Visual outcomes of Orbiflex K® lenses in patients with keratoconus
Berkay Akmaz, Ayse Yesim Oral, Baran Kandemir, Yusuf Ozerturk
Visual outcomes of Orbiflex K®lenses in patients with keratoconus
Berkay Akmaz1, Ayse Yesim Oral2, Baran Kandemir2, Yusuf Ozerturk2
1Department of Ophthalmology, Izmir Katip Celebi University, Ataturk Training and Research Hospital, Izmir 35360, Turkey
2Department of Ophthalmology, Lutfi Kirdar Kartal Training and Research Hospital, Istanbul 34890, Turkey
方法:选取研究对象为2012-11/2013-12在Dr. Lütfi Krdar Kartal培训和研究医院确诊为圆锥角膜的52例患者80眼。所有患者接受硬性角膜接触镜治疗,术后随访12mo。患者的平均年龄为26.1±6.9岁(范围:15~43岁)。患者依照Amsler-Krumeich分型以及各阶段角膜曲率值进行分组。在配戴角膜接触镜治疗前后进行裸眼视力(UCVA),最佳矫正视力(BCVA),主观验光,角膜形态,角膜曲率,中央角膜厚度和生物显微镜检查。
结果:角膜横轴屈光度(K1)平均值为50.25±4.17D,而角膜纵轴屈光度(K2)平均值为53.82±4.81D。K的平均值为52.03±4.42D。UCVA的平均值为1.31±0.21 LogMAR(Snellen 0.05±0.04),戴眼镜和戴角膜接触镜下BCVA的平均值分别为0.79±0.33 LogMAR(Snellen 0.21±0.17)和0.05±0.08 LogMAR(Snellen 0.91±0.13)。比较角膜接触镜治疗前后的视力结果,差异有统计学意义(P<0.001)。第1,2,3和4阶段圆锥角膜患者视力提高平均行数分别为5.18±1.38(范围:2~8)行,5.86±1.79(范围:2~8)行, 6.32±2.16(范围:3~9)行和6.92±2.35(范围:3~9)行。
结论:OrbiflexK®角膜接触镜显著地改善了所有阶段的圆锥角膜患者的视力。
•AIM: To evaluate the outcomes of Orbiflex K®(SwissLens SA, Prilly, Switzerland) contact lenses in the visual rehabilitation of patients with keratoconus at different disease stages.
•METHODS: This study included 80 eyes of 52 patients who were admitted to the eye clinic of Dr. Lütfi Krdar Kartal Training and Research Hospital between Nov. 2012 and Dec. 2013 with a diagnosis of keratoconus. All patients received a rigid contact lens prescription and were followed up for 12 months. The mean age of the patients was 26.1±6.9y (range:15-43y). The patients were grouped according to the Amsler-Krumeich classification and staging using their keratometric values. Uncorrected visual acuity (UCVA), best-corrected visual acuity (BCVA), subjective refraction, corneal topography, keratometry, central corneal thickness measurements, and biomicroscopic examination were performed for all eyes before and after contact lens application.
•RESULTS: The mean value of the flat meridian (K1) was 50.25±4.17 diopters (D), whereas the mean value of the vertical meridian (K2) was 53.82±4.81D. The mean K value was 52.03±4.42D. The mean UCVA was 1.31±0.21 logMAR (Snellen 0.05±0.04), and the mean BCVA while wearing spectacles and the contact lens were 0.79±0.33 logMAR (Snellen 0.21±0.17) and 0.05±0.08 logMAR (Snellen 0.91±0.13), respectively. Visual acuities were compared before and after contact lens application, and the differences were statistically significant (P<0.001). The mean line increases for stages 1, 2, 3, and 4 keratoconus groups were 5.18±1.38 (range: 2-8), 5.86±1.79 (range: 2-8), 6.32±2.16 (range: 3-9), and 6.92±2.35 (range: 3-9) lines, respectively.
•CONCLUSION: Orbiflex K®lens provide significant visual improvement in patients with keratoconus at all stages of the disease.
