Relationship between dermatochalasis and more prominent with aging: a prospective study in a tertiary referral center
Feride Aylin Kantarci, Muhammed Nabi Kantarci, Mehmet Gurkan Tatar,Emine Esra Karaca
1Department of Ophthalmology, Fatih University Medicine Faculty, Maltepe 34844, Istanbul, Turkey
2Department of Forensic Medicine, Ministry of Justice, Forensic Science Institue, Bahçelievler 34196, Istanbul, Turkey
3Department of Ophthalmology, Sorgun State Hospital, Sorgun 66700, Yozgat, Turkey
Correspondence to:Feride Aylin Kantarci. Department of Ophthalmology, Fatih University Medicine Faculty, Yali District, Coastal Way Street No:16, Maltepe 34844, Istanbul, Turkey. ferideaylin@gmail.com
Received: 2015-01-06 Accepted: 2015-07-29
眼睑皮肤松垂程度与年龄的关系——三级转诊中心的前瞻性研究
Relationship between dermatochalasis and more prominent with aging: a prospective study in a tertiary referral center
Feride Aylin Kantarci1, Muhammed Nabi Kantarci2, Mehmet Gurkan Tatar1,Emine Esra Karaca3
1Department of Ophthalmology, Fatih University Medicine Faculty, Maltepe 34844, Istanbul, Turkey
2Department of Forensic Medicine, Ministry of Justice, Forensic Science Institue, Bahçelievler 34196, Istanbul, Turkey
3Department of Ophthalmology, Sorgun State Hospital, Sorgun 66700, Yozgat, Turkey
Correspondence to:Feride Aylin Kantarci. Department of Ophthalmology, Fatih University Medicine Faculty, Yali District, Coastal Way Street No:16, Maltepe 34844, Istanbul, Turkey. ferideaylin@gmail.com
Received: 2015-01-06Accepted: 2015-07-29
眼睑皮肤松垂程度与年龄的关系——三级转诊中心的前瞻性研究
引用:Kantarci FA, Kantarci MN, Tatar MG, Karaca EE. 皮肤松垂程度与年龄的关系-三级转诊中心的前瞻性研究.国际眼科杂志2016;16(1):19-23
Abstract
•AIM: To investigate the localization and severity of dermatochalasis and accompanying pseudoptosis with age.
•METHODS:One hundred and thirteen subjects with dermatochalasis were included in the study. Age, gender and body mass index (BMI) of the subjects were recorded. Palpebral fissure height (PFH) and marginal reflex distance (MRD) were measured in the primary position. The severity of dermatochalasis was assesed as Stage 1: behind eyelid margin (minimum 1 mm); Stage 2: inline with eyelid margin; Stage 3: before eyelid margin.
•RESULTS: Mean age of the subjects were 52.7±8.6 (range 32 to 74)y. Thirty-six cases (31.9%) were male and 77 (68.1%) were female. The mean BMI was 30.3±4.7 (range 21.5 to 36.6) kg/m2, mean PFH was 10.7±1.6 (range 7 to 15) mm, mean MRD was 3.8±1.2 (range 1 to 5) mm. In 30 (26.5%) of the subjects dermatochalasis was localized behind eyelid margin, in 38 (33.6%) it was inline with eyelid margin and in 45 (39.8%) it was before eyelid margin. There was pseudoptosis due to dermatochalasis in 50 (44.2%) of the subjects. Age was significantly different in terms of dermatochalasis severity. Mean ages of subjects with dermatochalasis localization behind or inline with eyelid margin (50.3±6.6, 50.5±9.5y), were significantly lower than subjects with dermatochalasis localization before eyelid corner (56.0±8.2y). Mean age of subjects with pseudoptosis were significantly higher (56.3±8.3y), than subjects without it (49.8±7.8y). There was no BMI difference between the subjects in terms of dermatochalasis severity and presence of pseudoptosis.
•CONCLUSION:Dermatochalasis localization, severity and frequency of pseudoptosis increase with age.
