Minimally invasive closed reduction and internal fixation with fully threaded headless cannulated compression screws for repair of distal radius fracture: study protocol for a randomized controlled trial
Zhi Li *
Department of Orthopedic Surgery, Central Hospital Affiliated to Shenyang Medical College, Shenyang, Liaoning Province,China
BACKGROUND
Distal radius fracture is defined as a fracture within 3 cm of the distal articular surface (Hanel et al., 2002). When radius fracture and ulnar styloid process fracture occur together,internal fixation is generally not pursued; however, adverse events may occur after reduction with external fixation, including unstable fracture fragments, malalignment, and loss of radial inclination and ulnar deviation (Wei et al., 2009),leading to wrist function impairment (Yu et al., 2005).
The commonly used treatment methods for distal radius fracture include internal fixation with steel plate, internal fixation with Kirschner wire, and external fixation. Open reduction and internal fixation (ORIF) has disadvantages.For example, the pronator teres is incised in palmar ORIF and in situ suturing of the muscle is not possible in most patients after implantation of the titanium plate. Even when suturing is possible, the strength of the pronator teres will decrease after surgery, and a second surgery is needed to remove the titanium plate. Dorsal ORIF is also disadvantageous because more tendons and thin soft tissue may be encountered during surgery. In addition, tendon sheath injury is inevitable, leading to myotenositis, tendon adhesion, and even tendon rupture. Thus, internal fixators should be taken out as early as possible (Bhattacharyya and Wadgaonkar,2008). Satisfactory wrist function outcomes have been achieved with external fixators, in particular with dynamic external fixators. However, although external fixation has good fixing effects, it provides poor lateral stability, resulting in injury to the super ficial branch of the radial nerve,screw channel infection, screw channel fracture, screw loosening, and even Sudeck's atrophy (Li et al., 2008).Internal fixation with Kirschner wire generates minimal surgical trauma (Li et al., 2007), but this technique does not provide sufficient strength for fixation and is therefore rarely used at present. There is an urgent need to develop a more stable fixation method for distal radius fracture. Minimally invasive surgery avoids the tissue damage and impairment of physiological function caused by open surgery because of its precise location techniques. Brachial plexus anesthesia allows surgeons to avoid large incisions and excessive bleeding (Hu et al., 2015; Schuind et al., 2015; Zhang et al.,2015). There are no palmar or dorsal incisions in minimally invasive surgery for distal radius fractures, so the structures surrounding the wrist joint are not iatrogenically damaged,which theoretically improves wrist function recovery (Fei et al., 2014; Yamazaki et al., 2015).
During C-arm fluoroscopy-assisted minimally invasive closed reduction, either no surgical incision or an incision only 0.5 cm in length is made at the wrist joint; the fracture fragments are reduced with fully threaded headless cannulated compression screws. Repair stability is assessed with the C-arm fluoroscopic X-ray system. This method is theoretically feasible for distal radius fractures. The fracture fragments are fixed with fully threaded, cannulated,variable-pitch, headless compression screws, which can increase fragment stability (Zhang et al., 2012). Therefore,we hypothesize that C-arm fluoroscopy-assisted minimally invasive closed reduction will fix distal radius fractures and allow patients to perform wrist function exercises as early as possible.
Our previous studies have con firmed that minimally invasive closed reduction and internal fixation with fully threaded headless cannulated compression screws has precise therapeutic effects for distal radius fractures (Li et al., 2007; Li et al., 2012). This method can improve wrist function, and has therapeutic effects similar to those of conventional open reduction and internal fixation with titanium plates (Wang and Li, 2003). The results of these previous studies are shown in Table 1. However, it is not clear whether minimally invasive closed reduction and internal fixation with fully threaded headless cannulated compression screws has advantages over conventional open reduction and internal fixation with titanium plates for distal radius fracture repair.
In this study, we hypothesized that minimally invasive closed reduction and internal fixation with fully threaded headless cannulated compression screws provides better stability than conventional methods, and can effectively promote the early recovery of wrist function. Under conditions of no cutting of fracture fragments, no blood supply compromise in the fracture fragments, and no destruction of the local microenvironment, and with C-arm fluoroscopy assistance, we will perform minimally invasive closed reduction, pressurizing the fracture fragments with fully threaded headless cannulated compression screws, and will investigate whether this method of distal radius fracture repair provides satisfactory stability and allows early wrist function recovery.
