心理干预配合针灸治疗对小儿脑瘫康复治疗的疗效观察
李星慧 唐菁华 张 会 赵 燕 龚 芸
川北医学院附属医院儿科 南充 637000
心理干预配合针灸治疗对小儿脑瘫康复治疗的疗效观察
李星慧 唐菁华 张 会 赵 燕 龚 芸
川北医学院附属医院儿科 南充 637000
目的 探讨心理干预配合针灸治疗小儿脑瘫康复的临床疗效。方法 选取2010-04—2013-09于我院诊治的116例小儿脑瘫患者,随机分为A组和B组,每组58例,A组采用针灸与运动功能训练相结合的方法治疗;B组在此基础上加用心理干预治疗。评定治疗效果以及患儿运动功能的改善情况。结果 B组总有效率为91.38%,相比于A组的67.24%明显提高(χ2=14.053,P<0.05);2组治疗后6个月GMFM评分相比于治疗前均明显提高,但B组提高幅度更大(P<0.05);6个月~3岁患儿的总有效率为89.70%,明显高于>3~6岁的62.50%,差异有统计学意义(P<0.05)。结论 针灸联合心理干预能够有效改善患者的运动功能,提高治疗效果,改善预后。早期治疗可能治疗效果更佳。
心理干预;针灸;小儿脑瘫康复
小儿脑性瘫痪主要是指患儿大脑在出生1个月前的发育过程中由于某种致病因素所引起的一种脑损伤综合征[13],近年来发病率一直居高不下,临床主要表现为中枢性运动功能障碍和异常姿势[4-5],大部分患儿伴精神发育延迟、癫痫、智力、语言、视听觉、行为以及感知功能等发生障碍,给患儿的身心健康造成严重威胁。目前治疗仍十分棘手,康复治疗仍然是重中之重。本文采用针灸与心理干预相结合治疗小儿脑瘫取得明显效果,现报道如下。
1 资料与方法
1.1 一般资料 选取2010-04—2013-09于我院诊治的116例小儿脑瘫患者,诊断均符合小儿脑瘫座谈会确定的相关标准。纳入标准:年龄6个月~6周岁;存在运动功能障碍。排除标准:合并继发性癫痫、严重心肺器质性病变以及发热患者,施针部位存在皮损或感染者,不能遵医嘱坚持治疗者。所有患儿家属均签署知情同意书。男62例,女54例;年龄6个月~3岁68例,3~6岁48例,平均(3.15±1.98)岁;其中痉挛型61例,迟缓型29例,手足徐动型26例。随机分为A组和B组,每组58例,A组男30例,女28例;平均年龄(3.08±1.63)岁;痉挛29例,迟缓型16例,手足徐动型13例。B组男32例,女26例;平均年龄(3,17±1.86)岁;痉挛32例,迟缓型13例,手足徐动型13例。2组年龄、性别、分型等方面相比较,差异无统计学意义(P>0.05),具有可比性。
1.2 方法 A组采用针灸与运动功能训练相结合治疗,B组在此基础上加用心理干预治疗。
1.2.1 运动功能训练方法:对临床分型以及病情判断后,结合患儿的病情由治疗师开展康复训练,先以物理疗法降低患者的肌张力,然后用Bobath法纠正异常姿势,Vojta法帮助患儿恢复正常运动,根据抬头—翻身—坐—跪—爬行—站立—行走等儿童成长规律进行训练,并进行头部、四肢以及躯干等部位的平衡训练,采用作业治疗对四肢功能以及双手的精细动作进行训练。0.5~1h/次,1次/d,治疗10d后休息10d继续治疗,持续6个月。
1.2.2 针灸治疗方法:头针:选穴包括四神聪、神庭、双侧本神、颞三针、顶颞前斜线、顶旁1、2线以及顶中线等。痉挛性脑瘫刺激宜轻,徐动型脑瘫不留针。体针选穴:上肢瘫选取肩髃、曲池、手三里或合谷;下肢瘫选取解溪、三阴交、足三里、髀关、伏兔或环跳。操作方法:选取上述7~8个穴位,常规消毒后,采用华佗牌针灸针进行操作,快速进行提插或捻转,得气后与SDZ-Ⅱ型号的电针仪连接,电针器上的每对输出连接同侧神经支配肌肉的腧穴,接通电源后选择疏密波并对强度旋钮由小到大进行调节,以针灸部位的肌肉出现轻度收缩为度。30min/次,1次/d,治疗10d后休息10d继续治疗,持续6个月。
1.2.3 心理干预方法:对患儿人格表示尊重,如患儿比较努力或取得进步,及时进行肯定和表扬,仔细分析患儿出现不良行为的原因并对其进行有效引导,对患儿进行分组,定期组织康复比赛项目,让其主动参与某些特定的游戏和活动,鼓励类似病情的患儿相互沟通,相互促进,帮助患儿建立主动解决问题的能力以及社交能力,从而帮助患儿学会在成长过程中积极主动面对问题、解决问题。对家长的不良情绪进行疏导,鼓励家长积极进行配合,从家庭方面给予相应的呵护、理解、沟通,使患儿得到心理上的疏通。
