Unravelling psychosis: psychosocial epidemiology,mechanism, and meaning
Paul BEBBINGTON
•Special article•
Unravelling psychosis: psychosocial epidemiology,mechanism, and meaning
Paul BEBBINGTON
epidemiology; social factors; psychosis; cognitive behavior therapy
1. A sea-change in our understanding of psychotic disorder?
In the last 15 to 20 years there has been a revolution in our understanding of psychosis. It is now acknowledged that there are clear continuities between psychosis and attributes widely distributed in the population. Partly as a result of this new realization, there has been a large accumulation of scientific evidence suggestive of the processes underlying the emergence of psychotic symptoms and, hence, of psychosis itself. This has been aided by the parallel development and elaboration of cognitive behavioral treatments for psychosis (CBT-p).[1]
This work was initiated and carried forward by a loose, informal collective of research groups from centers in different countries and continents. Many,though not all, were concerned with evaluating psychological interventions for psychosis. In the process of developing these interventions, an interlocking set of complementary strategies for the acquisition and analysis of data has evolved. These approaches can be subsumed under the term ‘analytical psychosocial epidemiology’. In this narrative review I will describe how they have led to important new findings which have facilitated the advancement of psychological treatments.
Much of the work on psychosocial processes and treatments in psychosis was initiated in Europe,where there has been an enduring tradition of social psychiatry. More recently, there have been important American and Australasian contributions. CBT-p is now a recommended treatment in several jurisdictions[2-4]although it has yet to be evaluated in a Chinese context.In China there has been work on the effects of family atmosphere and family burden in psychosis[5-11]but relatively little research has focused on the topics covered in this review. There are, however, certainly opportunities for doing this sort of research in Chinese populations, for instance, as part of the epidemiological psychiatric survey recently conducted in Hong Kong.[12]
2. Modelling the symptoms of psychosis
Human societies down the ages have tended to see some of their members as consistently, persistently, and idiosyncratically in error, whether through abnormal perceptions or abnormal beliefs. Such individuals were often marginalized and sometimes identified as mad. Subsequently, in most societies the lay conceptualization of madness was gradually medicalized as different types of psychotic disorder. However, it has long been known that psychotic disorder is variably accompanied by a range of ancillary symptoms that are not intrinsically psychotic. Many of these are aspects of mood.[13]In the past, clinicians have tended to discount these ancillary symptoms as a distraction in the process of diagnosis. They have thus adopted what is essentially atopographical modelof psychosis, in which the psychotic symptoms form a core of interest and the(highly prevalent) ancillary symptoms are regarded as peripheral and incidental (see Figure 1).

Figure 1. Modelling psychosis symptoms:topographical model of psychosis symptoms
Moreover, there is now strong evidence that the core is poorly defined, suggesting that this model is an inadequate reflection of the empirical data.This is because individual psychotic experiences are commonplace in the general population.[15-27]Many people have a few mild or fleeting psychotic symptoms and a few people have many psychotic symptoms.Symptom frequency is distributed in an exponential pattern[21,23,28]as shown by the curve in Figure 2 which used data from the 2000 British National Survey of Psychiatric Morbidity to produce a 14-item scale of paranoia. These are cross-sectional data, so they represent the position of individuals along this curve at a given time. It seems likely that people move along the curve in one direction or another as time passes;[29]for individuals who at some stage meet criteria for a diagnosis of psychosis, such movement along the curve would represent recovery or relapse of their psychotic condition.

Figure 2. The distribution of the total paranoia score, with fitted exponential curve(reproduced with permission from Bebbington et al., 2013[23])
The topographical model of psychosis is topographically inadequate, but it also lacks explanatory value: it offers no theoretical account of how psychotic and non-psychotic symptoms are related. In this respect ahierarchical modelmight seem to be an advance because it would require a non-reflexive relationship between core and associated symptoms, such that core symptoms strongly predict associated symptoms but associated symptoms only weakly predict core symptoms. This does appear to be the case, and has the advantage of suggesting that symptoms are linked by some kind of mechanism: that in some way the coredrivesthe associated symptoms. However, it should be noted that the apparent hierarchy may be (and probably is) an artifact of the relative frequency of core and non-core symptoms. This hierarchical model may be partly true (having a delusion of persecution is likely to be scary and depressing), but it is almost certainly deficient.
