广东省梅州市24 450例女性HPV感染与基因分型
赵平森 贾润清 林利芳 苏鲁贤 钟志雄 曾毅
广东省梅州市24 450例女性HPV感染与基因分型
赵平森贾润清林利芳苏鲁贤钟志雄曾毅
514031 广东,梅州市人民医院 中山大学附属梅州医院(赵平森、林利芳、苏鲁贤、钟志雄);100124 北京工业大学 生命科学与生物工程学院 (贾润清、曾毅)
赵平森、贾润清为共同第一作者
【摘要】目的探讨梅州地区女性HPV感染情况与基因亚型分布,为该地区宫颈癌的预防和治疗提供数据资料。方法运用导流杂交基因芯片技术对24 450例就诊女性的宫颈脱落细胞标本进行HPV基因分型检测,并对HPV基因亚型感染情况进行对比分析。结果24 450例标本中检测出HPV阳性者3 922例,感染率为16.04%。在阳性标本中,HPV高危型阳性率最高的前3位依次是HPV-16(30.37%)、HPV-52(17.77%)和HPV-58(15.53%),低危型以HPV-CP8304为主(5.61%)。30~50岁是HPV感染的高峰年龄段,HPV阳性检出率在各年龄组的差异有统计学意义(P<0.001)。结论梅州地区就诊女性最常见的HPV亚型是16型,30~50岁是HPV感染高发人群,HPV基因分型对宫颈癌的预防和治疗具有积极的指导意义。
【主题词】乳头瘤状病毒,人;导流杂交;基因分型
Fundprograms:NaturalScienceFoundationofGuangdongProvinceofChina(2014A030307042);NationalScienceandTechnologyMajorProjectofChina“SignificantNewDrugsDevelopment”(2015ZX09102025)
人乳头瘤病毒(humanpapillomavirus,HPV)是球形DNA病毒,具有高度组织嗜性,可引起人体皮肤和黏膜异常增生[1]。HPV自20世纪70年代被发现与宫颈癌相关以来,一直备受关注。研究发现,HPV是宫颈鳞癌的主要致病因素[2]。至今已发现的HPV有100多个亚型,分为高危型(HR-HPV:如HPV-16和HPV-18)和低危型(LR-HPV:如HPV-6和HPV-11),各亚型与体内特定感染部位和病变有关,高危型HPV持续感染是宫颈癌及癌前病变发生的必要条件,约99.8%的宫颈癌患者为高危型HPV感染[3-5]。因此,在女性中检测HPV对于宫颈癌的早期诊疗具有重要的意义,同时为该地区的HPV疫苗研发提供重要的参考资料。本研究对来我院妇科就诊的24 450例患者HPV感染情况及基因亚型分布进行流行病学回顾性分析。
1资料与方法