1.3 观察评定指标
1.3.1 疗效评定[6]:按照全国小儿脑瘫学术研讨会制定的相关标准进行评定。显效:运动发育情况、关节活动及协调功能、原始反射、自动反应和肌力等指标均基本恢复正常;有效:以上指标相比于治疗前进步明显;无效:以上各项指标均无显著变化。总有效率为显效率与有效率之和。
1.3.2 运动功能恢复情况评定[7]:采用粗大运动功能评估量表(gross motor function measure,GMFM)分别于治疗前及治疗6个月后对患儿卧位和翻身、坐位和跪、站立位、行走、跑跳等5个功能区的88项指标进行评定,以判断治疗前后患儿的肢体情况。患儿完全不能完成评为0分;完成不足10%的动作评为1分;完成10%~100%的动作评为2分;全部完成动作评为3分。
1.4 统计学处理 将所得数据导入SPSS 15.0软件进行分析,计量资料以均数±标准差(±s)表示,采用t检验,计数资料以频数和百分率(%)表示,采用χ2检验,P<0.05为差异有统计学意义。
2 结果
2.1 临床疗效 B组总有效率明显高于A组,差异有统计学意义(χ2=14.053,P<0.05)。见表1。

表1 2组疗效比较[n(%)]
2.2 运动功能恢复情况 2组患儿GMFM评分差异无统计学意义(P>0.05),治疗后6个月GMFM评分相比于治疗前均明显提高,但B组提高幅度更大,差异有统计学意义(P <0.05)。见表2。
表2 2组GMFM评分情况比较(±s)

表2 2组GMFM评分情况比较(±s)
组别 n 治疗前 治疗6个月后 t值 P值A组58 108.32±51.94 135.85±48.29 7.872 0.000 B组 58 107.79±49.83 169.17±50.64 9.911 0.000 t值1.948 8.383 P值0.061 0.000
2.3 患儿年龄与临床疗效的关系 所有患儿总有效率为78.45%,其中6个月~3岁患儿的总有效率为89.70%,明显高于>3~6岁患儿的62.50%,差异有统计学意义(P<0.05)。见表3。
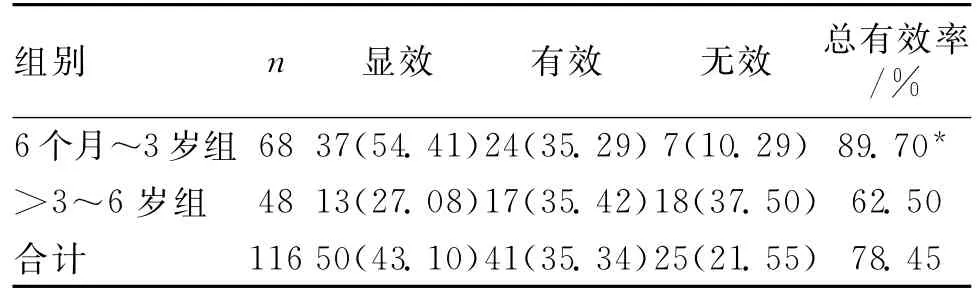
表3 患儿年龄与临床疗效的关系[n(%)]
3 讨论
运动功能以及姿势发生异常是小儿脑瘫重要的临床症状,尤以痉挛型脑瘫的表现最为突出。患儿的肌张力明显增高,肢体关节相对较僵硬,严重影响儿童的生活质量,且易使患儿在成长过程中产生自卑[8-9]、抑郁、焦虑等负性情绪[1012],影响其性格的完善以及治疗效果。本病在中医学中属于“痿证”的范畴[13]。目前,临床尚无特效药物能够有效控制病情,康复治疗仍然是临床关注的焦点,针灸治疗亦是康复治疗的重要手段之一[14-15]。我院通过选择头部的穴位进行针刺,以发挥针灸的近治作用,促进脑细胞的代谢,改善头部的血液循环,对神经元的网络系统进行重建,进而促进患儿运动功能的改善。根据中医“治痿症独取阳明”的理论[16]及患儿肢体运动功能受损情况,重用阳明经的腧穴进行针刺,并采用电针加强刺激强度,有助于从根本上改善患儿的肢体运动功能,符合中医“经脉所至,主治所及”[17]的原理。
本研究中,A组患儿总有效率为67.24%,治疗6个月后GMFM评分相比治疗前均明显提高,提示针灸作为康复治疗的重要方法之一,与其他康复治疗方法相结合,能够有效治疗小儿脑瘫患者的运动功能障碍,改善患儿的临床症状,提高患儿的生活能力。但仍有32.76%的患儿不能达到理想效果,通过长期临床观察,笔者认为患儿的负性情绪是影响治疗效果的重要因素,因此,我院采用针灸治疗与心理干预相结合治疗小儿脑瘫,结果提示,B组患儿的总有效率相比于A组明显提高,差异有统计学意义(P<0.05)。虽然2组治疗后6个月患儿GMFM评分相比于治疗前均明显提高,但B组提高幅度更大,说明心理干预能够使得患儿能够建立比较积极乐观的心态,接受病情,并努力配合治疗,通过病友间的相互交流与鼓励,能够帮助患者树立对治疗的信心,患儿对治疗的依从性明显提高,更加积极乐观,能够达到最佳的治疗效果[18]。在小儿脑瘫康复治疗的过程中,针灸具有双向良性调节的作用[19],临床应用较安全。但6个月~3岁患儿的总有效率明显高于>3~6岁患儿,差异有统计学意义(P<0.05),提示病变早期治疗的重要性。