Keratoconus, contact lens, Orbiflex K®
INTRODUCTION
Keratoconus is usually a bilateral, asymmetric and progressive corneal disorder, resulting in myopia, irregular astigmatism and reduced vision related to central and paracentral corneal thinning, steepening and scarring. This ectatic condition commonly appears during the second decade of life and puberty, progressing until the fourth decade of life, when it usually stabilizes[1]. During the past two decades, new developments in visual rehabilitation of keratoconus have been introduced, including new contact lens designs, photorefractive keratectomy, collagen cross-linking, intrastromal corneal ring segments, phakic intraocular lenses, and penetrating or lamellar keratoplasty in advanced stages[2]. Placido disk-based corneal topography in combination with biomicroscopic examination is widely used in the diagnosis of keratoconus in daily practice. The development of new technologies, such as slit-scanning technologies, rotating Scheimpflug devices, and optical coherence tomography, makes it now possible to quantitatively measure the posterior corneal curvature, and to provide useful diagnostic information for the detection of keratoconus in a clinical setting[3-5].
In the early stages of keratoconus, vision can be managed with spectacles but as the disease progresses, rigid gas-permeable (RGP) contact lenses are preferred for reducing distortion and providing better vision[6-8]. Contact lenses are the main treatment modality in the treatment of keratoconus, and are the appropriate treatment option in 90% of keratoconus patients[9].When spectacles fail to improve visual acuity, contact lenses must be tried before exploring surgical options. Today, advances in surgical alternatives such as corneal ring segments, deep anterior lamellar keratoplasty and penetrating keratoplasty are considered to be efficient and permanent solutions by patients who do not know the advantages and disadvantages of surgery and contact lens use. However, we, as ophthalmologists, should inform patients that contact lenses are good alternative to improve visual acuity, but there is no evidence that it can stop the progression of keratoconus. Corneal Collagen Crosslinking (CXL) is a surgical procedure that stops the progression of the disease and can improve the visual acuity and contrast sensitivity in patients with keratoconus[10]. Many patients treated with CXL will benefit from using contact lens to improve their visual acuity.
In our study,we used a new model RGP lens in 52 patients (80 eyes) with keratoconus at different stages and evaluated their visual outcomes.
MATERIALS AND METHODS
This study included 80 eyes of 52 patients whowere admitted to the eye clinic of Dr. Lütfi Krdar Kartal Training and Research Hospital between Nov. 2012 and Dec. 2013 with a diagnosis of keratoconus at different disease stages. All patients who received a rigid contact lens prescription were followed up for 12 months.

Figure 1Orbiflex®K lens geometry.
Demographic data, including age, gender, indications for the use of the contact lens, autorefractometric measurements before and after contact lens application, best-corrected visual acuity (BCVA) and uncorrected visual acuity (UCVA), and topographic keratometric values, were recorded. Visual acuities were taken using Snellen acuity chart. Visual acuity data were converted from Snellen equivalent to logMAR. Based on the Amsler-Krumeich classification of keratoconus[11], stage 1 included 12 eyes with a keratometric value <48 diopters (D); stage 2 included 40 eyes with a keratometric value <53D; stage 3 included 10 eyes with a keratometric value >53D; and stage 4 included 18 eyes with a keratometric value >55D. Patients in all keratoconus stages were prescribed Orbiflex K®(SwissLens SA, Prilly, Switzerland) lens, and the values of logMAR BCVA before and after lens application for each group were compared statistically (paired sample t-test). Inter-group differences for this parameter were compared with one way analysis of variance (ANOVA).
Orbiflex K®RGP lenses are made of Boston XO (Hexafocon A) material. Geometrically, the anterior and posterior optic zones are spherical. Peripherally, the lens has a spherical structure with three basic curves (Figure 1). The transmissibility level (Dk/t) value is equal to 100, the posterior surface basic curves range from 5.5 to 7.5 mm (in 0.1 mm increments), and the lens diameter ranges from 8.70 to 9.20 mm (in 0.1 mm increments). The posterior vertex power reaches up to 40D with 0.25 intervals.
