺街道社区卫生服务中心 400015;2.重庆市东南医院 401336;3.重庆市杨家坪街道社区卫生服务中心 400050)
·临床研究·
降钙素原和C反应蛋白在诊断脓毒症中的意义
李炅子1,张术华2△,全 艳3
(1.重庆市上清寺街道社区卫生服务中心 400015;2.重庆市东南医院 401336;3.重庆市杨家坪街道社区卫生服务中心 400050)
目的 探讨降钙素原(PCT)和C反应蛋白(CRP)对脓毒症的诊断价值。方法 收集152例全身炎性反应综合征患者,分为脓毒症组和非脓毒症组,比较2组患者的PCT和CRP水平。结果 脓毒症组患者CRP和PCT水平(4.38)显著高于非脓毒症组(0.78),差异有统计学意义(P<0.05)。绘制受试者工作特征(ROC)曲线获得PCT曲线下面积(AUC)为0.792(95%CI0.657~0.873),CRP的AUC为0.687(95%CI0.574~0.806),在各自的临界点(PCT=1.8 ng/mL,CRP=2.75 mg/L),PCT和CRP诊断尿脓毒症的敏感性分别是0.684和0.256,特异性是0.818和0.952。感染性脓毒症患者PCT浓度在第1、7、20天呈趋势性降低。结论 PCT诊断脓毒症的敏感性高于CRP,且能预测感染性脓毒症患者的预后。
降钙素原; C反应蛋白; 脓毒症
脓毒症是由感染引起的全身性炎性反应综合征,是重症监护室导致患者发病和病死的主要因素,全球每年有大量患者病死于脓毒症[1-2]。脓毒症病情复杂,感染表征不尽相同。及时诊断和抗菌治疗对降低脓毒症引起的器官衰竭等并发症至关重要[3-4]。患者出现发热,白细胞增高,心率和呼吸率增加,但这些表征缺乏特异性不能单独用于疾病诊断,血液培养是公认的诊断金标准[5]。近年来研究显示,降钙素原(PCT)水平能很好地指示细菌感染[6-8]。C反应蛋白(CRP)是一种急性时相蛋白,直接参与炎性反应。现检测患者血清PCT和CRP水平,探讨其对脓毒症的早期诊断价值和预后。
1 资料与方法
1.1 一般资料 收集2013年6月至2015年6月3家医院全身炎性反应综合征(SIRS)患者152例,男61例,女75例,平均年龄(62.8±16.5)岁,将患者分成脓毒症组(68例)和非脓毒症组(86例)。按美国胸科医师学会和危重病医学(ACCP/SCCM)关于脓毒症指南和国际脓毒症诊断标准[9-10]。
1.2 方法 患者于24 h内静脉采血2 mL送检。PCT采用罗氏Elecsys BRAHMS检测,CRP使用免疫比浊法测定。24 h内对患者的可疑感染部位分别进行血培养、中段尿培养、腹腔引流液或痰培养。

2 结 果
脓毒症组患者有57例细菌培养呈阳性,包括大肠埃希菌 16例、铜绿假单胞菌10例、肺炎克雷伯菌8例、肠球菌5例、金黄色葡萄球菌13例、表皮葡萄球菌3例、不动杆菌1例、肠杆菌1例。细菌培养阳性患者第1、7、20天PCT水平呈明显下降趋势。脓毒症组和非脓毒症组PCT为4.38 ng/mL和0.78 ng/mL,CRP为8.73 ng/mL和2.45 mg/L,差异有统计学意义(P<0.05)。分别绘制PCT(1.8 ng/mL)和CRP(2.75 mg/L)ROC曲线,获得其敏感性、特异性和预测值。见表1、2和图1、2。
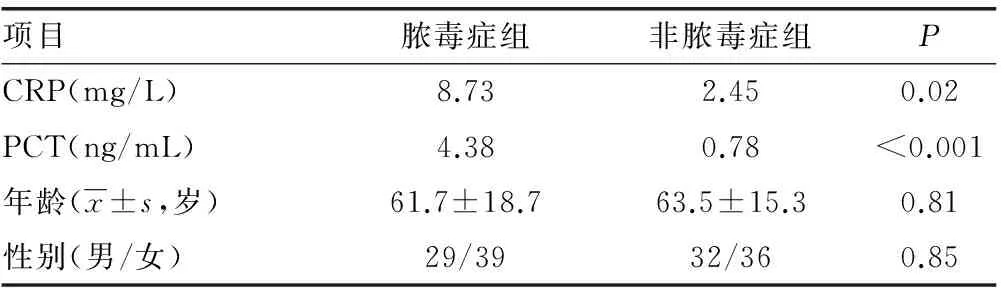
表1 2组患者临床资料和检测结果比较

图1 细菌感染引起的脓毒症患者血清PCT水平变化

图2 脓毒症组患者PCT和 CRP水平的ROC曲线

指标临界值95%CI敏感性特异性AUCYouden指数PCT(ng/mL)1.80.657~0.8730.6840.8180.7920.42CRP(mg/L)2.750.574~0.8060.2560.9520.6870.31
3 讨 论
PCT是降钙素的前体,由116个氨基酸组成[11]。PCT在外周血水平较低,主要由甲状腺和肺组织中的神经内分泌细胞释放,由炎性细胞因子刺激机体产生[12-13]。细菌感染后PCT增高,在非感染性系统炎性中也会升高[14-17]。
