氟比洛芬酯在甲状腺手术中的应用
谭文斐,金 凤,崔 湧,田阿勇,马 虹,吕黄伟
氟比洛芬酯在甲状腺手术中的应用
谭文斐*,金凤,崔湧,田阿勇,马虹,吕黄伟
目的探讨氟比洛芬酯治疗甲状腺手术术后头痛的有效性。方法86例择期行甲状腺手术的患者随机分为2组:对照组(43例):全麻拔管前给予生理盐水,氟比洛芬酯组(43例):全麻拔管前共计给予氟比洛芬酯100 mg。术后24、48 h随访,根据VAS评分(视觉疼痛模拟评分)两次评分均值>4分诊断为术后头痛。结果两组患者术后切口疼痛24、48 h VAS评分比较差异无统计学意义(P>0.05);对照组发生术后头痛10例(23.3%),氟比洛芬酯组发生术后头痛2例(4.7%),两组比较差异有统计学意义(P<0.05)。结论术中应用氟比洛芬酯可以缓解甲状腺手术术后头痛。
甲状腺切除术;术后头痛;氟比洛芬酯
0 引言
随着甲状腺疾病发病率的增加,超声诊断技术的提高,越来越多的患者接受外科手术治疗甲状腺疾病。有研究者应用机器人手术辅助系统完成甲状腺手术[1],且可以应用仪器实时完成喉返神经的监测[2]。此外,麻醉药物的选择也为患者安全舒适的度过围手术期提供了更多的保障[3-4]。
已有文献探讨甲状腺手术后头痛的原因和体位改良[5],但围术期麻醉管理方案的变化,能否改善患者术后头痛的症状并未见报道。虽然麻醉医生擅长应用强效的阿片类药物为患者解除围术期强烈的切口疼痛,但是甲状腺手术术后的头痛无论从疼痛的程度还是疼痛的性质,都不同于以往外科手术后疼痛。本文旨在通过随机双盲对照的临床研究,探讨预防性应用氟比洛芬酯是否能够改善甲状腺手术术后头痛。
1 资料与方法
1.1一般资料选择2014年1-12月在我院行甲状腺手术患者86例。本研究经我院伦理委员会批准。患者自愿加入临床研究并且签署知情同意书。86例患者按照随机数字表法分为2组。氟比洛芬酯组43例,分别于切皮后、拔出气管导管前给予氟比洛芬酯(北京泰德制药有限公司)50 mg静注;对照组43例,分别于切皮后、拔出气管导管前给予生理盐水5 mL静注。患者和术后随访研究人员对给药情况双盲。排除标准:长期服用非甾体类抗炎药物;术前并存严重心脑疾病病史;年龄超过65岁。
1.2方法
1.2.1麻醉方法两组麻醉方法相同:入室常规心电图、无创袖带压、脉搏血氧饱和度、脑电双频指数(BIS)监测。麻醉诱导药物:咪达唑仑0.04 mg/kg,顺式阿曲库铵0.2 mg/kg,依托咪酯0.3 mg/kg,舒芬太尼0.6 μg/kg。麻醉诱导后行气管插管,术中机械通气,麻醉维持丙泊酚4~6 mg/(kg·h),瑞芬太尼 0.1~0.5 μg/(kg·min),七氟烷呼气末浓度1.5~2 MAC,BIS值40~60。
1.2.2术后头痛诊断标准疼痛视觉模拟评分(VAS):1~3分为轻度疼痛,4~6分为中度疼痛,7~10分为重度疼痛。术后24、48 h两次随访术后头痛情况,根据VAS评分均值>4分诊断为术后头痛。

2 结果
2.1两组患者一般情况比较两组患者性别构成、年龄、身高、体重、手术时间和舒芬太尼用量比较差异无统计学意义(P>0.05)。见表1。

表1 两组患者一般情况比较(例)
2.2两组患者术后VAS评分比较两组患者术后24、48 h VAS评分差异无统计学意义(P>0.05)。按照本研究定义,根据VAS评分2次均值>4分诊断为术后头痛,对照组发生术后头痛10例,氟比洛芬酯组2例,两组比较差异有统计学意义(P<0.05)。见表2。
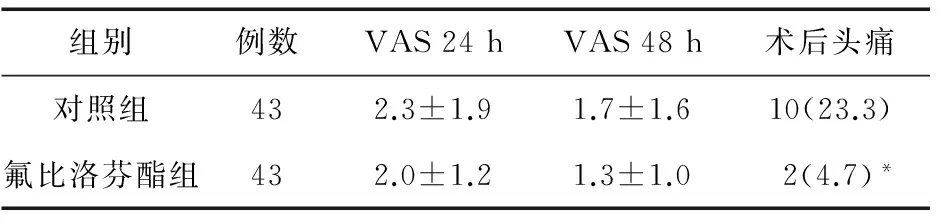
表2 两组患者术后VAS评分和头痛情况比较(例,%)
注:*与对照组比较,P<0.05
3 讨论
甲状腺疾病发病率不断增加,术后并发症也越来越受到重视。手术后头痛的原因已有文献报道,患者焦虑的精神状态、颈部过度伸展、颈静脉回流障碍、手术牵拉神经反射等因素[6]都可能造成术后头痛。但围术期麻醉管理方案是否影响手术后头痛未见文献报道。本研究发现,氟比洛芬酯组患者术后头痛发生率低于对照组,为临床麻醉工作中药物选择提供了理论根据。
氟比洛芬酯是一种可以静脉注射的具有靶向镇痛作用的非甾体类抗炎药物[7-8]。氟比洛芬是一种非选择性的环氧化酶抑制剂,通过减少前列腺素合成、减轻术区炎性反应而起到镇痛作用[9-12]。而氟比洛芬酯是氟比洛芬的前体药,其以脂微球作为载体,具有向炎症及创伤组织聚集的靶向性,广泛用于术后镇痛。甲状腺手术后头痛的机制较复杂,体位、血管、神经因素均有可能参与其中,而应用非选择性的环氧化酶抑制剂可以减轻手术后炎性反应,很好地缓解了这种特殊性质的术后并发症。
综上所述,甲状腺手术术中给予非选择性环氧化酶抑制剂氟比洛芬酯,可以改善患者术后头痛,提高麻醉质量,不失为临床工作中一个有效的选择。
[1]Shah SB,Hariharan U,Kulkarni A,et al.Anaesthesia for robotic thyroidectomy for thyroid cancer and review of literature[J].Indian J Anaesth,2016,60(1):55-57.