2.1 Symptom processes
Most epidemiological research in psychosis has focused on its associations with physical or social environmental factors. Until recently, scant regard has been paid to how these associations might work, that is, how the outside world gets into the inside. The concept of symptom processes offers a possible advance: it postulates that mental entities have relationships with each other that may be causal. This is implicit, for example, in cognitive accounts of depressive disorder, in which the development of the clinical picture is strongly predicated on the capacity of particular thinking patterns to drive changes in mood.[30]
This approach breaches the phenomenological precept that mental states are ultimately reflections of a unitary, indivisible experience,[31]but it does lead to testable hypotheses. In particular, it becomes possible to examine the interrelationship of social environmental factors and the internal features of psychosis. This endeavor has been furthered by analyzing symptoms in terms of correlates that are likely to influence them in distinguishable ways. There is, for instance,good evidence of this sort of multiple influence in paranoia, which is characteristically associated with a worry thinking style, negative thoughts about the self,increased interpersonal sensitivity, anomalous internal experiences, insomnia, and various unusual styles of reasoning.[32-34]
Thus specific ancillary symptoms of psychosis might operate as mediators between external experience and psychotic symptoms; for example, affective symptoms frequently predate the onset of psychosis and presage relapse.[13]As a consequence, the ancillary symptoms provide rational targets for psychological therapy in psychosis. Equally, epidemiological studies are a good way to check out ideas about mechanisms that emerge in therapy. Indeed, this sort of research ideally progresses by a continuing traverse between epidemiology and clinical studies. This crossover has been considerably strengthened by the use of creative secondary analyses of survey datasets and therapy outcome studies.
2.2 A caveat about social variables in psychiatry
There is something unusual about many of the variables used in research in social psychiatry. This is that they are chosen and defined in terms of their supposed effect on mental states. Thus, their definition is based on a consensus derived from researchers’ own capacity for theory of mind. For example, the concept of stressful life events depends on the belief that specific events have the capacity to elicit distress in many or most of those experiencing them.[35,36]The problem with framing social variables in this way is that the circularity inherent in their definition reduces the information content of research based on the variables. Thus one not unreasonable response to the statement that life events judged to be stressful cause distress is‘so what?’.On the other hand, a statement that life events cause depressive disorder has more strength, partly because the definition of depressive disorder connotes features that go beyond mere distress, and partly because the statement opens up the possibility of identifying specific mechanisms for the link between life events and depression.
At first sight, there appears to be little overlap between social experiences and the symptoms of psychosis. This is apparent in the lay conceptualization of madness as something that is ‘incomprehensible’.However, even here, judgments have to be made about the potential social determinants of cases of psychosis;for example, about the extent to which ideas of persecution are consistent and commensurate with real experiences, as they sometimes are. Again, this problem of understanding the overlap of social experiences and psychosis is reduced and partly circumvented in studies of the potential mechanisms linking social experiences to specific psychotic symptoms.
One example of the interleaving of social variables and psychiatric categories is post-traumatic stress disorder (PTSD), a diagnosis that requires both a characteristic stimulus (a life-threatening event) and a characteristic response on the part of the person experiencing the stimulus. Because these defining symptoms of PTSD can be distinguished from those of psychosis, the finding that aspects of PTSD may be involved in the development of psychotic symptoms(particularly hallucinations) is non-circular, and thus provides useful information.[37-40]Another, perhaps weaker, example is the quality ofintrusiveness, wherein individuals are subjected to the apparently arbitrary actions of people who are not close acquaintances.[41]There is some evidence that events with this characteristic are associated with psychosis through their particular links with persecutory ideation.[42,43]Intrusiveness is one of the characteristics of bullying,[44]which is defined in terms of attributes that tend (and are intended) to induce particular responses in victims. In this instance,studies of the mechanism relating bullying and intrusiveness to victims’ responses may reveal what drives the variability in responses to such experiences.
3. Psychosocial epidemiology in the study of psychosis
The most obvious way to study the psychosocial epidemiology of psychosis is to use a diagnosis of psychosis as the dependent variable. However,in acknowledgement of the polythetic nature of psychosis, researchers in this area have also used more specific symptomatic components of psychosis as representative dependent variables: paranoid ideation,hallucinations, and, more rarely, abnormalities of thought. Depending on the particular research question,these specific psychotic symptoms may also be used as independent or mediating variables. Many other types of independent variables are commonly employed in studies of psychosis: subjective experiences such as symptoms of anxiety and depression, and patterns of thought (schemas);[45-47]response styles ascertained through testing, such as the Jumping to Conclusions(JTC) bias;[48-50]environmental experiences including life events in general;[51-53]more specific events such as sexual abuse, physical or emotional abuse, and bullying victimization;[44,54,55]and diffuse environmental attributes, such as urban living.[56,57]The interplay of these environmental influences and mental attributes can be investigated to test hypotheses about the mechanisms that link these variables.
3.1 The creative use of data
Research on psychosis in the last 15 to 20 years has been characterized by the thoughtful use of data of various types and acquired through various designs.To a significant degree, this has been driven by the development of models, which are important methods of summarizing existing knowledge and of using it to suggest potential mechanisms. Models themselves may not be wholly testable, but they do drive testable hypotheses. There have been a number of such models.[58,59]An example based on the work of Garety and colleagues[60]and Kuipers and colleagues[61]is shown in Figure 3. This postulates that vulnerable people respond to stressful events with cognitive, emotional,and perceptual changes, and that these responses bias appraisals in a way that leads to the emergence of positive symptoms of psychosis. These hypothetical links can then be tested out in a variety of empirical studies, including treatment trials.