PCT检测结合其他临床感染指标,可判断患者预后[18-19]。CRP虽被用于诊断脓毒症,但作为脓毒症检测标志的性能仍存在争论[20-21]。本研究结果表明,脓毒症组患者PCT和CRP显著高于非脓毒症组,差异有统计学意义(P<0.05),PCT在细菌培养阳性的脓毒症患者中明显增高,与其他研究相似[22-24]。PCT和CRP均能用于诊断脓毒症。本研究ROC曲线结果显示,PCT在1.8 ng/mL时敏感性(0.684)和特异性(0.818)达到最佳。CRP在2.75 mg/L时具有较高的敏感性(0.952),但特异性(0.256)欠佳。PCT和CRP诊断脓毒症的AUC分别为0.792和0.687,提示PCT在诊断脓毒症具有更好的性能,与Castelli等[25]的研究结果类似。
本研究结果表明,患者在第1、7、20天细菌感染的脓毒症中PCT水平逐渐下降,说明PCT既能作为脓毒症预后的指标,也能判断感染患者的预后,但CRP不能反映患者预后[26]。CRP作为炎性指标在临床中应用最为广泛,但CRP对脓毒症患者是否具有良好的诊断性能仍然存在争议[27-28]。本研究结果显示,CRP能对脓毒症的诊断具有较高的敏感性,但特异性欠佳,在临床上应结合PCT对脓毒症进行准确诊断。
综上所述,PCT和CRP能够早期诊断脓毒症,反映患者感染状态时,PCT的特异性和敏感性比CRP高,具有更佳的诊断性能。细菌感染的脓毒症患者,PCT能预测预后,且CRP具有较高的敏感性。本研究样本量较少,需扩大样本量进行更深入的研究。
[1]Angus DC,Linde-Zwirble WT,Lidicker J,et al.Epidemiology of severe sepsis in the United States:analysis of incidence,outcome,and associated costs of care[J].Crit Care Med,2001,29(7):1303-1310.
[2]Prescott HC,Langa KM,Liu V,et al.Increased 1-year healthcare use in survivors of severe sepsis[J].Am J Respir Crit Care Med,2014,190(1):62-69.
[3]Seymour CW,Rea TD,Kahn JM,et al.Severe sepsis in pre-hospital emergency care:analysis of incidence,care,and outcome[J].Am J Respir Crit Care Med,2012,186(12):1264-1271.
[4]Dellinger RP,Levy MM,Rhodes A,et al.Surviving sepsis campaign:international guidelines for management of severe sepsis and septic shock:2012[J].Crit Care Med,2013,41(2):580-637.
[5]Giamarellos-Bourboulis EJ,Mega A,Grecka P,et al.Procalcitonin:a marker to clearly differentiate systemic inflammatory response syndrome and sepsis in the critically ill patient?[J].Intensive Care Med,2002,28(9):1351-1356.
[6]Kenneth LB.Richard snider and Eric S.nylen.procalcitonin in sepsis and systemic inflammation:a harmful biomarker and a therapeutic target[J].Br J Pharmacol,2010,159(2):253-264.
[7]Lee H.Procalcitonin as a biomarker of infectious diseases[J].Korean J Intern Med,2013,28(3):285-291.
[8] Faix JD.Biomarkers of sepsis[J].Crit Rev Clin Lab Sci,2013,50(11):23-36.