1.1样本采集与保存收集2008年2月至2013年12月在梅州市人民医院妇科就诊的24 450例HPV女性检测者,年龄13~88岁,平均年龄(41.3±9.8)岁。由医生采集宫颈脱落细胞,将其放入加有专用细胞保存液的取样管中。样本采集后放置于4 ℃保存,24h内测定。
1.2试剂和仪器21种HPV分型检测试剂盒(包含HPV-DNA抽提试剂、PCR扩增试剂和杂交试剂)购自凯普生物、PCR扩增仪为RocheLightCycler480、医用核酸分子快速杂交仪购自凯普生物。
1.3检测方法DNA提取所采集的样本振荡混匀,取500μl,14 000rpm离心1min,弃上清,按HPV-DNA抽提试剂说明书指导抽提DNA。PCR扩增将上述抽提的DNA作为模板进行扩增,每份PCR反应体系为25μl,反应程序参考试剂说明。PCR产物杂交和显色按杂交试剂说明进行。结果判定:阳性为清晰可见的蓝紫色圆点,根据膜条HPV分型分布图,判断阳性点的HPV亚型,多个圆点代表多重感染,每次杂交试验均设置阴性与阳性对照。
1.4统计学方法数据统计采用GrapgPadPrismv5.0进行,计数资料和计量资料分别用χ2检验(%)和t检测,P<0.05为差异具有统计学意义。
2结果
2.1HPV基因分型检出情况24 450例标本中有3 922例感染HPV,感染率为16.04%。在3 922例阳性标本中,单一高危型感染有2 923例,占74.53%(2 923/3 922);单一低危型感染有367例,占9.36%(367/3 922);多重感染有632例,占16.11%(632/3 922),主要以高危型多重感染为主,占11.45%(449/3 922),如表1。
2.2阳性标本的HPV亚型分布在3 922例阳性标本中可检测到21种亚型HPV的分布,其中高危型阳性率最高的3种亚型分别为HPV-16(30.37%),HPV-52(17.77%),HPV-58(15.53%),低危型以HPV-CP8304为主(5.61%),如表2。
2.3HPV感染者年龄分布本研究所收集的病例中,年龄最小的为13岁,年龄最大的为88岁。将24 450例标本按患者年龄进行分组,显示不同年龄组HPV阳性检出率差异有统计学意义χ2=88.38,P<0.001(表3)。
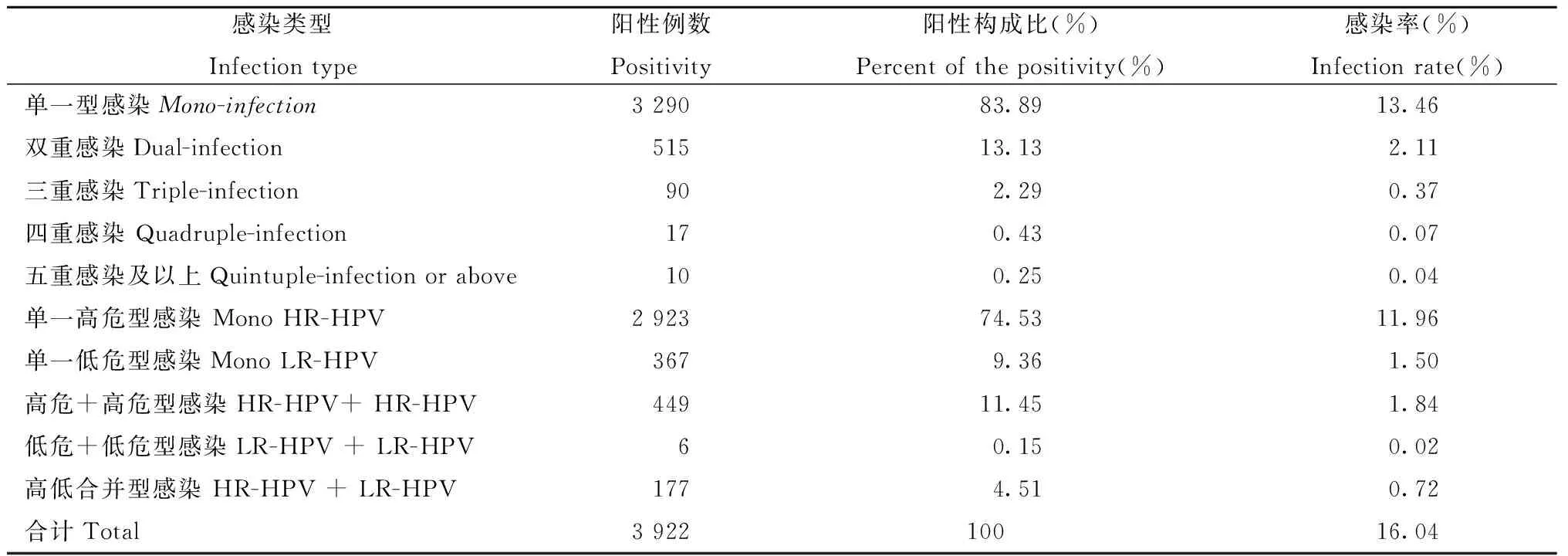
表1 24 450份标本HPV基因型检出情况
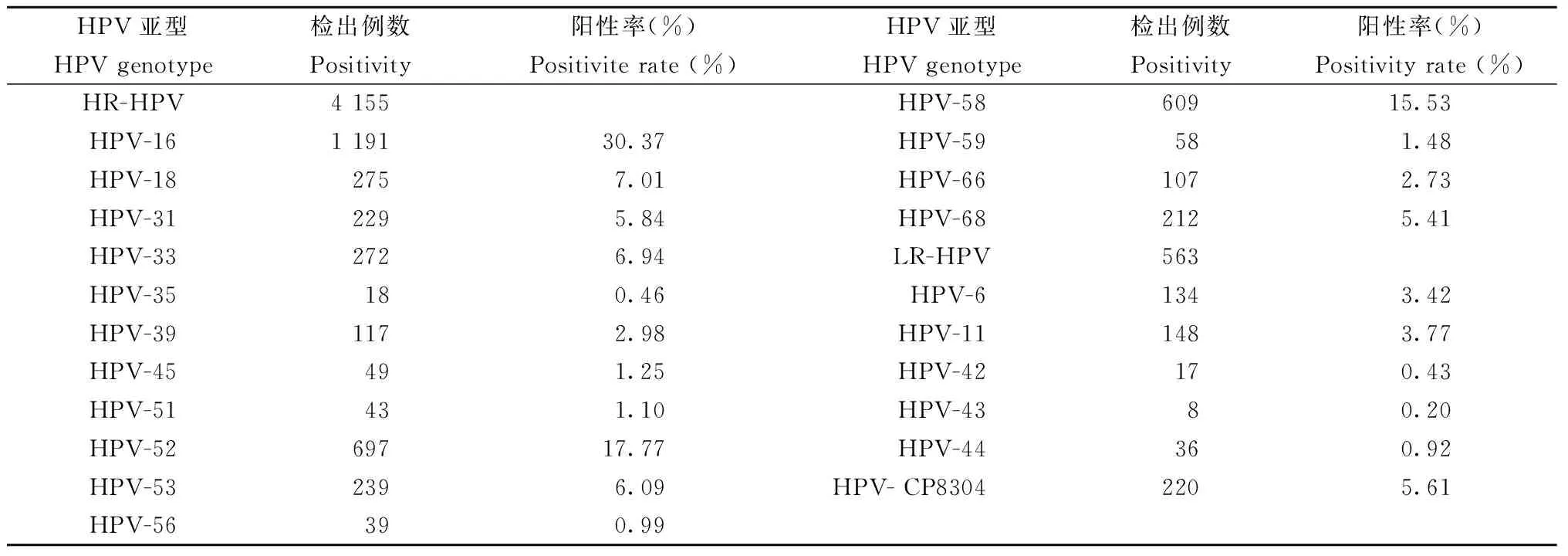
表2 3 922例阳性标本的HPV基因亚型分布
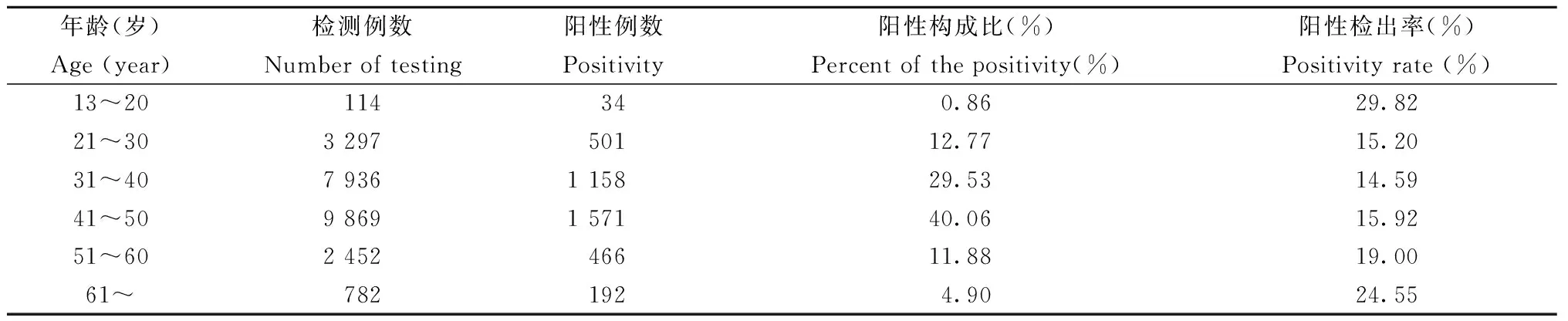
表3 24 450例标本的年龄分布和HPV阳性率
3讨论