Before the application of the trial lenses, the mean keratometric measurements were calculated using the Sirius Corneal Topography device (Sirius, CSO, Florence, Italy). Keratometric values were converted to millimeters using a corneal refraction index of 1.3375. Lenses with a basic curvature value of 0.1 mm more vertical than the mean keratometric value were chosen as the initial trial contact lens. Twenty minutes later, the fit of the contact lens was evaluated using a biomicroscope to assess the lens-cornea relationship, fluorescein pattern, and movement and centralization of the lens. A three-point-touch fitting technique was used. We tried to find a lens that slightly touched the apical surface of the central cornea. After deciding on the accurate lens, the refraction examination with the contact lens was repeated and corrected. The dioptric power of the contact lens was calculated according to the final correction values, and final lens parameters were prescribed. Healthy contact lens wear and care were explained to the patients in detail. All contact lens examinations were made by the same physician (BA).
Routine control visits and examinations were performedat 1 week, 2 weeks, 6 months, and 1 year after commencing wear of the contact lens. At each visit, we recorded the following: refraction using an auto refractometer, BCVA with spectacles and contact lenses, position and movement of the lens, relationship between the cornea and the edge of the lens, and fluorescein pattern using a slit-lamp biomicroscope. Any complications were also recorded. Exclusion criteria for this study included corneal leukoma, a non-centralized contact lens, vernal conjunctivitis, and non-compliance. All procedures conformed to the tenets of the Declaration of Helsinki, and written informed consent was obtained from all subjects.
BCVA with contact lens at the first day were compared withat the 1 year follow-up statistically for each group (paired sample t test). Inter-group differences for this parameter were compared with ANOVA.
Statistical AnalysesStudy data were analyzed using SPSS 17.0 (SPSS, Chicago, IL, USA) software. Intra group comparisons were made by paired t-test and one way analysis of variance (ANOVA) for inter-group comparisons.P< 0.05 was considered to be statistically significant.
RESULTS
Eighty eyes of 52 patients (30 males, 22 females) with keratoconus were included in the study. A rigid contact lens (Orbiflex K®) was applied to all eyes, and patients were followed up for 12 months. The mean age was 26.1±6.9 (range: 15-43) years (Table 1). According to the Amsler-Krumeich keratoconus classification, 12 eyes were stage 1, 40 eyes were stage 2, 10 eyes were stage 3, and 18 eyes were stage 4 (Table 2).
The mean value ofthe flat meridian (K1) was 50.25±4.17D (range: 43.50-62.40D), whereas the mean vertical meridian (K2) was 53.82±4.81D (range: 46.91-66.02D) in the keratoconus patients. The mean K value was 52.03±4.42D (range: 45.36-64.21D) (Figure 2).
The mean best spectacle- and best contact lens-corrected visual acuity measurements of all keratoconus patients in all stages are given in Table 3. BCVA with contact lenses (0.04±0.88 logMAR) was significantly better than the uncorrected visual acuity (1.30±0.39 logMAR) for logMAR chart (P<0.001, paired samplest-test). Further, BCVA with contact lenses (0.04±0.88 logMAR) was also significantly higher than BCVA with spectacles (0.67±0.77 logMAR) for logMAR charts (P<0.001, paired samplest-test).
Average number of trials was 1.57 (range: 1-4). The best fitting contact lens was found at the first trial in 48 eyes (60%), at the second trial in 20 eyes (25%), at the third trial in 10 eyes (12.5%), at the fourth trial in 2 eyes (2.5%). The mean line gain in BCVA with the contact lenses was 6.08±2.56 (range: 3-9) lines in the Snellen chart compared with that in BCVA with spectacles. Of the 80 eyes, 74 (92.5%) increased by >3 lines in the Snellen chart. During the follow-up period, BCVA with contact lenses remained stable and unchanged (Table 4). The mean line increases for the stages 1, 2, 3, and 4 keratoconus groups were 5.18±1.38 (range: 2-8), 5.86±1.79 (range: 2-8), 6.32±2.16 (range: 3-9), and 6.92±2.35 (range: 3-9) lines, respectively (Figure 2).