METHODS/DESIGN
This is a prospective randomized controlled trial. The entire trial will be designed and managed by ZL. Sixty patients with distal radius fracture will be randomly divided into two treatment groups. The experimental group (n = 30) will undergo C-arm fluoroscopy-assisted minimally invasive closed reduction and internal fixation with fully threaded headless cannulated compression screws. The control group(n = 30) will undergo open reduction, including palmar and dorsal incisions, and internal fixation with a titanium plate.X-ray and CT examinations of the fracture fragments will be performed 24 weeks after surgery. The trial protocol is shown in Figure 1.
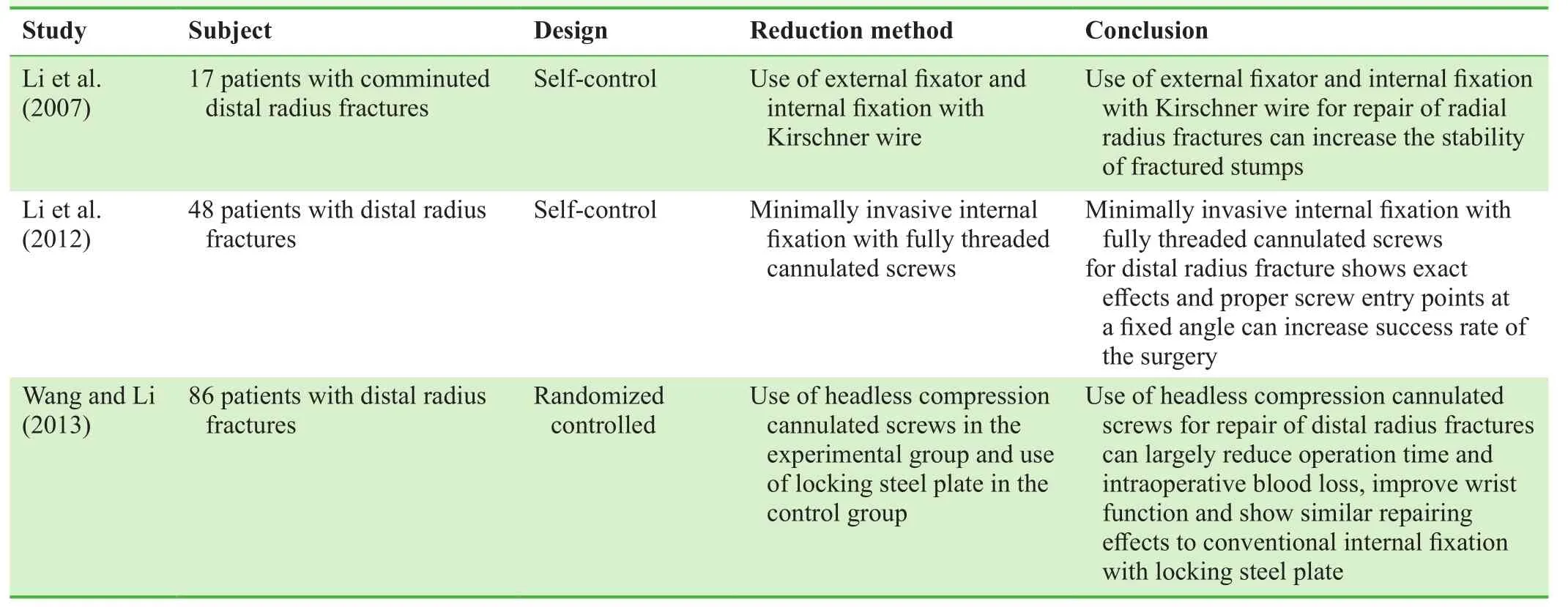
Table 1: Previous studies of distal radius fracture repair methods reported by the team of ZL

Figure 1: Flow chart of the trial protocol.