综上所述,针灸联合心理干预对小儿脑瘫患者具有较好的治疗作用,能够有效改善患儿的运动功能,提高治疗效果,改善预后,早期治疗可能效果更佳。
[1]Zhou J,Liu HY,Deng H.Comparative research and follow-up study on treatment of spastic cerebral palsy with Jiaji(EX-B2)point needling[J].Zhongguo Zhong Xi Yi Jie He Za Zhi,2010,30(9):928-930.
[2]Duncan B,Shen K,Zou LP,et al.Evaluating intense rehabilitative therapies with and without acupuncture for children with cerebral palsy:a randomized controlled trial[J].Arch Phys Med Rehabil,2012,93(5):808-815.
[3]Liu L,Liu LG,LüM,et al.Clinical observation on infantile cerebral palsy treated with quick meridian needling therapy plus scalp acupuncture[J].Zhongguo Zhen Jiu,2010,30(10):826-829.
[4]Han X,Shang Q,Ma BX.Clinical observation on plum-blossom needle on Governor Vessel and point Jiaji(EX-B 2)for treatment of cerebral palsy of involuntary movement[J].Zhongguo Zhen Jiu,2010,30(5):359-363.
[5]Stasolla F,CaffòAO,Picucci L,et al.Assistive technology for promoting choice behaviors in three children with cerebral palsy and severe communication impairments[J].Res Dev Disabil,2013,34(9):2 694-2 700.
[6]Wang SQ,Liang WX,Huang GH,et al.Randomized controlled clinical trials for acupuncture treatment of spastic cerebral palsy children by bilateral horizontal puncturing from Yuzhen(BL 9)to Tianzhu(BL 10)[J].Zhen Ci Yan Jiu,2011,36(3):215-219.
[7]Zhang XJ,Wu Q.Impacts on IEMG of gastrocnemius muscle for children with cerebral palsy treated with different intervention order[J].Zhongguo Zhen Jiu,2012,32(4):301-304.
[8]Al-Gamal E,Long T.Psychological distress and perceived support among Jordanian parents living with a child with cerebral palsy:a cross-sectional study[J].Scand J Caring Sci,2013,27(3):624-631.