Figure 2 The mean visual acuity measurements before and after contact lens application in different stages ofkeratoconusUVA: Uncorrected visual acuity; BCVA-S: Best-corrected visual acuity-spectacles; BCVA-CL: Best-corrected visual acuity-contact lenses.
Table 1Demographic and clinical characteristics of the patients

Numberofpatients52M30(50eyes)F22(30eyes)Mean±SDage(a)26.1±6.9
Table 2Classification of keratoconus

KeratoconusstageNo.(eye)Stage112Stage240Stage310Stage418
Table 3Visual acuity (logMAR) before and after rigid contact lenses wearing in different stages of keratoconus patients at the first day
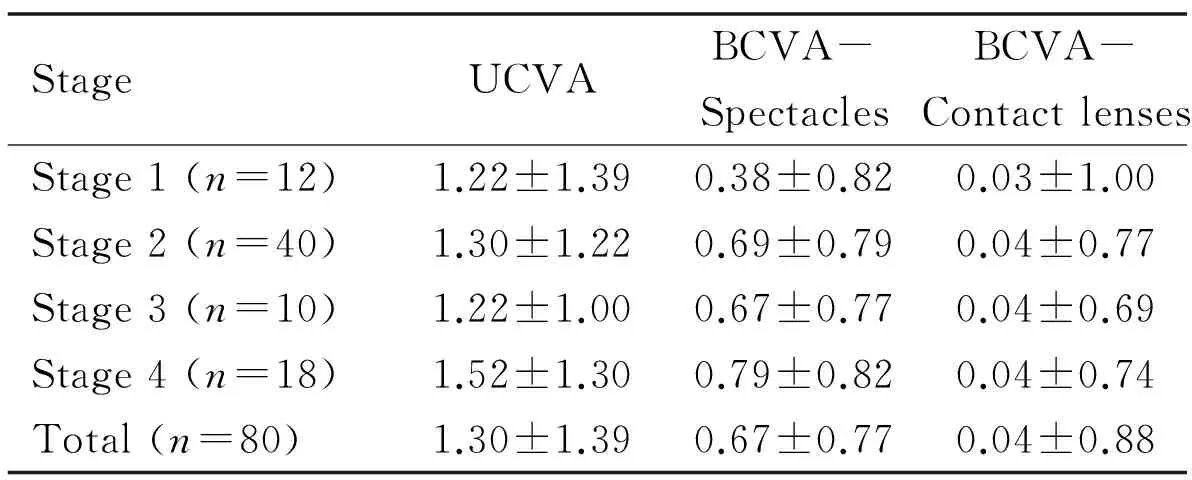
StageUCVABCVA-SpectaclesBCVA-ContactlensesStage1(n=12)1.22±1.390.38±0.820.03±1.00Stage2(n=40)1.30±1.220.69±0.790.04±0.77Stage3(n=10)1.22±1.000.67±0.770.04±0.69Stage4(n=18)1.52±1.300.79±0.820.04±0.74Total(n=80)1.30±1.390.67±0.770.04±0.88
UCVA: Uncorrected visual acuity; BCVA: Best corrected visual acuity.
The Snellen line gain with contact lenses was significantly higher in the stage 4 patients than in the other groups (one-way analysis of variance;P<0.05). BCVA did not change in any of the patients after contact lens application during the follow-up period.