KEYWORDS:•aging; blepharoptosis; dermatochalasis
Citation:Kantarci FA, Kantarci MN,Tatar MG, Karaca EE. Relationship between dermatochalasis and more prominent with aging: a prospective study in a tertiary referral center.GuojiYankeZazhi(IntEyeSci) 2016;16(1):19-23
INTRODUCTION
Various changes in eyelids, eyebrows and eyelashes, such as dermatochalasis, senile entropion and ectropion, and ptosis, may be observed with increasing age[1]. Eyelashes and eyelids get white with increasing age and this can be used in age determination after 40y of age[2]. Dermatochalasis is a common ocular manifestation of aging[1,3]. Dermatochalasis refers to redundant eyelid skin and subcutaneous tissue. Dermatochalasis is caused by laxity from involutional changes with aging. The orbital fat frequently prolapses through an attenuated septum[3-4]. Excess upper eyelid skin may overhang the eyelashes and obstruct visualization of the eyelid margin, giving the impression of a low-lying eyelid[5]. Blepharoptosis, more commonly known as ptosis, is a downward displacement of the upper eyelid margin. The causes of ptosis are myogenic, involutional, neurogenic, mechanical, traumatic, or congenital[6]. Severe dermatochalasis is also associated with upper-eyelid ptozis (droopy lid) or pseudoptosis (mechanical effect from the dermatochalasis)[4,7].
Gravity, loss of elasticity in eyelid skin, and weakining of connective tissue contribute to the formation on lax and redundant eyelid tissue[4,8-10]. Age and ultraviolet dependent changes in elastin and collagen in eyelid tissue may be observed. Collagenase enzyme released from impaired epidermis contributes to collagen degeneration. Dermatochalasis may also be observed among young people due to ultraviolet damage. Orbital septum which become thinner and weaker with time makes protrusion of subcutanous fat pads easier. Subcutanous fat pads may also be seen at medial of upper eyelid and central and lateral of lower eyelid[11].
Hereditary passing, smoking and nutrition may be effective on dermatochalasis formation[11-12]. Hereditary angioedema, lymphedema, renal diseases, cutis laxa, and collagen vascular diseases (Ehlers-Danlos syndrome) must be considered in subjects with recurring dermatochalasis[11].
Dermatochalasis may lead to functional and cosmetic impairments in the patients[10,13-15]. It may lead to narrowing of visual field due to blepharoptosis[13,16]. Besides, entropion, corneal irritation, difficulty in reading and narrowed peripheral vision may also develop. Laxed eyelid skin may lead to eye tiredness and may prevent eye make-up in women[6,11,14]. Dermatochalasis may also cause serious psychological problems in the subjects[13,15]. For all these reasons, dermatochalasis must be treated[3].
The type and requirement of surgery differ with severity of dermatochalasis. Therefore, in our study, we investigated clinically the localization and severity of dermatochalasis. Association of dermatochalasis localization and severity with age and accompanying signs were evaluated. Effects of gender and body mass index (BMI) on dermatochalasis were also investigated.
SUBJECTS AND METHODS
Our study was conducted in 113 individuals with dermatochalasis who were evaluated at Fatih University Ophtalmology Clinic. Our study was approved by the relevant institutional review boards and performed in accordance with the ethical guidelines of the Declaration of Helsinki. All individuals signed written informed consent. Age, gender, weight and height of the individuals were recorded. BMI was computed as ‘weight/height2’ after weight was measured as kilogram and height was measured as metres. BMI was categorised into four groups: normal range (18.5-24.9), overweight range (25-30), obese (>30), and under the weight range (<18.5). Subjects with history of recurring eyelid edema and systemic diseases, which may lead to blepharochalasis were not included in the study.
Individuals were also evaluated for eyebrow ptosis since it can be confused with dermatochalasis. If the eyebrow is under superior orbital rim, the low eyebrow will push the eyelid down. Clinician must lift eyebrow above superior orbital rim with two fingers and must evaluate redundant eyelid tissue which is supposed to be due to dermatochalasis. If dermatochalasis is due to low eyebrows, correction of this condition usually leads to cosmetic and functional improvement. Levator muscle function was evaluated to differentiate from real ptosis[9, 11]. Complete ophtalmological examination of the subjects, including visual acuity, intraocular pressure, fundus and anterior segment examinations. Palpebral fissure height (PFH) and marginal reflex distance (MRD) were measured in the primary position. The distance between the corneal light reflex and the upper eyelid margin when the patient gazes at light source is named as MRD1, and the distance to lower eyelid is named as MRD2[9,17]. PFH ranges changes between 7-10 mm in men and 8-12 mm in women. In ptosis evaluation, mild refers to drooping to 2 mm, moderate refers to drooping to 3 mm, and severe refers to drooping of 4mm or more. The distance between upper eyelid fold and eyelid margin is 10 mm in women and 8 mm in men. MRD1 measurement is 4-4.5 mm on average[18].