Study participants
Sixty patients with distal radius fractures will be recruited from the Bone Surgery Clinic, Central Hospital Affiliated to Shenyang Medical College, China.
Inclusion criteria
Patients with distal radius factures clinically diagnosed according to the diagnostic criteria formulated at the Fourth Session of the Second Meeting of the Chinese Medicine Institute in Orthopedics, Guangzhou, China (Tan, 2007)must meet all of the following criteria for inclusion:
· Age 55 years or older, either sex
· A history of known trauma
· Presence of wrist joint pain and limitation of motion after trauma
· Fracture occurring 2.0–3.0 cm proximal to the articular surface, con firmed with imaging findings
· Unstable distal radius fracture
· Dorsal displacement of fracture fragment
· Fracture involving the wrist joint, but no more than two fracture fragments involving the wrist joint
Exclusion criteria
Patients with clinically diagnosed distal radius fractures presenting with any of the following characteristics will be excluded.
· Acute fracture of several other regions, including the ulnar styloid process
· Open fracture
· Mental disorder
· Occurrence of fracture more than 21 days before presentation
· Severe heart, lung, liver, or kidney function disorder
· Severe local infection after fracture
· Refusal to sign informed consent form
· Poor compliance, or upon the request of the sponsor for safety reasons
· If participation in the trial would be a potential hazard to patient’s heath
Sample size
Following the intention-to-treat analysis principle, 60 patients, n = 30 patients per group, will be included in this trial.
Randomization and interventions
One day prior to treatment, a temporarily arranged physician will generate random sequences with SPSS (SPSS,Chicago, IL, USA) to allocate the 60 patients into either the experimental or the control group with a 1:1 allocation ratio.Medical advice will be electronically recorded. Patients in the experimental group will undergo C-arm fluoroscopyassisted minimally invasive closed reduction and internal fixation with fully threaded headless cannulated compression screws. Patients in the control group will undergo open reduction (palmar and dorsal incisions) and internal fixation with a titanium plate (Ningbo Cibei Medical Treatment Appliance Co., Ltd., Ningbo, China). Internal fixation will be maintained for 24 weeks in both groups.
C-arm fluoroscopy-assisted minimally invasive surgery
In the experimental group, fractures will be reduced and internally fixed with fully threaded headless cannulated compression screws of appropriate lengths (Acutrak plus;Acumed Inc., Beaverton, OR, USA) under C-arm fluoroscopic guidance to restore the radial inclination and ulnar deviation of the distal radius.
Rehabilitation training
Both groups of patients will perform the same functional exercises of the wrist joint and metacarpophalangeal joint after internal fixation, under physician guidance. From day 3 after surgery, non-loaded wrist joint exercises(palmer flexion, dorsal extension, radial-ulnar deviation,and slight rotation) will be performed, twice per day for 15 minutes initially and gradually increasing to 30 minutes once daily.
Outcome measures
The timing of outcome measures is shown in Table 2.
Primary outcomes
Imaging findings prior to and at 3, 6, 12, and 24 weeks after treatment:
X-ray findings: Measurement of radial inclination and ulnar deviation of distal radius, measurement of radial height and length, and observation of fracture line on anteroposterior and lateral X-ray images.
CT findings: CT images can help clarify the displacement direction and angle of fracture fragments and the degree of articular surface collapse, and can identify hidden wrist fracture.
Imaging findings of fracture fragments at 24 weeks after treatment will be mainly evaluated.
Secondary outcomes
· Patient-rated wrist evaluation (PRWE) score (John et al., 2008) at 3, 6, 12, and 24 weeks after treatment:The PRWE is a 0–100-point scale that evaluates pain, range of motion, grip strength, daily activities,and specific activity of the wrist joint. Higher scores indicate more severe joint pain and dysfunction.

Table 2: Timing of trial outcome measures
· Healing of fracture at 3, 6, 12, and 24 weeks after treatment: earlier radiographic disappearance of the fracture line indicates faster healing
· Visual Analogue Scale (VAS) score at 3, 6, 12, and 24 weeks after treatment: used to evaluate wrist joint pain after treatment.