Table 4Visual acuity (logMAR) before and after rigid contact lenses wearing in different stages of keratoconus patients at the first year
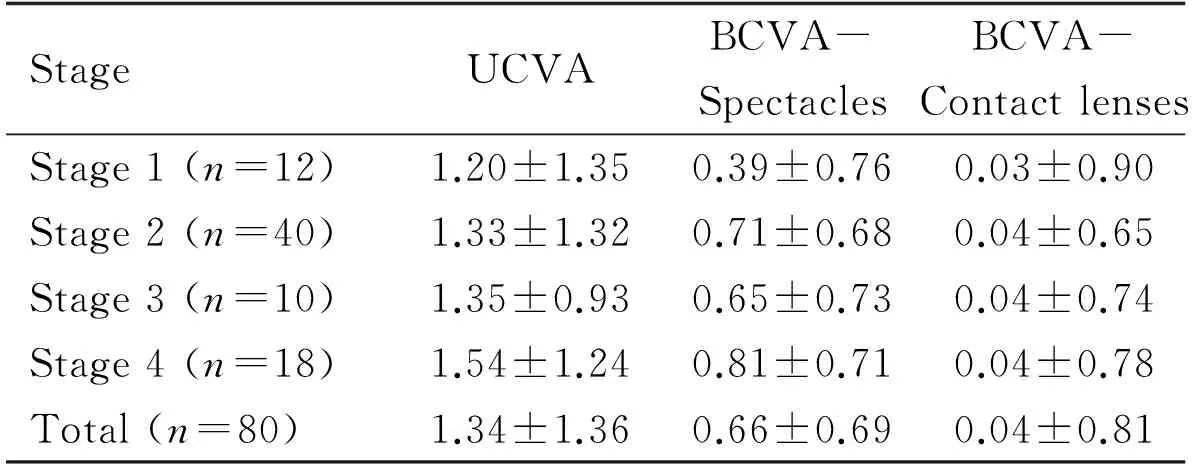
StageUCVABCVA-SpectaclesBCVA-ContactlensesStage1(n=12)1.20±1.350.39±0.760.03±0.90Stage2(n=40)1.33±1.320.71±0.680.04±0.65Stage3(n=10)1.35±0.930.65±0.730.04±0.74Stage4(n=18)1.54±1.240.81±0.710.04±0.78Total(n=80)1.34±1.360.66±0.690.04±0.81
UCVA: Uncorrected visual acuity; BCVA: Best corrected visual acuity.
DISCUSSION
In early stages ofkeratoconus, spectacles, soft CLs and even custom aberration-correcting soft CLs may be adequate to correct for vision changes. But as the keratoconus progresses, the optically smooth surface from a rigid gas permeable lens is necessary to ameliorate the irregular corneal surface of the ectatic eye to provide clearer vision. Corneal RGPs, and now more popularized scleral lenses, are the mainstay visual treatments for these eyes[12]. RGPs comprise 65% of contact lens correction for keratoconus and has delayed the need for surgery in approximately 80% to 98.9% of all fittings[13-15].Whereas the current treatments for ectasias revolve around visual rehabilitation, CXL is a promising treatment to actually delay and potentially halt the progression of many ectasias, including keratoconus. Considering all these treatments, rigid contact lenses are an alternative optic rehabilitation method that can successfully correct high corneal astigmatism in keratoconus patients who fail to achieve sufficient vision using glasses. Kazunoetal[16]stated in their study that contact lenses correct irregular optical surfaces of corneas, and provide acceptable vision for keratoconus patients. In addition, they showed that RGP contact lenses increase visual performance by reducing high-order aberrations in eyes with keratoconus.
In our study, BCVA with contact lens was found to be significantly better than BCVA with glasses in 80 eyes with keratoconus (P<0.001). Similarly, Yanaietal[17]established that the mean visual acuity was 0.70 logMAR (20/111) with glasses and 0.20 logMAR (20/29) with contact lenses. Cagiletal[18]reported that the mean BCVA was 0.40±0.19 logMAR with glasses and 0.14±0.11 logMAR with Rose K contact lenses in patients with keratoconus, and the difference was statistically significant (P=0.001). Further, Gunesetal[19]reported the efficacy of Rose K RGP contact lenses in patients with keratoconus. The mean BCVA with glasses in 31 eyes of 17 patients (5 early, 18 moderate, and 8 advanced stage) was 0.54±0.21 logMAR, whereas it improved to 0.04±0.09 logMAR following Rose K application. During the follow-up period in our study, the BCVA with contact lenses remained stable. The visual acuity increased immediately following contact lens fitting in most of the patients.