Figure 3. A cognitive model of the positive symptoms of psychosis(adapted with permission from Garety et al., 2001,[60] and Kuipers et al., 2006[61])
This research has also been advanced by the creative deployment of all the usual techniques of data acquisition, including interviews, questionnaires,and psychological testing procedures. Data are either sampled at a specific point in time or repeatedly over various periods. Some of the techniques have been particularly innovative. For example, Experience Sampling Methodology (ESM), initially described in 1987,[62]has been used to great effect in psychosis research since 2000; it requires participants to record their feelings, thoughts, and situation at random times during the day when cued by a programmed wristwatch alarm.[63,64]It thus provides an additional,intermediate, route to data acquisition that complements more traditional approaches based on retrospective interviewing. Another innovative method involves constraining the environment artificially in order to identify individual differences in response, and using these observed differences to test hypothesized mechanisms. For example, Green and colleagues[65]placed research participants in a waiting room so they could hear simulated laughter in the next room. The most sophisticated way of creating these experimental environments involves virtual reality, which provides an immersive interactive experience, for instance, of a library or a subway.[66]
Recent epidemiological research into the psychological mechanisms involved in psychosis has been governed by an overall strategy that was always at least partly intentional but has become more explicit with the passage of time. This can be described as a process of multipletriangulation. The first element in the strategy is to set up theory-driven hypotheses and to use them in a range of different epidemiological contexts. The second is to use several different measures of psychosis as the dependent variable, including the overall diagnosis, the presence of individual psychotic symptoms (mainly auditory hallucinations and paranoid ideation), and continuous measures of psychotic attributes such as the paranoia score described above. This is a very powerful way of testing theories: the failure to refute the same specific hypotheses in relation to these different measures and diverse contexts adds greatly to the plausibility of the findings. Similarly, associations identified in both cross-sectional and longitudinal analyses allow more confident inference. The availability of data from repeated population surveys using similar or identical methods permits immediate replication, which makes for a particularly stringent test of hypotheses.
3.2 A note on the exploitation of temporal relationships
It is often stated that causal relationships cannot be inferred from cross-sectional studies. This is not so.Whatever the methodology, it is always possible toinfercausality, and, whatever the methodology, it is never possible to be certain of the truth of the inferred causal relationship. One may certainly take account of the results of cross-sectional analyses whenrefutinga hypothesis; so when a hypothesis is not refuted, the result acts to corroborate the hypothesis. At issue is the weight that can be placed on the inference, which is greater in studies where the chosen independent variables clearly precede the chosen dependent variable. However, most of the variables in studies of mental states are extended in time, so restricting sampling to a single time point may induce a spurious confidence in temporal relationships.
The simplest approach to temporal relationships in psychosis research involves a single repetition of measures. A stronger design incorporates multiple repetitions. Experience Sampling Methodology (ESM)is a particular version of this, and raises the question of the proper interval for such studies. It is apparent from ESM research that mental phenomena fluctuate quite rapidly, and thus changes assessed over larger stretches of time must involve some kind of integration of these smaller (‘micro-level’) fluctuations.[46,67]Collip and colleagues[67]suggest that an enduring characteristic of stress sensitivity converts transient psychotic phenomena into more persistent ones. These issues emphasize the need for the triangulation approach described above.
3.3 An example of triangulation
As an example of the triangulation of research in this area, we may consider the link between mood instability and psychosis.[64]The study of affect in psychosis has been based on a number of attributes.These have generally included amplitude (how severe is the disturbance of affect?) and duration (how long has it lasted?). However, theconsistencyof affective disturbance, which incorporates both frequency and amplitude, has been relatively neglected until recently. Emotional regulation is a learnt behavior,characterized by a number of strategies, both adaptive(emotion management, cognitive reappraisal), and maladaptive (experiential avoidance, attentional deployment, dissociation, and alexithymia).[68]A number of consequences are associated with a relative failure to learn these skills. It has mainly been studied in the context of borderline personality disorder and bipolar disorder.[69,70]
Psychotic symptoms fluctuate considerably, as anyone who has tried to define onset, remission and relapse in longitudinal research can testify.[71]Could this variability arise as a consequence of affective fluctuations? If so, this would parallel the altered stress sensitivity identified in studies of psychosis that use Experience Sampling Methodology.[64]Recent studies have confirmed the presence of emotional dysregulation in psychosis.[68,72]
In a study that deliberately followed the triangulation strategy described above, Marwaha and colleagues[73]used the British national surveys of psychiatric morbidity to investigate the hypothesized links between mood instability and psychosis. They first used cross-sectional analyses of the 2000 and 2007 surveys to show that there is a very strong association between mood instability and a diagnosis of psychosis. This relationship remained after controlling for sociodemographic variables and, crucially, the effect of mood instability was still large and significant after controlling forcurrentaffect. This implies that instability has an intrinsic effect that goes beyond mere exposure to affective disturbance. There was also an extremely strong association between mood instability and the specific symptoms of paranoid ideation and auditory hallucinations in both surveys. This association remained after controlling for sociodemographic factors and current affect. Finally, analysis of an 18-month follow-up of over 2000 selected participants in the 2000 survey demonstrated that mood instability at inception predicted the later emergence and maintenance of paranoia, even after controlling for initial affect level.However, the effect of mood instability over time was less clear in relation to individual symptoms: it predicted the emergence of auditory hallucinations at followup, but not if initial affect was controlled; and it did not predict the maintenance of auditory hallucinations at follow-up.
