Ultrasound diagnosis of diverticulitis
Ultrasound diagnosis of diverticulitis
Michael E.Abboud, Sarah E.Frasure, Michael B.Stone
Emergency Department, Harvard University, 45 Francis St Neville House - 236A, Boston, Massachusetts 02115, USA
World J Emerg Med 2016;7(1):74–76
INTRODUCTION
Diverticular disease accounts for approximately 312 000 hospital admissions in the United States annually, and costs nearly 2.6 billion dollars.[1,2]Approximately 20% of Americans with diverticular disease will experience at least one episode of acute diverticulitis, necessitating a visit to their physician's office or the emergency department (ED) for treatment.[3]As the risk of developing diverticulitis rises with age (nearly 50% of people aged over 60 years have colonic diverticula), the incidence is rising as the elderly population grows.[4]The majority of the patients are treated non-operatively, with a course of oral antibiotics and diet modification.Although computed tomography (CT) imaging is considered the "gold standard" for the diagnosis of acute diverticulitis in the United States, ultrasound is routinely used in Europe, Asia, and Africa as the initial imaging modality of choice in the evaluation of patients with suspected diverticulitis.Recent studies[5,6]have suggested that there is no significant difference in the test performance characteristics of CT as opposed to ultrasound for the diagnosis of diverticulitis.We present two cases in which point-of-care ultrasound was used to diagnose acute uncomplicated diverticulitis in the ED.C
ase 1
A 30-year-old man with no significant history of medication or surgery presented to the ED because of abdominal pain for several days.He stated that the pain began four days before presentation after breakfast at home, and subsequently deteriorated as a constant, non-radiating pressure.There were no alleviating or aggravating factors.The patient had no history of similar abdominal pain, nor nausea, vomiting, hematemesis, change in bowel habits, fever, anorexia, dysuria, testicular pain, back pain, or rash.
On presentation, his temperature was 98.1 °F, heart rate 77 beats per minute, blood pressure 143/92 mmHg, respiratory rate 16 breaths per minute, and oxygen saturation 99% while breathing room air.The patient was alert and oriented and in no acute distress.His sclerae were anicteric.His abdomen was soft with mild tenderness in the left lower quadrant.No rebound or voluntary guarding was noted.There was no costovertebral angle (CVA) tenderness to palpation.In addition, there was no tenderness at McBurney's point.His genital examination was normal.
An emergency physician (EP) performed a point-ofcare abdominal ultrasound, paying particular attention to the left lower quadrant of the abdomen.The sigmoid colon was identified in the left lower quadrant of the abdomen, with evidence of bowel wall thickening (Figure 1).In addition, a single diverticulum, visualized as an echo-poor protrusion from the colon wall with surrounding hyperechoic fat stranding, indicative of active inflammation, was noted at the point of maximal tenderness (Figure 2).The EP determined that the patient's presentation combined with the point-of-careultrasound images was consistent with a diagnosis of acute diverticulitis.The EP offered the patient the option of further testing with CT imaging versus empiric treatment with oral antibiotics.The patient opted to forego further radiologic testing and was subsequently discharged with a course of oral antibiotics and close primary care follow-up.

Figure 1.This fi gure demonstrates a measurement taken by the EP of the bowel wall that is approximately 1 cm.A measurement of >4–5 mm is indicative of bowel wall thickening.
Three weeks after his initial ED visit, the patient presented with recurrent abdominal pain to a different ED.He stated that his prior episode of abdominal pain had completely resolved with oral antibiotics.Twelve hours before his second ED visit, however, he developed recurrent left lower quadrant abdominal pain.Relevant bloodwork was as follows: WBC 10.3 K/μL, creatinine of 1.10 mg/dL, blood urea nitrogen 9 mg/dL, ALT 31 U/L, AST 20 U/L, alkaline phosphatase 44 U/L, and lipase 25 U/L.He subsequently underwent CT imaging of the abdomen, which demonstrated both prominent infl amed diverticuli and extensive fat stranding, consistent with acute uncomplicated sigmoid diverticulitis (Figure 3).He was admitted to the hospital and treated with intravenous antibiotics for 24 hours.He was discharged on a 7-day course of oral antibiotics and had no further episodes of diverticulitis.