In our study,the increase in Snellen visual acuity following contact lens fitting was significantly larger in the advanced keratoconus patients than in the other groups (P<0.05). This may be due to lower initial visual acuity levels in the advanced group. Canetal[20]applied Rose K2 rigid lenses to 80 eyes of 47 keratoconus patients and found that the mean visual acuity was significantly higher with these lenses than with glasses; additionally, these lenses were more effective at improving visual acuity in both the moderate and severe keratoconus groups than in the mild group.
RGP contact lenses playan important role in improving visual acuity in irregular astigmatism and keratoconus; however, they have some practical difficulties. Firstly, they may decentralize easily because the cornea is flat at the upper part and vertical at the lower part. Moreover, many patients cannot tolerate RGP lenses due to a foreign body sensation and complaint about scratchy eyes, despite a good visual outcome. On the other hand, while soft contact lenses provide excellent comfort and physiological response, the visual rehabilitation outcome may not be as good as for rigid lenses[21].
Other contact lens options in keratoconus include scleral lenses, hybrid lenses, special soft lenses, and piggyback lens systems. The piggyback lens system comprises a RGP lens fitted onto a soft lens and can be successfully used in keratoconus patients; however, using two different lenses makes cleaning and disinfecting difficult[22].
Hybrid lenses are made of an RGP center, with a hydrogel periphery surrounding this center, and may be easily used in patients with astigmatism and keratoconus as they provide both comfort and good centralization. However, their lower oxygen permeability may lead to complications such as hypoxia and corneal neovascularization, which limit their indications[23]. Scleral lenses are also used in the treatment of keratoconus, but they are difficult to use and need more time for adaptation compared to corneal contact lenses. New generation scleral lenses are made from gas-permeable materials rather than polymethyl methacrylate (PMMA), and thus, their oxygen permeability is higher. Despite various drawbacks, this type of lens may be successfully used in patients for whom corneal contact lenses fail[24-27].
When previous studies on contact lenses in keratoconus patients are taken into account, it is clear that the most widely used lens is the RGP lens. Corneal RGP lens is the first lens of choice for visual improvement in patients with keratoconus[28]. Both Bettsetal[29]and Jainetal[30]reported 90% compliance rates for Rose K lenses in their studies, which evaluated visual performance and comfort. Ozkurtetal[31]also reported a 96% success rate using the same lenses. Mandatharaetal[32]the success rate of fitting Rose K lens in keratoconus was reported to be more than 90% and they have shown similar results in 95% patients with an average number of trials being 1.73 (range: 1-5) and in 95% of the cases, the final fit was achieved within the first three trials. In our study, we used a similar type of RGP contact lens (Orbiflex K®), and none of the patients stopped wearing them during the 1-year follow-up period (success rate, 100%). Further, no severe complications were observed. Two patients lost their lenses at the third and sixth months; new lenses were prescribed using the same parameters. Artificial tear drops were recommended in patients with gritty eye irritation.
As in all the other contact lenses, complications related to Orbiflex K®lenses included dry eye, keratitis, hypoxia-induced neovascularization, lens into lerance, and issues with centralization and stabilization of the lens. In our study, we did not observe any of these complications. In the long term, apical scarring may be seen in keratoconus[33]. In addition, corneal erosion due to direct physical trauma and hypoxia may lead to scarring in the central cornea. Several studies have reported that contact lenses may increase the possibility of apical scar formation[34],and Esginetal[35]found as 8.2% rate of apical scar development in keratoconus patients wearing RGP contact lenses during 33 months of follow-up. Moreover, Tunceretal[36]reported a 28.8% rate of apical scar development in keratoconus patients with a 7-year follow-up. In our study group, we observed no apical scarring or other complications during the 1-year follow-up. This may be due to the relatively shorter follow-up period and the higher Dk/t values (100 Dk/t) of the contact lenses used in our study. Keratoconus patients using any contact lenses should be monitored closely for such complications.