3.4 The analysis of complex relationships
The different analytic possibilities for assessing the interrelationships between environmental variables and symptoms are summarized in Table 1. In addition to establishing two-way relationships between different variables, cross-sectional and longitudinal analyses can both be used to test potential mediation effects.Longitudinal analyses enable testing of hypotheses about the emergence of new symptoms and about the maintenance of symptoms that are already present.Such analyses may be based on straightforward followup studies, but it is also possible to exploit treatment trial data in this way. Depending on the type of treatment and the measures used, clinical trials can also be used to probe mechanisms. Indeed, there is strong argument for designing them to do thisa priori.[46]Experimental manipulations intended to be precursors of new elements of treatment can be designed to test possible mechanisms that are based on specific theories.[74,75]
Traversing between epidemiological surveys and clinical studies is a central element in the process of triangulation. Given a continuous distribution of psychotic experiences and phenomena in the general population, one would hypothesize that most of the correlates in people whose symptoms fell short of the criteria for a diagnosis of a psychotic disorder would overlap with those of clinical psychosis. If this is found to be so, the argument for a continuity between nonclinical psychotic experience and clinical psychosis becomes even more compelling.
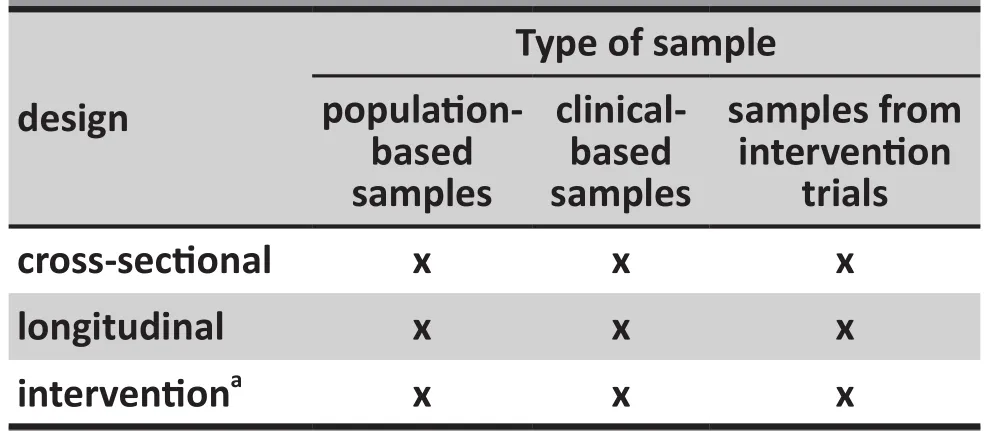
Table 1. The creative use of different data types
3.5 Adversity and psychosis
The evidence for social influences on the experiences,beliefs, and behavior of people with psychosis is now well established. Early work demonstrating the effect of institutional environments[76]was followed by the development of techniques for assessing the effects of the family environment on the course of psychotic illness.[77-79]This led in turn to the development of effective family interventions.[80,81]Technological advances also promoted the study of the role of life events in the onset of episodes of psychosis.[82]However,the subsequent literature has produced results that are variable and difficult to interpret. Beards and colleagues’recent a meta-analysis of life events and psychosis[53]identified 14 studies published between 1968 and 2012 that linked exposure to adult life events to the onset of psychotic episodes or experiences. The authors calculated an overall odds ratio of 3.2, but expressed reservations about the quality of some of the included studies. The growing literature using experience sampling methodology in people with psychosis has also included measures of life events and other stresses;[64]these studies consistently report a relationship between life events and psychotic symptoms that appears to be mediated via an alteration in stress sensitivity.