[9]Lin KC,Wang TN,Wu CY,et al.Effects of home-based constraint-induced therapy versus dose-matched control intervention on functional outcomes and caregiver well-being in children with cerebral palsy[J].Res Dev Disabil,2011,32(5):1483-1491.
[10]Whittingham K,Bodimeade HL,Lloyd O,et al.Everyday psychological functioning in children with unilateral cerebral palsy:does executive functioning play a role[J].Dev Med Child Neurol,2014,7(2):352-357.
[11]Moreira H,Carona C,Silva N,et al.Psychological and quality of life outcomes in pediatric populations:aparent-child perspective[J].J Pediatr,2013,163(5):1 471-1 478.
[12]Bjorgaas HM,Elgen I,Boe T,et al.Mental health in children with cerebral palsy:does screening capture the complexity[J].Scientific World Journal,2013,13(5):462-468.
[13]Zhang HY,Du F.Clinical trials of acupuncture intervention combined with sitting training for cerebral palsy children with parafunctional sitting position[J].Zhen Ci Yan Jiu,2013,38(5):403-410.
[14]Zhang Y,Lan R,Liu ZH.Impacts on tiptoe deformity and intelligent development in spasmodic cerebral palsy treated with acupuncture at naoqing xue(extra)[J].Zhongguo Zhen Jiu,2013,33(7):595-599.
[15]Nam MJ,Bang YIe,Kim TI.Effects of abdominal meridian massage with aroma oils on relief of constipation among hospitalized children with brain related disabilities[J].J Korean Acad Nurs,2013,43(2):247-255.
[16]Hao JJ,Zhongren S,Xian S,et al.Chinese scalp acupuncture for cerebral palsy in a child diagnosed with stroke in utero[J].Glob Adv Health Med,2012,1(1):14-17.
[17]Zhang HY,Lu SF,Xiao N.Effects of mild warming moxibustion on acupoints Shenque(RN8)and Guanyuan(RN4)for prevention and treatment of recurrent respiratory tract infection in children with cerebral palsy[J].Zhongguo Zhong Xi Yi Jie He Za Zhi,2010,30(9):935-937.
[18]Chen KL,Tseng MH,Shieh JY,et al.Determinants of quality of life in children with cerebral palsy:a comprehensive biopsychosocial approach[J].Res Dev Disabil,2014,35(2):520-528.
[19]Ukhanova TA,Gorbunov FE.Micro-current reflexotherapy in the rehabilitative treatment of the speech function disorders in children withcerebral palsy[J].Vopr Kurortol Fizioter Lech Fiz Kult,2011,3(1):3-6.
(收稿2014-04-14)
Obseruation on the efficacy of psychological intervention plus acupuncture rehabilitation treatment for children with cerebral palsy
Li Xinghui,Tang Jinghua,Zhang Hui,Zhao Yan,Gong Yun
Department of Paediatrics,the Affiliated Hospital of North Sichuan Medical College,Nanchong637000,China
Objective To investigate the clinical efficacy of psychological intervention with acupuncture treatment for rehabilitation of children with cerebral palsy.Methods 116cases of cerebral palsy children from April 2010to September 2013treated in my hospital were randomly divided into group A(n=58,treated by acupuncture combined with functional training and exercise)and group B(n=58,treated by acupuncture combined by functional training and exercise and psychological intervention).Its therapeutic effect and improvement of motor function in children were evaluated.Results Compared to group A with 67.24%,the total effective rate of group B with 91.38%improved significantly(χ2=14.053,P<0.05);GMFM scors after 6 months of treatment in two groups were significantly improved compared with those before treatment,but the group B improved even more sharply(P<0.05);total effective rate for all children was 78.45%,which 6months to 3years old children with the total effective rate of 89.70%,was significantly higher than 62.50%of 3years to 6years old children.Differences were statistically significant(P<0.05).Conclusion Acupuncture combined psychological intervention in children with cerebral palsy have a better therapeutic effect;it can effectively improve the motor function of patients,the therapeutic effect and the prognosis of children.Also,early treatment can cure better.
Psychological intervention;Acupuncture;Pediatric cerebral palsy
R742.3
A
1673-5110(2015)05-0004-03