[2]Pachuski J,Vaida S,Donahue K,et al.Effect of laryngotracheal topical anesthesia on recurrent laryngeal nerve monitoring during thyroid Surgery[J].J Clin Anesth,2016,29:10-13.
[3]Lim H,Doo AR,Son JS,et al.Effects of intraoperative single bolus fentanyl administration and remifentanil infusion on postoperative nausea and vomiting[J].Korean J Anesthesiol,2016,69(1):51-56.
[4]Santosh BS,Mehandale SG.Does dexmedetomidine improve analgesia of superficial cervical plexus block for thyroid surgery[J].Indian J Anaesth,2016,60(1):34-38.
[5]Wattier JM,Caiazzo R,Andrieu G,et al.Chronic post-thyroidectomy pain:incidence,typology,and risk factors[J].Anaesth Crit Care Pain Med,2016,35(3):197-201.
[6]Han DW,Koo BN,Chung WY,et al.Preoperative greater occipital nerve block in total thyroidectomy patients can reduce postoperative occipital headache and posterior neck pain[J].Thyroid,2006,16(6):599-603.
[7]Su C,Su Y,Chou CW,et al.Intravenous flurbiprofen for post-thymectomy pain relief in patients with myasthenia gravis[J].J Cardiothorac Surg,2012,7:98.
[8]Yamashita K,Fukusaki M,Ando Y,et al.Preoperative administration of intravenous flurbiprofen axetil reduces postoperative pain for spinal fusion surgery[J].J Anesth,2006,20(2):92-95.
[9]Lin X,Zhang R,Xing J,et al.Flurbiprofen axetil reduces postoperative sufentanil consumption and enhances postoperative analgesic effects in patients with colorectal cancer surgery[J].Int J Clin Exp Med,2014,7(12):4887-4896.
[10]Wu TT,Wang ZG,Ou WL,et al.Intravenous flurbiprofen axetil enhances analgesic effect of opioids in patients with refractory cancer pain by increasing plasma beta-endorphin[J].Asian Pac J Cancer Prev,2014,15(24):10855-10860.
[11]Yang YG,Hu LH,Chen H,et al.Target-controlled infusion of remifentanil with or without flurbiprofen axetil in sedation for extracorporeal shock wave lithotripsy of pancreatic stones:a prospective,open-label,randomized controlled trial[J].BMC Anesthesiol,2015,15:161.
[12]Zhang L,Zhu J,Xu L,et al.Efficacy and safety of flurbiprofen axetil in the prevention of pain on propofol injection:a systematic review and meta-analysis[J].Med Sci Monit,2014,20:995-1002.
Application of flurbiprofen axetil in thyroidectomy
TAN Wen-fei*,JIN Feng,CUI Yong,TIAN A-yong,MA Hong,LÜ Huang-wei
(Department of Anesthesiology,the First Hospital of China Medical University,Shenyang 110001,China)
ObjectiveTo investigate the effect of flurbiprofen axetil on postoperative headache induced by thyroidectomy.MethodsEighty-six patients were divided into two groups randomly.All the patients underwent general anesthesia,and patients in control group and flurbiprofen axetil group were given sodium chloride injection and flurbiprofen axetil 100 mg.The visual analogue scale (VAS) score was recorded at 24 and 48 h after operation.Postoperative headache was diagnosed when VAS>4.ResultsThere was no significant difference in VAS scores between the two groups at 24 and 48 h after treatment (P>0.05).10 cases (23.3%) of control group,and 2 cases (4.7%) in flurbiprofen axetil group had postoperative headache,there being significant difference between the two groups (P<0.05).ConclusionAdministration of flurbiprofen axetil during operation can release postoperative headache induced by thyroidectomy.
Thyroidectomy;Postoperative headache;Flurbiprofen axetil
2016-03-23
中国医科大学第一医院麻醉科,沈阳 110001
辽宁省自然科学基金(2014021035)
10.14053/j.cnki.ppcr.201609020