In contrast to the literature on recent life events,the strong association reported between psychosis and severely traumatic experiences early in life (including child sexual abuse, physical assault, exposure to domestic violence, and bullying) seems more secure.[44,52,54,83-91]Some of these studies are based on the use of existing cohorts and are thus prospective.[91-93]The literature linking sexual abuse to psychosis, including studies that consider the mediating mechanisms underlying this link,has been critically reviewed by Bebbington.[94]It appears that there is a dose-response effect, in that increasing numbers of traumas and increasing severity of individual traumatic events are more strongly associated with the subsequent development of psychosis.[54,95]Although childhood sexual abuse is associated with many psychiatric outcomes, this dose-response effect may be of particular relevance to the onset of psychosis.[54,94,96]
3.6 Studies in the mediation of psychotic disorder
As noted above, many of the ancillary symptoms of psychosis are associated with affect. It is worth considering the role of ancillary symptoms and other psychological attributes in the emergence and maintenance of psychotic symptoms. There is now good evidence for this, based on several sorts of analysis using data from a range of sources. These include several large epidemiological surveys: the British national psychiatric morbidity surveys (especially those of 2000 and 2007),[54,73,86,96-100]the Dutch Netherlands Mental Health Survey and Incidence Study (NEMESIS),[101-103]the English Avon Longitudinal Study of Parents and Children(ALSPAC) study,[92,104], the Dunedin Birth Cohort Study,[105]and the United States National Comorbidity Survey and its replication.[106,107]Other types of studies supporting the mediating role of ancillary symptoms include experience sampling methodology surveys,[108-114]virtual reality studies,[115-119]treatment trials of CBT-p,[46,50,120]and experimental manipulations.[74,75]
Several such studies have been based on the theoretical model of paranoia put forward by Freeman and colleagues,[59]which asserts that negative affect,worry, and insomnia are important determinants of paranoid thinking. According to this theory, anxiety produces anticipation of threat; depression increases the sense of vulnerability; worry leads to implausible ideas; and insomnia exacerbates negative affect and cognition, and creates an altered perceptual state.
People with psychosis have a range of sleep problems, including nightmares.[121]In cross-sectional analyses from the British national psychiatric morbidity surveys, people who had sleep difficulties, insomnia,or chronic insomnia were more than twice as likely to acknowledge that others were deliberately acting to harm them or their interests.[122]These associations were stronger still in relation to the more extreme belief that a group of people was plotting to cause the participant serious harm or injury (with odds ratios rising to 4.5 in the case of chronic insomnia). Moreover,these relationships were equally apparent if the dimensional paranoia score referred to above was used instead of the categorical variables, thus confirming the robustness of the findings.
These authors also studied participants without paranoia at baseline. Those who reported insomnia,worry, anxiety, depression, or depressive ideas were much more likely to develop paranoia (including a severe degree of paranoia) by the time of the 18-month follow-up.[98]Long-term data from the ALSPAC study corroborate these findings: psychotic experiences in adolescence were predicted by nightmares and night terrors in childhood, and were strongly associated with concurrent parasomnias.[92]
Insomnia is a treatable condition.[123,124]If it is indeed a significant driver of paranoia, a crucial test suggests itself: treat the insomnia to treat the paranoia. Myers and colleagues[125]carried out a pilot intervention specifically for insomnia which was successful in improving delusional symptoms in patients with psychosis. A more prolonged randomized controlled trial of a cognitive behavioral intervention for insomnia is now being conducted in patients with delusions or hallucinations.[126]
The Freeman model of paranoia[59]attributes a significant role to worry processes. This implies that direct attempts to modify levels of worry in people with paranoia should also be beneficial. A randomized controlled trial specifically targeting worry in patients with paranoid delusions has just been completed (the Worry Intervention Trial (WIT)).[120]This was successful both in modifying worry and in improving psychotic symptoms; moreover, two-thirds of the treatment effect was mediated through its effect on worry. This confirms that the treatment did what was intended and that there seems to be a causal link between worry and delusion formation.
4. Conclusions
Over the last two decades a large number of studies using increasingly sophisticated methods have established that the external social world has an important influence on the development and persistence of psychotic disorders. Moreover, these studies have demonstrated that the so-called ancillary symptoms of psychosis perform an important role in mediating the effects of the social environment in the generation of psychotic symptoms. It is apparent that there are many routes to psychosis and it takes many forms. It thus seems entirely appropriate that cognitive behavior therapy for psychosis is formulation-based, involving the analysis of the processes that seem to be most important in the individual case and the subsequent deployment of specific techniques to deal with these processes. It thus turns out that psychosis is not ‘un-understandable’:it relates to real-world experience and events, and symptoms do, after all, have meaning. The delineation of the involved processes enriches attempts to treat psychosis using psychological techniques, and the outcome of treatment in turn suggests new directions for research – a productive reciprocal influence.
In this paper, I have chosen to review a particular aspect of the recent literature on psychosis. It should,nevertheless, be acknowledged that there are links between the social and genetic epidemiology of psychosis. For instance, the association between the experience of bullying and psychosis is partly heritable,[127]and the stress sensitivity associated with psychotic-like experiences reported in studies using experience sampling methodology may be partly genetically conditioned.[128]However, genetic studies in psychosis have identified myriad candidate genes of small effect,[129]with no clear implications for treatment. This is not the case with the research on the psychosocial aspects of psychosis.
Conflict of interest
The author declares that he has no conflicts of interest.