宫颈癌是常见的妇科恶性肿瘤之一,发病率居全球妇科恶性肿瘤第二位,仅次于乳腺癌[6, 7]。相比于其他肿瘤,宫颈癌病因相对明确。近年来,宫颈癌及癌前病变发生率在全球范围内呈逐渐上升的趋势。流行病学和基础研究已证实,宫颈持续的高危型HPV感染是宫颈上皮内瘤变和宫颈癌的主要病因[8]。因此,对HPV基因的早期分型检测,能够及时发现宫颈病变并进行治疗,以降低宫颈癌的发病率和病死率。目前,国际上许多国家已将HPV基因分型检测纳入到女性宫颈癌前筛查计划中。
本研究对梅州市24 450例就诊女性HPV感染情况及基因亚型分布进行流行病学回顾性分析,结果显示感染率为16.04%。单一型感染(83.89%)远高于多重感染,说明该地区HPV可能多为单一型感染;另外,单一高危型感染占74.53%,远高于单一低危型感染(9.36%)、高危型合并感染(11.45%)、低危型合并感染(0.15%)和高低合并型感染(4.51%),说明该地区HPV感染可能多为单一型感染且以单一高危型感染为主。持续的HPV高危型感染是宫颈上皮内瘤变和宫颈癌发生的一个首要条件[8],
在本研究中, 21种亚型的HPV均有分布,HPV高危型阳性率最高的前3个依次是HPV-16、HPV-52和HPV-58,CP8304在低危型HPV感染中阳性率最高,与Zou等[9]报道的结果相一致。现已公认高危型HPV感染可引起宫颈癌前病变与宫颈癌,但在不同国家和地区,HPV分型的流行病学分布不同[10-13]。因此,基于HPV亚型的流行与分布数据可为高风险人群制订有针对性的疫苗接种方案,为防治宫颈癌提供有价值的资料。本研究发现不同年龄组的HPV阳性检出率有显著性差异。13~20岁组的HPV阳性检出率高于其他年龄组,提示HPV感染有年轻化的趋势。而且31~40岁组和41~50岁组HPV感染阳性构成比高于其他年龄组,提示该地区HPV感染的高峰年龄段是30~50岁。因此,应加强对此年龄段女性HPV基因分型检测普查力度。
综上所述,本研究可了解梅州地区就诊女性HPV感染情况及基因亚型分布,为HPV疫苗的研制和应用及宫颈癌预防提供重要的参考资料。
4参考文献
[1]Donders GG, Gabrovska M, Bellen G, et al. Knowledge of cervix cancer, human papilloma virus (HPV) and HPV vaccination at the moment of introduction of the vaccine in women in Belgium[J]. Arch Gynecol Obstet, 2008, 277 (4):291-298. doi:10.1007/s00404-007-0487-1.
[2]Walboomers JM, Jacobs MV, Manos MM, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide[J]. J Pathol, 1999, 189 (1):12-19.doi:10.1002/(SICI)1096-9896(199909)189:1<12::AID-PATH431>3.0.CO;2-F.