In our study, the severity of dermatochalasis was evaulated as Stage 1: behind eyelid margin (minimum 1 mm) (Figure 1A), Stage 2: inline with eyelid margin (Figure 1B), Stage 3: before eyelid margin (Figure 1C). Pseudoptosis due to dermatochalasis was evaluated in the cases (Figure 1D).
Statistical AnalysisNCSS (Number Cruncher Statistical System) 2007&PASS (Power Analysis and Sample Size) 2008 Statistical Software (Utah, USA) was used for statistical analysis. Statistical analysis included descriptive statistical methods (mean, standard deviation, median, frequency, rate, minimum, maximum), along with Student’st-test, which was used to compare two groups in quantitative data which were normally distributed. Oneway ANOVA test was used to compare three or more groups with normal distribution and Tukey HSD test was used to detect the group which lead to statistical difference. Pearson Chi-square test and Yates Continuity Correction test were used to compare qualitative data. Significance was evaluated atP<0.01 andP<0.05 levels.

Figure 1Severity of dermatochalasisA: Stage 1: behind the eyelid margin (minimum 1 mm); B: Stage 2: in alignment with eyelid margin; C: Stage 3: before the eyelid margin; D:Pseudoptosis due to dermatochalasis.
Table 1Evaluation of descriptive features regarding dermatochalasis severity

±s;n(%)
aOneway ANOVA test;bPearson Chi-square test.
RESULTS
Mean age of the individuals were 52.7±8.6 (range 32 to 74)y. Thirty-six cases (31.9%) were male and 77 cases (68.1%) were female.
BMI measurement changed between 21.5 and 36.6 kg/m2, with a mean of 30.3±4.7 kg/m2. The mean eyelid aperture was 10.7±1.6 (range 7 to 15) mm, and mean MRD1 was 3.8±1.2 (range 1 to 5) mm.
In 30 of the cases (26.5%) dermatochalasis was localized behind eyelid margin, in 38 of the cases (33.6%) was inline with eyelid margin and in 45 of the cases (39.8%) was front eyelid margin.