Funding
The work for this publication was unfunded.
1. Turner DT, van der Gaag M, Karyotaki E, Cuijpers P.Psychological interventions for psychosis: a meta-analysis of comparative outcome studies.Am J Psychiatry. 2014;171(5): 523-538. doi: http://dx.doi.org/10.1176/appi.ajp.2013.13081159
2. Kreyenbuhl J, Buchanan RW, Dickerson FB, Dixon LB. The Schizophrenia Patient Outcomes Research Team (PORT):updated treatment recommendations 2009.Schizophr Bull.2010; 36(1): 94-103. doi: http://dx.doi.org/10.1093/schbul/sbp130
3. Kuipers E, Yesufu-Udechuku A, Taylor C, Kendall T.Management of psychosis and schizophrenia in adults:summary of updated NICE guidance.BMJ. 2014; 348: g1173.doi: http://dx.doi.org/10.1136/bmj.g1173
4. Nordentoft M, Austin S. CBT for psychotic disorders: beyond meta-analyses and guidelines - it is time to implement!World Psychiatry. 2014; 13(3): 260-261. doi: http://dx.doi.org/10.1002/wps.20164
5. Phillips MR, Pearson V, Li F, Xu M, Yang L. Stigma and expressed emotion: a study of people with schizophrenia and their family members in China.Br J Psychiatry. 2002;181: 488-493
6. Ran MS, Leff J, Hou ZJ, Xiang MZ, Chan CL. The characteristics of expressed emotion among relatives of patients with schizophrenia in Chengdu, China.Cult Med Psychiatry. 2003;27(1): 95-106. doi: http://dx.doi.org/10.1023/A:1023636021995
7. Yang LH, Phillips MR, Licht DM, Hooley JM. Causal attributions about schizophrenia in families in China: expressed emotion and patient relapse.J Abnorm Psychol. 2004;113(4): 592-602. doi: http://dx.doi.org/10.1037/0021-843X.113.4.592
8. Li Z, Arthur D. A study of three measures of expressed emotion in a sample of Chinese families of a person with schizophrenia.J Psychiatr Ment Health Nurs. 2005;12(4): 431-438. doi: http://dx.doi.org/10.1111/j.1365-2850.2005.00858.x
9. Chien WT, Lee IY. The schizophrenia care management program for family caregivers of Chinese patients with schizophrenia.Psychiatr Serv. 2010; 61: 317-320. doi: http://dx.doi.org/10.1176/appi.ps.61.3.317
10. Chow W, Law S, Andermann L, Yang J, Leszcz M, Wong J,et al. Multi-family psycho-education group for assertive community treatment clients and families of culturally diverse background: a pilot study.Community Ment Health J. 2010; 46(4): 364-371. doi: http://dx.doi.org/10.1007/s10597-010-9305-5
11. Chien WT, Chan ZC, Chan SW. Testing the psychometric properties of a Chinese version of the level of expressed emotion scale.Scientific World Journal. 2014; 2014(2014).doi: http://dx.doi.org/10.1155/2014/905950
12. Lam LCW, Chan WC, Wong CSM, Chen EYH, Ng RMK, Lee EHM, et al. The Hong Kong mental morbidity survey team.the Hong Kong mental morbidity survey: background and study design.East Asian Arch Psychiatry. 2014; 24: 30-36
13. Häfner H, Maurer K, an der Heiden W. ABC Schizophrenia study: an overview of results since 1996.Soc Psychiatry Psychiatr Epidemiol. 2013; 48(7): 1021-1031. doi: http://dx.doi.org/10.1007/s00127-013-0700-4
14. Carragher N, Krueger RF, Eaton NR, Slade T. Disorders without borders: current and future directions in the metastructure of mental disorders.Soc Psychiatry Psychiatr Epidemiol. 2015; 50: 339-350 doi: http://dx.doi.org/10.1007/s00127-014-z. [Epub ahead of print]
15. van Os J, Verdoux H, Maurice-Tison S, Gay B, Liraud F,Salamon R, et al. Self-reported psychosis-like symptoms and the continuum of psychosis.Soc Psychiatry Psychiatr Epidemiol. 1999; 34: 459-463
16. Johns LC, Cannon M, Singleton N, Murray RM, Farrell M,Brugha T, et al. Prevalence and correlates of self-reported psychotic symptoms in the British population.Br J Psychiatry.2004; 185: 298-305
17. Shevlin M, Adamson G, Vollebergh W, de Graaf R, van Os J. An application of item response mixture modelling to psychosis indicators in two large community samples.Soc Psychiatry Psychiatr Epidemiol. 2007; 42(10): 771-779. doi:http://dx.doi.org/10.1007/s00127-007-0244-6
18. Shevlin M, Murphy J, Dorahy MJ, Adamson G. The distribution of positive psychosis-like symptoms in the population: a latent class analysis of the National Comorbidity Survey.Schizophr Res. 2007; 89: 101-109.doi: http://dx.doi.org/10.1016/j.schres.2006.09.014