Figure 2.This figure shows a single diverticulum (arrow) with surrounding hyperechoic (bright) fat stranding.
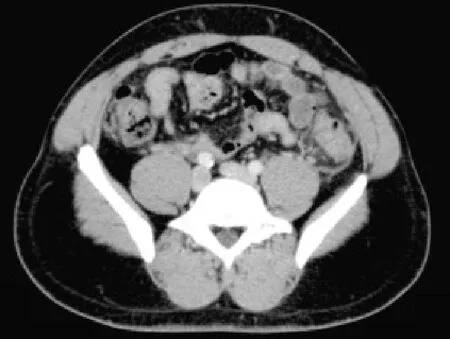
Figure 3.This figure shows the CT findings of acute uncomplicated diverticulitis (arrow) with surrounding fatstranding.
Case 2
A 49-year-old man with a history of diverticulitis presented with abdominal pain for one day to the ED.The pain began on the day before his ED presentation; it was described as sharp and localized to the left lower quadrant.He remarked that the pain was worse with movement and bending forward, and alleviated by remaining still.The pain was similar in quality to his one prior episode of uncomplicated diverticulitis.The patient denied fever, nausea, vomiting, diarrhea or constipation.
In the ED, the patient's vital signs were temperature 97.7 °F, heart rate 99 beats per minute, blood pressure 153/92 mmHg, respiratory rate 16 breaths per minute, and oxygen saturation 97% while breathing room air.The patient was awake, alert, and in no acute distress.His heart had a regular rate and rhythm and lungs were clear to auscultation.His abdominal examination was notable for normal bowel sounds and mild tenderness to palpation in the left lower quadrant, without rebound or guarding.He had no CVA or testicular tenderness on examination.
The EP performed a point-of-care ultrasound to evaluate the patient's left lower quadrant abdominal pain, and immediately identified a diverticulum with surrounding echogenic non-compressible fat consistent with an acute inflammatory process (Figure 4).The patient was diagnosed with sigmoid diverticulitis and was treated successfully with a ten-day course of oral antibiotics with a close primary care follow-up.

Figure 4.This figure demonstrates a single diverticulum (arrow) with adjacent hyperechoic (bright) fat stranding.
DISCUSSION
Acute diverticulitis is caused by inflammation of colonic diverticula, which can either occur in a true diverticulum (more frequently noted in right-sided diverticulitis) or in a false or pseudo-diverticulum (generally noted in left-sided diverticulitis).[7]Nearly20% of patients with diverticula will develop at least one episode of acute diverticulitis, thus rendering diverticulitis a major cause of hospitalization and medical expenditure.[3]As the population ages, the prevalence of diverticulitis will certainly rise, leading to a greater number of urgent care and ED visits for this disease.
Computed tomography has long been the diagnostic modality of choice to confirm acute diverticulitis in the United States.[8]Yet given the high cost associated with CT imaging, many countries utilize ultrasound as the first-line imaging study to make this diagnosis.[9]Other obvious drawbacks to CT imaging include radiation exposure and increased length of stay in the ED.As EPs become ever more adept at performing point-of care ultrasound examinations, this imaging modality has developed a reputation as an inexpensive, safe, and radiation-free alternative to CT in the ED.In a few studies ultrasound correctly diagnosed acute diverticulitis in greater than 90% of cases.[10]A recent meta-analysis also noted no significant difference between the sensitivity of ultrasound and CT in the evaluation of patients with suspected acute diverticulitis.[5]
The clinician performs an abdominal ultrasound to assess for diverticulitis by gently sweeping through loops of the bowel in the area of localized abdominal pain.A low-frequency curvilinear array transducer is used to visualize bowel as it provides adequate depth.The EP can ask the patient to point to the area of maximal tenderness, which often indicates the highestyield area for sonographic evaluation.The EP evaluates the symptomatic region with the transducer, looking for evidence of acute diverticulitis: (1) at least one diverticulum; (2) thickening of the bowel wall (typically 4–5 mm or more); and (3) echogenic non-compressible fat surrounding one or more diverticula, suggesting an acute infl ammatory process.[11,12]In addition, the clinician may identify a so-called "target sign" or "pseudokidney sign", which refers to the hypoechoic wall surrounding a hyperechoic center.[13]
Although multiple studies have confirmed the high sensitivity and specificity of ultrasound in the evaluation of patients with suspected diverticulitis, there are few reports on point-of-care ultrasound use for this indication.If utilized by providers with appropriate training, point-of-care ultrasound could possibly represent an ideal first-line imaging test for uncomplicated diverticulitis, with CT imaging reserved for ill-appearing patients with unstable vital signs, or for those whose point-of care ultrasound images demonstrate fi ndings concerning complicated diverticulitis, such as an abscess or intra-abdominal free fl uid.Further prospective studies are warranted.