There was a highly significant difference between mean ages in terms of dermatochalasis severity (P=0.003). Binary comparisons indicated that mean ages of individuals mild dermatochalasis (behind eyelid margin or inline with eyelid margin) were significantly lower than individuals with severe (dermatochalasis skin fold before the eyelid margin) (P=0.011;P=0.008) (Table 1). There was no significant age difference between individuals with dermatochalasis behind eyelid margin or inline with eyelid margin (P>0.05) (Table 1,
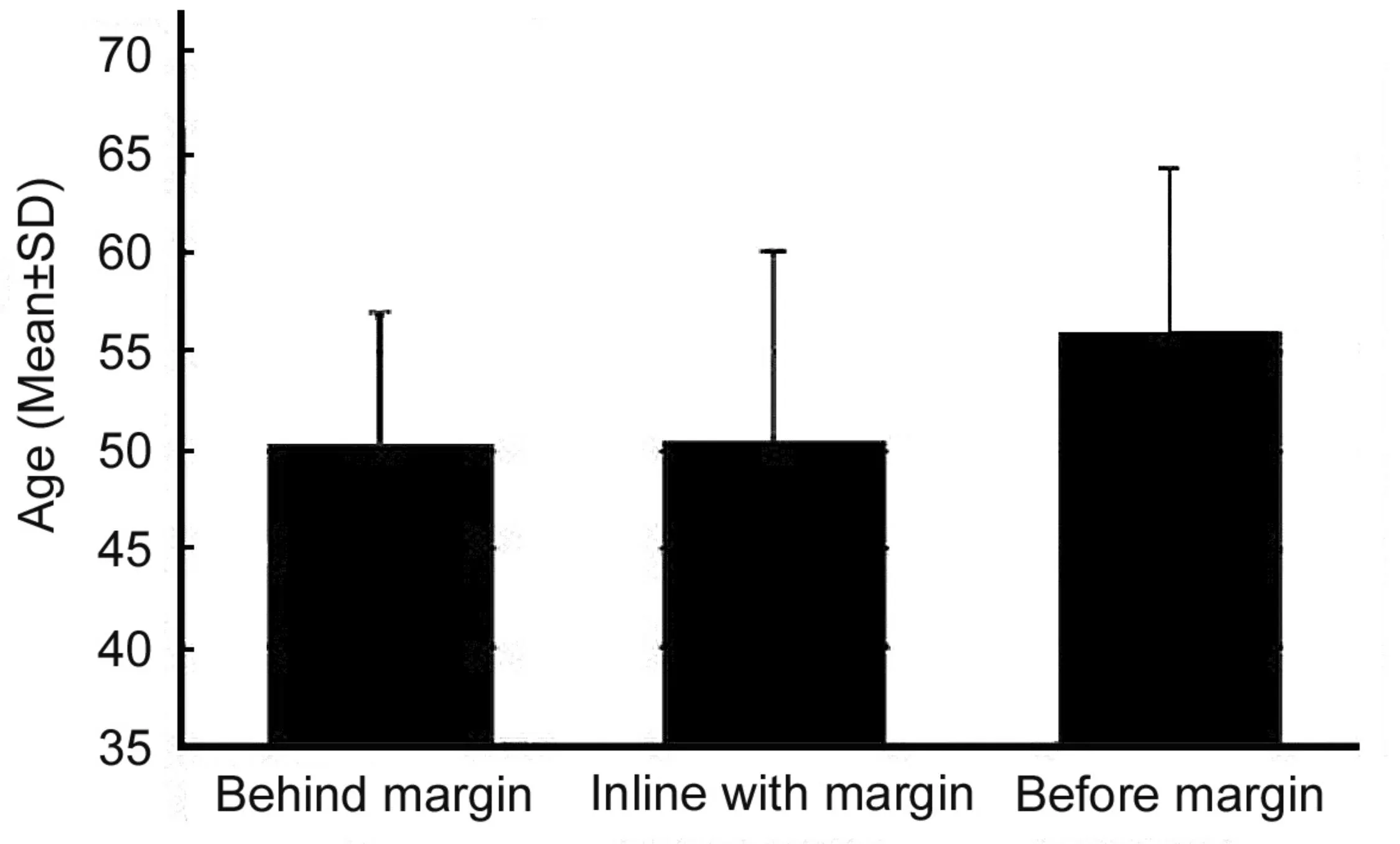
Figure 2The relationship between age distribution and severity of dermatochalasis.
Figure 2). There were no significant differences of BMI measurements of the individuals regarding dermatochalasis severity (P>0.05).
There was a highly significant difference of eyelid aperture measurements in terms of dermatochalasis severity (P=0.001) (Table 1). Binary comparisons indicated that mean eyelid aperture of individuals with mild dermatochalasis (behind eyelid margin or inline with eyelid margin) were significantly higher than individuals with severe (dermatochalasis skin fold before the eyelid margin) (P=0.001;P=0.019). There was no significant eyelid aperture difference between individuals with dermatochalasis behind eyelid margin or inline with eyelid margin (P>0.05) (Table 1).
There was a significant difference of gender in terms of dermatochalasis severity (P=0.035) (Table 1, Figure 3). The ratio of females were higher among individuals with dermatochalasis severity behind eyelid margin when compared with individuals with inline with eyelid margin. There were no significant gender differences between other groups.

Figure 3The relationship between gender and severity of dermatochalasis.