19. Morrison AP, French P, Wells A. Metacognitive beliefs across the continuum of psychosis: comparisons between patients with psychotic disorders, patients at ultra-high risk and nonpatients.Behav Res Ther. 2007; 45: 2241-2246. doi: http://dx.doi.org/10.1016/j.brat.2007.01.002
20. van Os J, Linscott RJ, Myin-Germeys I, Delespaul P,Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis pronenesspersistence-impairment model of psychotic disorder.Psychol Med. 2009; 39(2): 179-195. doi: http://dx.doi.org/10.1017/S0033291708003814
21. Nuevo R, Chatterji S, Verdes E, Naidoo N, Arango C, Ayuso-Mateos JL. The continuum of psychotic symptoms in the general population: a cross-national study.Schizophr Bull.2012; 38: 475-485. doi: http://dx.doi.org/10.1093/schbul/sbq09
22. Rössler W, Hengartner MP, Ajdacic-Gross V, Haker H, Angst J. Sex differences in sub-clinical psychosis--results from a community study over 30 years.Schizophr Res. 2012; 139:176-182. doi: http://dx.doi.org/10.1016/j.schres.2012.04.0
23. Bebbington PE, McBride O, Steel C, Kuipers E, Radovanovic M, Brugha T, et al.The structure of paranoia in the general population.Br J Psychiatry. 2013; 202(6): 419-427. doi:http://dx.doi.org/10.1192/bjp.bp.112.119032
24. Taylor HE, Stewart SL, Dunn G, Parker S, Fowler D, Morrison AP. Core schemas across the continuum of psychosis:a comparison of clinical and non-clinical groups.Behav Cogn Psychother. 2014; 42(6): 718-730. doi: http://dx.doi.org/10.1017/S1352465813000593
25. Tesli M, Espeseth T, Bettella F, Mattingsdal M, Aas M, Melle I, et al. Polygenic risk score and the psychosis continuum model.Acta Psychiatr Scand. 2014; 130(4): 311-317. doi:http://dx.doi.org/10.1111/acps.12307
26. van Os J. The many continua of psychosis.JAMA Psychiatry.2014; 71: 985-986. doi: http://dx.doi.org/10.1001/jamapsychiatry.2014.1068
27. Zavos HM, Freeman D, Haworth CM, McGuire P, Plomin R, Cardno AG, et al. Consistent etiology of severe,frequent psychotic experiences and milder, less frequent manifestations: a twin study of specific psychotic experiences in adolescence.JAMA Psychiatry. 2014; 71(9): 1049-1057.doi: http://dx.doi.org/10.1001/jamapsychiatry.2014.994
28. Wong KK, Freeman D, Hughes C. Suspicious young minds:paranoia and mistrust in 8- to 14-year-olds in the U.K. and Hong Kong.Br J Psychiatry. 2014; 205(3): 221-229. doi:http://dx.doi.org/10.1192/bjp.bp.113.135467
29. Kaymaz N, Drukker M, Lieb R, Wittchen HU, Werbeloff N,Weiser M, et al. Do subthreshold psychotic experiences predict clinical outcomes in unselected non-help-seeking population-based samples? a systematic review and meta-analysis, enriched with new results.Psychol Med.2012; 42(11): 2239-2253. doi: http://dx.doi.org/10.1017/S0033291711002911
30. Bebbington PE. Three cognitive theories of depression.Psychol Med. 1985; 15: 759771
31. Skodlar B, Henriksen MG, Sass LA, Nelson B, Parnas J.Cognitive-behavioral therapy for schizophrenia: a critical evaluation of its theoretical framework from a clinicalphenomenological perspective.Psychopathology. 2013;46(4): 249-265. doi: http://dx.doi.org/10.1159/000342536
32. Beards S, Fisher HL. The journey to psychosis: an exploration of specific psychological pathways.Soc Psychiatry Psychiatr Epidemiol. 2014; 49: 1541-1544. doi: http://dx.doi.org/10.1007/s00127-014-0953-6
33. Bentall RP, de Sousa P, Varese F, Wickham S, Sitko K,Haarmans M, et al. From adversity to psychosis: pathways and mechanisms from specific adversities to specific symptoms.Soc Psychiatry Psychiatr Epidemiol. 2014; 49: 1011-1022. doi:http://dx.doi.org/10.1007/s00127-014-0914-0
34. Freeman D, Garety P. Advances in understanding and treating persecutory delusions: a review.Soc Psychiatry Psychiatr Epidemiol. 2014; 49: 1179-1189. doi: http://dx.doi.org/10.1007/s00127-014-0928-7
35. Brown GW. Meaning, measurement and the stress of life events. In: Dohrenwend BS, Dohrenwend BP, editors.Stressful Life Events: Their Nature and Effects. New York:John Wiley & Sons; 1974. p. 217-243