In conclusion, visual rehabilitation outcomes from the use of rigid contact lenses in keratoconus are promising compared with other treatment modalities. Rigid contact lenses are an effective method for correcting visual acuity, and area non-invasive and reversible method of treating keratoconus in certain patients.
1 Romero-Jiménez M, Santodomingo-Rubido J, Wolffsohn JS. Keratoconus: A review.ContLensAnteriorEye2010;33(4):157-166
2 Fadlallah A, Dirani A, El Rami H, Cherfane G, Jarade E. Safety and visual outcome of Visian toric ICL implantation after corneal collagen cross-linking in keratoconus.JRefractSurg2013;29:84-89
3 Ishii R, Kamiya K, Igarashi A, Shimizu K, Utsumi Y, Kumanomido T. Correlation of corneal elevation with severity of keratoconus by means of anterior and posterior topographic analysis.Cornea2012;31(3):253-258
4 Miha’ltz K, Kova’cs I, Taka’cs A, Nagy ZZ. Evaluation of keratometric, pachymetric, and elevation parameters of keratoconic corneas with Pentacam.Cornea2009;28(9):976-980
5 Kamiya K, Ishii R, Shimizu K, Igarashi A. Evaluation of corneal elevation, pachymetry and keratometry in keratoconic eyes with respect to the stage of Amsler-Krumeich classification.BrJOphthalmol2014;98(4):459-463
6 Jhanji V, Sharma N, Vajpayee RB. Management of keratoconus: current scenario.BrJOphthalmol2011;95:1044-1050
7 Barnett M, Mannis MJ. Contact lenses in the management of keratoconus.Cornea2011;30:1510-1516
8 Vazirani J, Basu S. Keratoconus: current perspectives.ClinOphthalmol2013;7:2019-2030
9 Rabinowitz YS. Keratoconus.SurvOphthalmol1998;42:297-319
10 Lamy R, Netto CF, Reis RG, Procopio B, Porco TC, Stewart JM, Dantas AM, Moraes HV Jr. Effects of corneal cross-linking on contrast sensitivity, visual acuity, and corneal topography in patients with keratoconus.Cornea2013;32(5):591-596
11 Alió JL, Shabayek MH. Corneal higher order aberrations: a method to grade keratoconus.JRefractSurg2006;22(6):539-545
12 Weed KH, MacEwen CJ, McGhee CN. The Dundee University Scottish Keratoconus Study II: a prospective study of optical and surgical correction.OphthalmicPhysiol2007;27(6):561-567
13 Kennedy RH, Bourne WM, Dyer JA. A 48-year clinical and epidemiologic study of keratoconus.AmJOphthalmol1986;101:267-273
14 Wagner H, Barr JT, Zadnik K. Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study: methods and findings to date.ContLensAnteriorEye2007;30(4):223-232
15 Bilgin LK, Yilmaz S, Araz B, Yüksel SB, Sezen T. 30 years of contact lens prescribing for keratoconic patients in Turkey.ContactLensAntEye2009;32(1):16-21
16 Negishi K, Kumanomido T, Utsumi Y, Tsubota K. Effect of high-order aberrations on visual function in keratoconic eyes with a rigid gas permeable contact lens.AmJOphthalmol2007;144(6):924-929
17 Yanai R, Ueda K, Nishida T. Retrospective analysis of vision correction and lens tolerance in keratoconus patients prescribed a contact lens with dual aspherical curves.EyeContactLens2010;36:86-89