There was a highly significant difference of pseudoptosis frequency in terms of dermatochalasis severity (P=0.001) (Table 1). Pseudoptosis was significantly less common among individuals with dermatochalasis localized behind eyelid margin when compared with subjects with dermatochalasis localization inline with eyelid margin or before eyelid margin. Pseudoptosis was also significantly less frequent in individuals with dermatochalasis in line with the eyelid margin when compared with subjects with dermatochalasis localized before eyelid margin. It can be suggested that pseudoptosis frequency increased with increasing the lower edge of the dermatochalasis fold (Table 1).
There was a highly significant age difference among individuals in terms of presence of pseudoptosis (P=0.001). Mean age of subjects with pseudoptosis was significantly higher than individuals without it. There was no significant BMI measurement and gender distribution differences regarding presence of pseudoptosis (P>0.05) (Table 2).
DISCUSSION
Eyes are the most important parts of the face aesthetically and they may be exposed to changes with increasing age[1]. Mild degrees of dermatochalasis may be managed with laser skin resurfacing[19]. In most cases, surgical excision of skin and muscle will be required to achieve an acceptable cosmetic and functional result[9,15,20]. Dermatochalasis may present alone or with fatty prolapse, or ptosis. Accordingly, the surgical solutions may vary. Dermatochalasis alone is corrected by carring out a skin-excision blepharoplasty. Dermatochalasis with fatty prolapse is managed by performing a blepharoplasty with trimming of only sufficient fat. Pseudoptosis with dermatochalasis is corrected using blepharoplasty, plus levator aponeurotic repair[20-22]. It has been shown that dermatochalasis has negative effects on individuals and that these effects decrease with surgical correction[23].
Dermatochalasis is a redundant skin fold which increase with time, and there is no definitive classification of it. Therefore, we evaluated individuals with dermatochalasis in our study in terms of the position of skin fold relative to eyelid margin. We also compared presence of pseudoptosis regarding dermatochalasis severity. We evaluated the association with age, gender and BMI. In our study, we investigated individuals with dermatochalasis who did not have systemic problems.
Table 2Evaluation of demographical features regarding pseudoptosis

±s;n(%)
aStudent’st-test;bYates’ Continuity correction test.
In our study, mean age of the individuals was 52.7±8.6 (range 32 to 74)y and 77 individuals (68.1%) were female. It has been known that dermatochalasis is caused by age dependent changes. We did not find any information in the literature indicating whether dermatochalasis is more common in males or females. A previous study reported that 64.1% of individuals who have blepharoplasty surgery for dermatochalasis were females[24]. A significant gender difference was found in terms of dermatochalasis severity. Female ratio was significantly higher among individuals with dermatochalasis localized behind eyelid margin when compared with individuals with dermatochalasis localized inline with eyelid margin.
Progressive effects of aging on dermatochalasis stage has not been defined in the literature. In our study, we found a highly significant difference of age regarding dermatochalasis. Mean ages of individuals with dermatochalasis localized behind eyelid margin or inline with eyelid margin (50.3±6.6, 50.5±9.5y) were significantly lower than mean age of individuals with dermatochalasis localized before eyelid margin (56.0±8.2y). This difference may indicate that skin fold increase and become more prominent with aging.
Eyelid opening measurements of individuals with dermatochalasis localized behind eyelid margin or inline with eyelid margin were significantly higher than subjects with dermatochalasis localized before eyelid margin. Rate of pseudoptosis was significantly higher in individuals with dermatochalasis localized before eyelid margin when compared with individuals with dermatochalasis localized inline with or before eyelid margin.
Blepharoplasty surgery is applied to subjects with pseudoptosis due to dermatochalasis for functional and cosmetic reasons.Among these individuals those with a superior visual field defect, a MRD1≤2 mm and those with difficulty when reading looking down have been reported to be more content with the treatment[3]. Kimetal[25]reported that increased contrast sensitivity and improved functional visual acuity after upper eyelid blepharoplasty were caused by changes in corneal high-order aberration and the degree of lash ptosis after surgery. In addition, there were no changes in corneal topography or astigmatism.Watanabeetal[26]showed that long-term tear volume was not changed after blepharoplasty for dermatochalasis. On the contrary, long-term tear volume was decreased after blepharoptosis surgery, and even more so in cases with an initial high tear volume. After the blepharoplasty, significant variations were shown from those before the surgery, indicating that the correction of redundant tissues in the brow accentuates the tendency of the eyebrow to move down[27].