Safety assessment
Adverse events should be accurately recorded, including time of onset, severity, duration, and measures taken. The known possible adverse events include bone nonunion,displaced fracture, wrist joint pain, Sudeck's syndrome,primary or secondary tendon injury, shoulder-hand syndrome, traumatic arthritis of the wrist joint, implant failure,malunion, infection, septicemia, and thrombosis.
Any of the following will be considered a severe adverse event: death, prolonged hospital stay, mutilation, fatal reaction, or teratogenicity. Any adverse event occurring during the trial will be reported to the researchers in charge and to the ethics committee within 24 hours.
Follow-up
All patients will be followed up at 3, 6, 12, and 24 weeks after surgery and follow-up medical record forms will be completed. The time of the last rehabilitation training session will be recorded. Electronic follow-up medical records will be preserved.
When patients drop out of the trial, the reasons for withdrawal will be recorded in detail. Comprehensive and supportive patient communication will be undertaken; patients lost to follow-up because of any reason will be gotten in touch as soon as possible and be followed up within 3, 6,12 and 24 weeks.
Data regarding patients withdrawn from the trial will be included in the final analysis, according to the intention-totreat analysis principle.
Data management
Data from the trial will be kept in a secure, locked storage area with limited access for later review by a biostatistician,a researcher in charge.
Statistical analysis
All data will be statistically processed with SPSS 11.0 software (SPSS, Chicago, IL, USA). Normally distributed measurement data will be expressed as mean and SD. Nonnormally distributed measurement data will be expressed as lower quartile (q1), median, and upper quartile (q3). The numeration data will be expressed as constituent ratios. The Mann–Whitney U non-parametric test will be used to compare age and course of disease between the experimental and control groups. The chi-square test will be used to compare sex differences between the two groups. The Mann–Whitney U non-parametric test will also be used to compare imaging parameters (for example, angle, height, and length), PRWE scores, healing time of fracture, and VAS scores. The chisquare test will also be used to compare the effective rate between the two groups. An alpha level of 0.05 (two-sided)will be considered statistically significant.
DISCUSSION
This trial will follow a strict randomized controlled principle. Imaging findings, the primary outcome of this trial,will help precisely assess the repair effects. The positions for implantation of fully threaded headless cannulated compression screws are the super ficial branch of the radial nerve and the extensor pollicis longus muscle, which should be well protected during implantation of the fully threaded headless cannulated compression screws from the ulnar styloid process with the assistance of C-arm fluoroscopy. To ensure the effects of internal fixation, a guide pin should be implanted into the lateral radial cortex, and fully threaded headless cannulated compression screws should reach or extend slightly into the lateral radial cortex.
It is difficult to use conventional X-rays to diagnose distal radius fracture in the navicular fossa and lunar bone fossa.For this reason, CT imaging will be performed in this trial to increase diagnostic accuracy. CT imaging is important in diagnosing three-column injury of the distal radius and ulna, including articular surface injury. CT is especially helpful in diagnosing injury of the medial column, which is easily missed on X-ray examination. We hope that findings from this trial will con firm that minimally invasive closed reduction and internal fixation with fully threaded headless cannulated compression screws achieves better stability for distal radius fractures than conventional open reduction (palmar and dorsal incisions) and internal fixation with a titanium plate, further con firming that distal radius fractures are an indication for minimally invasive surgery.
Trial status
Recruiting at the time of submission.
Con flicts of interest
None declared.
Author contributions
ZL designed this trial protocol, collected and processed data and agreed the final version of this paper for publication.
Plagiarism check
This paper was screened twice using Cross Check to verify originality before publication.
Peer review
This paper was double-blinded and stringently reivewed by international expert reviewers.
Bhattacharyya T, Wadgaonkar AD (2008) Inadvertent retention of angled drill guides after volar locking plate fixation of distal radial fractures: a report of three cases. J Bone Joint Surg Am 90:401-403.
Fei JL, Liang B, Jiang CZ, Wang LM (2014) Minimally invasive treatment for distal radial fracture and dislocation of type IV based on Fernandez classification. Zhongguo Gu Shang 27:341-345.
General Assembly of the World Medical Association (2014) World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. J Am Coll Dent 81:14-18.