[9]Levy MM,Fink MP,Marshall JC,et al.2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference[J].Intensive Care Med,2003,29(4):530-538.
[10]Bone RC,Balk RA,Cerra FB,et al.Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis.The ACCP/SCCM Consensus Conference Committee.American College of Chest Physicians/Society of Critical Care Medicine[J].Chest,1992,101(6):1644-1655.
[11]Le Moullec JM,Jullienne A,Chenais J,et al.The complete sequence of human preprocalcitonin[J].FEBS Lett,1984,167(1):93-97.
[12]Snider RH,Nylen ES,Becker KL.Procalcitonin and its component peptides in systemic inflammation:immunochemical characterization[J].J Investig Med,1997,45(9):552-560.
[13]Dandona P,Nix D,Wilson MF,et al.Procalcitonin increase after endotoxin injection in normal subjects[J].J Clin Endocrinol Metab,1994,79(6):1605-1608.
[14]Maier M,Wutzler S,Lehnert M,et al.Serum procalcitonin levels in patients with multiple injuries including visceral trauma[J].J Trauma,2009,66(1):243-249.
[15]Picariello C,Lazzeri C,Chiostri M,et al.Procalcitonin in patients with acute coronary syndromes and cardiogenic shock submitted to percutaneous coronary intervention[J].Intern Emerg Med,2009,4(5):403-408.
[16]Schuetz P,Affolter B,Hunziker S,et al.Serum procalcitonin,C-reactive protein and white blood cell levels following hypothermia after cardiac arrest:a retrospective cohort study[J].Eur J Clin Invest,2010,40(4):376-381.
[17]Bonaci-Nikolic B,Jeremic I,Nikolic M,et al.High procalcitonin in a patient with drug hypersensitivity syndrome[J].Intern Med,2009,48(16):1471-1474.
[18]Bloos F,Marshall JC,Dellinger RP,et al.Multinational,observational study of procalcitonin in ICU patients with pneumonia requiring mechanical ventilation:a multicenter observational study[J].Crit Care,2011,15(2):R88.
[19]Giamarellos-Bourboulis EJ,Tsangaris I,Kanni T,et al.Procalcitonin as an early indicator of outcome in sepsis:a prospective observational study[J].J Hosp Infect,2011,77(1):58-63.
[20]Wyllie DH,Bowler IC,Peto TE.Bacteraemia prediction in emergency medical admissions:role of C reactive protein[J].J Clin Pathol,2005,58(4):352-356.
[21]Lee CC,Hong MY,Lee NY,et al.Pitfalls in using serum C-reactive protein to predict bacteremia in febrile adults in the ED[J].Am J Emerg Med,2012,30(4):562-569.
[22]Clech C,Ferriere F,Karoubi P,et al.Diagnostic and prognostic value of procalcitonin in patients with septic shock[J].Crit Care Med,2004,32(5):1166-1169.
[23]Brunkhorst FM,Wegscheider K,Forycki ZF,et al.Procalcitonin for early diagnosis and differentiation of SIRS,sepsis,severe sepsis,and septic shock[J].Intensive Care Med,2000,26(Suppl 2):S148-S152.
[24]Nakamura A,Wada H,Ikejiri M,et al.Efficacy of procalcitonin in the early diagnosis of bacterial infections in a critical care unit[J].Shock,2009,31(6):586-591.
[25]Castelli GP,Pognani C,Meisner M,et al.Procalcitonin and C-reactive protein during systemic inflammatory response syndrome,sepsis and organ dysfunction[J].Crit Care,2004,8(4):R234-R242.
[26]Bloos F,Marshall JC,Dellinger RP,et al.Multinational,observational study of procalcitonin in ICU patients with pneumonia requiring mechanical ventilation:a multicenter observational study[J].Crit Care,2011,15(2):R88.
[27]Ivaska L,Elenius V,Mononen I,et al.Discrepancies between plasma procalcitonin and C-reactive protein levels are common in acute illness[J].Acta Paediatr,2015,86(24):1889-1893.
[28]Standage SW,Wong HR.Biomarkers for pediatric sepsis and septic shock[J].Expert Rev Anti Infect Ther,2011,9(1):71-79.
10.3969/j.issn.1673-4130.2016.20.057
A
1673-4130(2016)20-2929-03
2016-02-16
2016-04-18)
△通讯作者,E-mail:326842927@qq.com。