Funding: None.
Ethical approval: Not needed.
Conflicts of interest: The authors declare that there are no confl icts of interest relevant to the content of the article.
Contributors: Abboud M analyzed the literature and drafted the manuscript.All authors contributed to the design and interpretation of the study and to further drafts.
REFERENCES
1 Kozak LJ, DeFrances CJ, Hall MJ.National hospital discharge survey: 2004 annual summary with detailed diagnosis and procedure data.Vital Health Stat 13.2006; 162: 1–209.
2 Sandler RS, Everhart JE, Donowitz M, Adams E, Cronin K, Goodman C, et al.The burden of selected digestive diseases in the United States.Gastroenterology 2002; 122: 1500–1511.
3 Stollman N, Raskin JB.Diverticular disease of the colon.Lancet 2004; 363: 631–639.
4 Weizman AV, Nguyen GC.Diverticular disease: epidemiology and management.Can J Gastroenterol 2011; 25: 385–389.
5 Lameris W, van Randen A, Bipat S, Bossuyt PM, Boermesster MA, Stoker J.Graded compression ultrasonography and computed tomography in acute colonic diverticulitis: metaanalysis of test accuracy.Eur Radiol 2008; 18: 2498–2511.
6 King WC, Shuaib W, Vijayasarathi A, Fajardo CG, Cabrera WE, Costa JL.Benefi ts of sonography in diagnosing suspected uncomplicated acute diverticulitis.J Ultrasound Med 2015; 34: 53–58.
7 Vijaraghavan SB.High-resolution sonographic spectrum of diverticulosis, diverticulitis, and their complications.J Ultrasound Med 2006; 25: 75–85.
8 Tack D, Bohy P, Perlot I, De Maertelaer V, Alkeilani O, Sourtzis S, et al.Suspected acute colon diverticulitis: imaging with lowdose unenhanced multi-detector row CT.Radiology 2005; 237: 189–196.
9 Nippak PM, Isaac WW, Ikeda-Douglas CJ, Marion AM, VandenBroek M.Is there a relation between emergency department and inpatient lengths of stay? Can J Rural Med 2014; 19: 12–20.
10 Gritzmann N.Acute colonic diverticulitis and diverticulosis.Med Radiology 2014; 37–43.
11 Schwerk WB, Schwarz S, Rothmund M.Sonography in acute colonic diverticulitis: a prospective study.Dis Colon Rectum 1992; 35: 1077–1084.
12 Mazzei MA, Cioffi Squitieri N, Guerrini S, Stabile Ianora AA, Cagini L, Macarini L, et al.Sigmoid diverticulitis: US fi ndings.Crit Ultrasound J 2013; 5 Suppl 1: S5.
13 Anderson DR.The pseudokidney sign.Radiology 1999; 21: 395–397.
Received May 16, 2015
Accepted after revision September 26, 2015
Corresponding Author:Sarah E.Frasure, Email: sarahfrasure@yahoo.com
DOI:10.5847/wjem.j.1920–8642.2016.01.015
 World journal of emergency medicine2016年1期
World journal of emergency medicine2016年1期
- World journal of emergency medicine的其它文章
- Information for Readers
- World Journal of Emergency Medicine
- The Chikungunya virus: An emerging US pathogen
- Instructions for Authors
- Generalized seizure, the only manifestation of a small ischemic atherothrombotic infarction
- Invasive group B streptococcal infection in a patient with post splenectomy for hypersplenism secondary to liver cirrhosis and portal hypertension