There was pseudoptosis in 44.1% of the individuals. In our study, we found a highly significant difference of mean age between individuals with and without pseudoptosis. It can be argued that, with increasing age skin fold increases and rates of pseudoptosis become higher.
It has been reported that dermatochalasis may be hereditary or due to smoking, nutrition and systemic diseases, along with aging[11].
In our study, we also evaluated the association between BMI and dermatochalasis localization among individuals without systemic diseases. Mean BMI measurement of the subjects were 30.3±4.7 (range 21.5 to 36.6) kg/m2. BMI was not associated with dermatochalasis severity and presence of pseudoptosis.
Limitations of our study included small sample size, no follow-up, not evaluating visual field defects and psychological complaints of the individuals due to dermatochalasis. The study can be repeated in the future in a more elaborate design.
In conclusion, degenerative changes in elastin and collagen tissues in eyelid structure have been shown to be associated with development of dermatochalasis[11]. In our study, we found that dermatochalasis localization and severity increase with increased age.
REFERENCES
1 Tyers AG. Aging and the ocular adnexa: a review.JRSocMed1982;75(11):900-902
2 Kantarci FA,Kantarci MN, Bilgi S. Age estimation using level of eyebrow and eyelash whitening.MedSciMonit2014;20:97-102
3 Friedman NJ, Kaiser PK.EssentialOfOphthalmology. USA: Elsevier Inc. 2007:125-149
4 Pottier F, El-Shazly NZ, El-Shazly AE. Aging of orbicularis oculi: anatomophysiologic consideration in upper blepharoplasty.ArchFacialPlastSurg2008;10(5):346-349
5 Cohen AJ, Weinberg DA.EvaluationandManagementofBlepharoptosis. USA: Springer; 2011:61-67
6 Cahill KV, Bradley EA, Meyer DR, Custer PL, Holck DE, Marcet MM, Mawn LA. Functional indications for upper eyelid ptosis and blepharoplasty surgery: a report by the American Academy of Ophthalmology.Ophthalmology2011;118(12):2510-2517
7 Martin JJ. Ptosis repair in aesthetic blepharoplasty.ClinPlastSurg2013;40(1): 201-212
8 Cho I. Aging blepharoplasty.ArchPlastSurg2013;40(5):486-491
9 Weissman JD, Most SP. Upper lid blepharoplasty.FacialPlastSurg2013;29(1):16-21
10 Lee H, Park M, Lee J, Lee ES, Baek S. Histopathologic findings of the orbicularis oculi in upper eyelid aging: total or minimal excision of orbicularis oculi in upper blepharoplasty.ArchFacialPlastSurg2012;14(4):253-257
11 De Angelis DD, Carter SR, Seiff SR. Dermatochalasis.IntOphthalmolClin2002;42(2):89-101
12 Deliaert AE, van den Elzen ME, van den Kerckhove E, Fieuws S, van der Hulst RR. Smoking in relation to age in aesthetic facial surgery.AestheticPlastSurg2012;36(4):853-856
13 Bullock JD, Warwar RE, Bienenfeld DG, Marciniszyn SL, Markert RJ. Psychosocial implications ofblepharoptosis and dermatochalasis.TransAmOphthalmolSoc2001;99:65-71;discussion 71-72
14 Bassichis BA. Cosmetic upper-lid blepharoplasty.JOtolaryngolHeadNeckSurg2007;18(3):203-208