[3]Schiffman M, Castle PE. Human papillomavirus: epidemiology and public health[J]. Arch Pathol Lab Med, 2003, 127 (8):930-934. doi:10.1043/1543-2165(2003)127<930:HPEAPH>2.0.CO;2.
[4]Tarkkanen J, Auvinen E, Nieminen P, et al. HPV DNA testing as an adjunct in the management of patients with low grade cytological lesions in Finland[J]. Acta Obstet Gynecol Scand, 2007, 86 (3):367-372. doi:10.1080/00016340601185343.
[5]Ribeiro J, Teixeira D, Marinho-Dias J, et al. Characterization of human papillomavirus genotypes and HPV-16 physical status in cervical neoplasias of women from northern Portugal[J]. Int J Gynaecol Obstet, 2014, 125 (2):107-110. doi:10.1016/j.ijgo.2013.10.011.
[6]Munoz N, Castellsague X, de Gonzalez AB, et al. Chapter 1: HPV in the etiology of human cancer[J]. Vaccine, 2006, 24 Suppl 3:S3/1-10. doi:10.1016/j.vaccine.2006.05.115.
[7]Bosch FX, Manos MM, Munoz N, et al. Prevalence of human papillomavirus in cervical cancer: a worldwide perspective. International biological study on cervical cancer (IBSCC) Study Group[J]. J Natl Cancer Inst, 1995, 87 (11):796-802.doi: 10.1093/jnci/87.11.796.