20 Can ÇÜ. Keratokonuslu Olgularda Rose K2 Kontakt Lens Uygulama Sonuçlarmz.MNOphtalmology2008;15:10-13
21 Maguen E, Caroline P, Rosner IR, Macy JI, Nesburn AB. The use of SoftPerm lens for the correction of irregular astigmatism.CLAOJ1992;18(3):173-176
22 Giasson CJ, Perreault N, Brazeau D. Oxygen tension beneath piggyback contact lenses and clinical outcomes of users.CLAOJ2001;27:144-150
23 O’Donnell C, Maldonado-Codina C. A hyper-Dk piggyback contact lens system for keratoconus.EyeContactLens2004;30:44-48
24 Pullum KW, Whiting MA, Buckley R. Scleral contact lenses: the expanding role.Cornea2005;24:269-277
25 Segal O, Barkana Y, Hourovitz D, et al. Scleral contact lenses may help where other modalities fail.Cornea2003;22:308-310
26 Schornack MM, Patel SV. Scleral lenses in the management of keratoconus.EyeContactLens2010;36:39-44
27 Rathi VM, Mandathara PS, Dumpati S, Vaddavalli PK, Sangwan VS. Boston ocular surface prosthesis: An Indian experience.IndianJOphthalmol2011;59:279-281
28 Rathi, Varsha M., Preeji S. Mandathara, and Srikanth Dumpati. "Contact lens in keratoconus."IndianJophthalmol2013;61(8):410
29 Betts AM, Mitchell GL, Zadnik K. Visual performance and comfort with the Rose K lens for keratoconus.OptomVisSci2002;79:493-501
30 Jain AK, Sukhija J. Rose-K contact lens for keratoconus.IndianJOphthalmol2007;55:121-125
31 Ozkurt YB, Sengor T, Kurna S, Evciman T, Acikgoz S, Haboglu M, Aki S. Rose K contact lens fitting for keratoconus.IntOphthalmol2008;28(6):395-398
32 Mandathara Sudharman P, Rathi V, Dumapati S. Rose K lenses for keratoconus-An Indian experience.EyeContactLens2010;36:220-222
33 Krachmer JH, Feder RS, Belin MW. Keratoconus and related noninflammatory corneal thinning disorders.SurvOphthalmol1984;28:293-322
34 Korb DR, Finnemore VM, Herman JP. Apical changes and scarring in keratoconus as related to contact lens fitting techniques.JAmOptomAssoc1982;53:199-205
35 Esgin H, Erda N, Ozgur S. Keratokonuslu hastalarda cift eliptik kontakt lens uygulamas.MN-Oftalmoloji2002;9:44-47
36 Tuncer Z, Soylu T. Ileri Keratokonuslu Olgularda Kontakt Lens Uygulamas: Uzun Sureli Takip Sonuclarmz.TurkJOphthalmol. 2012;42:202-206
配戴Orbiflex K®角膜接触镜改善圆锥角膜患者视力的研究
Berkay Akmaz1, Ayse Yesim Oral2, Baran Kandemir2, Yusuf Ozerturk2
135360 土耳其伊兹密尔阿塔图尔克培训与研究医院伊兹密尔Katip Celebi大学眼科;234890 土耳其伊斯坦布尔Lutfi Kirdar Kartal培训与研究医院眼科)
Berkay Akmaz. 土耳其伊兹密尔阿塔图尔克培训与研究医院伊兹密尔Katip Celebi大学眼科. berkayakmaz@hotmail.com
目的:评估圆锥角膜患者配戴Orbiflex K®角膜接触镜在不同疾病阶段的视力康复结果。
圆锥形角膜;角膜接触镜;Orbiflex K®
Berkay Akmaz. Department of Ophthalmology, Izmir Katip Celebi University, Ataturk Training and Research Hospital, Izmir, Turkey.berkayakmaz@hotmail.com
2015-09-24Accepted: 2016-09-07
10.3980/j.issn.1672-5123.2016.11.05
Akmaz B, Oral AY, Kandemir B, Ozerturk Y. Visual outcomes of Orbiflex K®lenses in patients with keratoconus.GuojiYankeZazhi(IntEyeSci) 2016;16(11):2001-2005
引用:Akmaz B, Oral AY, Kandemir B, Ozerturk Y. 配戴Orbiflex K®角膜接触镜改善圆锥角膜患者视力的研究.国际眼科杂志2016;16(11):2001-2005