15 Karam AM, Lam SM. Management of the aging upper eyelid in the asian patient.FacialPlastSurg2010;26(3):201-208
16 Levine BM, Lelli GJ. Bitemporal hemianopia caused by bilateral blepharoptosis.Orbit2010;29(6): 351-353
17 Boboridis K, Assi A, Indar A, Bunce C, Tyers AG. Repeatability and reproducibility of upper eyelid measurements.BrJOphthalmol2001;85(1):99-101
18 Kanski JJ, Bowling B.Clinicalophthalmology:asystematicapproach. Eyelids-Ptosis. 7th Edition. UK: Elsevier Saunders; 2011: 39-45
19 Balzani A, Chilgar RM, Nicoli M, Sapountzis S, Lazzeri D, Cervelli V, Nicoli F. Novel approach with fractional ultrapulse CO2 laser for the treatment of upper eyelid dermatochalasis and periorbital rejuvenation.LasersMedSci2013;28(6):1483-1487
20 Jung Y, La TY. Blepharoptosis repair through the small orbital septum incision and minimal dissection technique in patients with coexisting dermatochalasis.KoreanJOphthalmol2013;27(1):1-6
21 Dutton JJ, Gayre CS, Proria AD.Diagnosticatlasofcommoneyeliddiseases. USA: Informa Healthcare. 2007:68-69
22 Chen WP, Park JD. Asian upper lid blepharoplasty: an update on indications and technique.FacialPlastSurg2013;29(1):26-31
23 Asano ME, Osaki MH. Quality of life assessment in patients with blepharoptosis.ArqBrasOftalmol2006;69(4):545-549
24 Lee H, Shin H, Park M, Baek S. Comparison of surgical techniques and results of upper blepharoplasty between Asian males and females.AnnPlastSurg2013;70(1):6-9
25 Kim JW, Lee H, Chang M, Park M, Lee TS, Baek S. What causes increased contrast sensitivity and improved functional visual acuity after upper eyelid blepharoplasty?JCraniofacSurg2013;24(5):1582-1585
26 Watanabe A, Selva D, Kakizaki H, Oka Y, Yokoi N, Wakimasu K, Kimura N, Kinoshita S. Long-term tear volume changes after blepharoptosis surgery and blepharoplasty.InvestOphthalmolVisSci2014;56(1):54-58
27 Prado RB, Silva-Junior DE, Padovani CR, Schellini SA. Assessment of eyebrow position before and after upper eyelid blepharoplasty.Orbit2012;31(4):222-226
Feride Aylin Kantarci1, Muhammed Nabi Kantarci2, Mehmet Gurkan Tatar1, Emine Esra Karaca3
(作者单位:1土耳其,伊斯坦布尔,马尔泰佩 34844,法提赫大学医学院,眼科;2土耳其,伊斯坦布尔,Bahçelievler 34196,法医科学研究所,司法行政部,法医学系;3土耳其,约兹加特,索尔贡 66700,索尔贡州立医院,眼科)
摘要
目的:调查眼睑皮肤松垂的位置和程度及是否伴随假性上睑下垂与年龄的关系。
方法:选取113例眼睑皮肤松垂患者纳入本研究,记录患者的年龄,性别及体质指数。于第一眼位检测睑裂高度和睑缘至瞳孔反射点距离(MRD)。皮肤松垂的程度分为1级:皮肤松垂未及睑缘(至少距睑缘1 mm);2级:皮肤松垂达睑缘水平;3级:皮肤松垂越过睑缘前。
结果:患者平均年龄为52.7±8.6(32~74)a。男36例(31.9%),女77例(68.1%)。平均体质指数为30.3±4.7 (21.5~36.6)kg/m2,平均睑裂高度为10.7±1.6 (7~15)mm,平均MRD为3.8±1.2 (1~5) mm。30例(26.5%)患者的皮肤松垂未及睑缘(1级),38例(33.6%)患者位于睑缘水平线(2级),而45例(39.8%)患者越过睑缘前(3级)。50例(44.2%)患者由于皮肤松垂引起假性上睑下垂。皮肤松垂程度在年龄方面的差异显著。皮肤松垂1级和2级患者的平均年龄(50.3±6.6, 50.5±9.5岁)明显低于3级患者年龄(56.0±8.2岁)。假性上睑下垂患者(56.3±8.3岁)的平均年龄明显高于非假性上睑下垂患者(49.8±7.8岁)。对于皮肤松垂严重程度和假性上睑下垂,患者体质指数无显著差别。
结论:皮肤松垂严重程度和假性上睑下垂的发生率随年龄的增长而有所增加。
关键词:年龄;上睑下垂;眼睑皮肤松垂
DOI:10.3980/j.issn.1672-5123.2016.1.05
通讯作者:Feride Aylin Kantarci. ferideaylin@gmail.com
·Original article·