Hanel DP, Jones MD, Trumble TE (2002) Treatment of complex fractures, wrist fractures. Orthop Clin North Am 33:35-37.
Hu XF, Wei SS, Wang SS (2015) Treatment of osteochondritis lesion in the knee with reduction and fixation under arthroscopy.Zhongguo Gu Shang 28:963-966.
John M, Angst F, Awiszus F, Pap G, Macdermid JC, Simmen BR(2008) The patient-rated wrist evaluation (PRWE): cross-cultural adaptation into German and evaluation of its psychometric properties. Clin Exp Rheumatol 26:1047-1058.
Knop C, Oeser M, Bastian L, Lange U, Zdichavsky M, Blauth M(2001) Development and validation of the Visual Analogue Scale(VAS) Spine Score. Unfallchirurg 104:488-497.
Li J, Jin D, Ding XF, Hu YL, Pei GX (2008) External fixation versus plate osteosynthesis for unstable distal radius fractures: a meta analysis. Zhonghua Chuangshang Guke Zazhi 10:405-409.
Li Z, Wang L, Ma J (2007) Treatment of 17 patients with comminuted intra-articular fracture of distal end of the radius by external fixation and percutaneous pins. Shenyang Yixueyuan Xuebao 9:13-17.
Li Z, Ma J, Zhang Y, Yang LF, Zhao W (2012) Effect of non head compression screw for internal fixation of distal radius fracture.Shandong Yiyao 52:65-66.
Schuind S, De Witte O, Sadeghi N, Lefranc F (2015) Supraorbital approach to treat a fronto-orbital fracture with pneumocephaly, a minimal invasive technique. Rev Med Brux 36:430-432.
Tan YC (2007) The Fourth Session of the Second Meeting of Chinese Medicine Institute in Orthopedics. Guangzhou, China.
Wang N, Li Z (2013) Effectiveness of acutrak compression screws and locking compression plates for the distal fracture of radius.Yixue yu Zhexue 34:23-26.
Wei DH, Raizman NM, Bottino CJ, Jobin CM, Strauch RJ, Rosenwasser MP (2009) Unstable distal radial fractures treated with external fixation, a radial column plate, or a volar plate: a prospective randomized trial. J Bone Joint Surg Am 91:1568-1577.
Yamazaki H, Uchiyama S, Komatsu M, Hashimoto S, Kobayashi Y, Sakurai T, Kato H (2015) Arthroscopic assistance does not improve the functional or radiographic outcome of unstable intraarticular distal radial fractures treated with a volar locking plate: a randomised controlled trial. Bone Joint J 97-B:957-962.
Yu JH, Feng JS, Li ZY, Huang AQ (2005) The impact of tilt changes due to distal radius fractures on wrist joint: a biomechanical study.Zhongguo Jiaoxing Waike Zazhi 13:750-752.
Zhang J, Wu K, Zhang W, Wu W, Hou S (2012) Percutaneous fixation of pelvic fracture by acutrak full thread headless hollow compression screw. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 26:91-96.
Zhang QX, Gao FQ, Sun W, Wang YT, Yang YR, Li Z (2015) Minimally invasive percutaneous plate osteosynthesis versus open reduction and internal fixation for distal tibial fractures in adults: a meta-analysis. Zhongguo Gu Shang 28:757-762.
 Clinical Trials in Orthopedic Disorder2016年2期
Clinical Trials in Orthopedic Disorder2016年2期
- Clinical Trials in Orthopedic Disorder的其它文章
- Polymerase chain reaction for diagnosis of isolated tuberculosis of the wrist joint
- Lateral dislocation of the elbow: a report of two cases and literature review
- Isometric muscle strength as a predictor of one repetition maximum in healthy adult females: a crossover trial
- Consistency of microbiological and pathological tests between infected bone and surrounding deep soft tissues in diabetic foot osteomyelitis: study protocol for a singlecenter, self-controlled, open-label trial
- Minimally invasive treatment of proximal humerus fractures with locking compression plate improves shoulder function in older patients: study protocol for a prospective randomized controlled trial
- Treatment of intertrochanteric femoral fracture with proximal femoral medial sustainable intramedullary nails: study protocol for a randomized controlled trial