[8]Huang MZ, Li HB, Nie XM, et al. An analysis on the combination expression of HPV L1 capsid protein and p16INK4a in cervical lesions[J]. Diagn Cytopathol, 2010, 38 (8):573-578.doi: 10.1002/dc.212580
[9]Zou H, Sun Y, Zhang G, et al. Positivity and incidence of human papillomavirus in women attending gynecological department of a major comprehensive hospital in Kunming, China 2012-2014[J]. J Med Virol, 2016, 88 (4):703-711.doi: 10.1002/jmv.24377.
[10]Anttila A, Pukkala E, Soderman B, et al. Effect of organised screening on cervical cancer incidence and mortality in Finland, 1963-1995: recent increase in cervical cancer incidence[J]. Int J Cancer, 1999, 83 (1):59-65. doi:10.1002/(SICI)1097-0215(19990924)83:1<59::AID-IJC12>3.0.CO;2-N.
[11]Hou R, Xu C, Zhang S, et al. Distribution of human papillomavirus genotype and cervical neoplasia among women with abnormal cytology in Beijing, China[J]. Int J Gynaecol Obstet, 2012, 119 (3):257-261.doi: 10.1016/j.ijgo.2012.07.011.
[12]Liu W, Wu EQ, Yu XH, et al. Detection of human papillomavirus genotypes associated with mucopurulent cervicitis and cervical cancer in Changchun, China[J]. Int J Gynaecol Obstet, 2012, 120 (2):124-126. doi:10.1016/j.ijgo.2012.07.032.
[13]Clifford GM, Gallus S, Herrero R, et al. Worldwide distribution of human papillomavirus types in cytologically normal women in the International Agency for Research on Cancer HPV prevalence surveys: a pooled analysis[J]. Lancet, 2005, 366 (9490):991-998.doi: 10.1016/s0140-6736(05)67069-9.
通信作者:赵平森,Email:zhaopingsen01@163.com,zhaopingsen@hotmail.com
DOI:10.3760/cma.j.issn.1003-9279.2016.03.014
基金项目:广东省自然科学基金(2014A030307042);国家科技重大专项“重大新药创制”(2015ZX09102025)
(收稿日期:2016-01-20)
Infection status of human papillomavirus and its genotype distribution among 24 450 women in Meizhou, Guangdong province
ZhaoPingsen,JiaRunqing,LinLifang,SuLuxian,ZhongZhixiong,ZengYi
MeizhouPeople′sHospital,MeizhouHospitalAffiliatedtoSunYat-senUniversity,Meizhou514031,China(ZhaoPS,LinLF,SuLX,ZhongZX);CollegeofLifeScienceandBioengineering,BeijingUniversityofTechnology,Beijing100124,China(JiaRQ,ZengY)ZhaoPingsenandJiaRunqingarethefurstauthorswhocontributedequallytothearticleCorrespondingauthor:ZhaoPingsen,Email:zhaopingsen01@163.com,zhaopingsen@hotmail.com
【Abstract】ObjectiveTo investigate the situation of human papillomavirus (HPV) infection and the distribution of HPV genotypes among women attending hospital in Meizhou, Guangdong province.MethodsFlow-through hybridization and gene chip technique was used to detect HPV in cervical exfoliated cell specimens collected from 24 450 women for HPV screening in Department of Gynecology, Meizhou People′s Hospital, Meizhou Hospital Affiliated to Sun Yat-sen University, and then the situation of HPV infection and distribution of HPV genotypes were analyzed. ResultsAmong 24 450 female exfoliated cell specimens, 3 922 were found to be positive for HPV infection, with the total infection rate of 16.04%. Among 3 922 samples, the top three high-risk subtypes of HPV were HPV-16 (30.37%), HPV-52 (17.77%) and HPV-58 (15.53%), the majority of low-risk HPV was HPV-CP8304 (5.61%). The positivity of various HPV types peaked among 30-50 years old. The differences of the HPV positive rates in different age groups was statistical significance (P<0.001). ConclusionsThe majority of women attending hospital detected with HPV-16 in Meizhou and the positivity of various HPV types peaked among women aged 30-50 years. Genotyping of HPV was meaningful for preventing and treating cervical cancer.
【Key words】Human papillomavirus; Flow-through hybridization; Genotyping
·病毒病诊断与治疗·