36. Bebbington PE. George W. Brown - The science of meaning and the meaning of science. In: Harris T, editor.Where Inner and Outer Worlds Meet. London: Routledge; 2000. p. 71-78
37. Hardy A, Fowler D, Freeman D, Smith B, Steel C, Evans J,et al. Trauma and hallucinatory experience in psychosis.J Nerv Ment Dis. 2005; 193: 501-507. doi: http://dx.doi.org/10.1097/01.nmd.0000172480.56308.21
38. Gracie A, Freeman D, Green S, Garety PA, Kuipers E, Hardy A, et al. The association between traumatic experience,paranoia and hallucinations: a test of the predictions of psychological models.Acta Psychiatr Scand. 2007;116(4): 280-289. doi: http://dx.doi.org/10.1111/j.1600-0447.2007.01011.x
39. Soosay I, Silove D, Bateman-Steel C, Steel Z, Bebbington P,Jones PB, et al. Trauma exposure, PTSD and psychotic-like symptoms in post-conflict Timor Leste: an epidemiological survey.BMC Psychiatry. 2012; 12: 229. doi: http://dx.doi.org/10.1186/1471-244X-12-229
40. Longden E, Madill A, Waterman MG. Dissociation,trauma, and the role of lived experience: toward a new conceptualization of voice hearing.Psychol Bull. 2012;138(1): 28-76. doi: http://dx.doi.org/10.1037/a0025995
41. Harris T. Recent developments in the study of life events in relation to psychiatric and physical disorders. In: Cooper B, editor.Psychiatric Epidemiology. London: Croom-Helm;1987. p. 81-103
42. Raune D, Bebbington P, Dunn GD, Kuipers E. Event attributes and the content of psychotic experiences in first episode psychosis.Psychol Med. 2006; 188(2): 221-230. doi: http://dx.doi.org/10.1017/S003329170500615X
43. Raune D, Kuipers E, Bebbington P. Stressful and intrusive life events preceding first episode psychosis.Epidemiol Psichiatr Soc. 2009; 8: 221-228. doi: http://dx.doi.org/10.1017/S1121189X00000506
44. Catone G, Marwaha S, Kuipers E, Lennox B, Freeman D,Bebbington P, et al. Bullying victimization and psychotic phenomena: analyses of British National Survey data.Lancet Psychiatry. 2015; (in press)
45. Fowler D, Freeman D, Smith B, Kuipers E, Bebbington P,Bashforth H, et al. The Brief Core Schema Scales (BCSS):Psychometric properties and associations with paranoia and grandiosity in non-clinical and psychosis samples.Psychol Med. 2006; 36: 749-759. doi: http://dx.doi.org/10.1017/S0033291706007355
46. Fowler D, Hodgekins J, Garety P, Freeman D, Kuipers E, Dunn G, et al. Negative cognition, depressed mood and paranoia:A longitudinal pathway analysis using structural equation modelling.Schizophr Bull. 2012; 38(5): 1063-1073. doi:http://dx.doi.org/10.1093/schbul/sbr019
47. Morrison AP, French P, Wells A. Metacognitive beliefs across the continuum of psychosis: comparisons between patients with psychotic disorders, patients at ultra-high risk and nonpatients.Behav Res Ther.2007; 45: 2241-2246. doi: http://dx.doi.org/10.1016/j.brat.2007.01.002
48. Garety PA, Hemsley DR, Wessely S. Reasoning in deluded schizophrenic and paranoid patients. Biases in performance on a probabilistic inference task.J Nerv Ment Dis. 1991; 179:194-201
49. Garety PA, Freeman D, Jolley S, Dunn G, Bebbington PE,Fowler DG, et al. Reasoning, emotions, and delusional conviction in psychosis.J Abnorm Psychol. 2005; 114: 373-384. doi: http://dx.doi.org/10.1037/0021-843X.114.3.373
50. So SH, Freeman D, Dunn G, Kapur S, Kuipers E, Bebbington P, et al. Jumping to conclusions, a lack of belief flexibility and delusional conviction in psychosis: a longitudinal investigation of the structure, frequency, and relatedness of reasoning biases.J Abnorm Psychol. 2012; 121(1): 129-139.doi: http://dx.doi.org/10.1037/a0025297
51. Bebbington PE, Wilkins S, Jones P, Foerster A, Murray RM,Toone B, et al. Life events and psychosis: Initial results from the Camberwell Collaborative Psychosis Study.Br J Psychiatry. 1993; 162: 7279
52. Shevlin M, Houston JE, Dorahy MJ, Adamson G.Cumulative traumas and psychosis: an analysis of the national comorbidity survey and the British Psychiatric Morbidity Survey.Schizophr Bull. 2008; 34(1): 193-199. doi:http://dx.doi.org/10.1093/schbul/sbm069
53. Beards S, Gayer-Anderson C, Borges S, Dewey ME, Fisher HL, Morgan C. Life events and psychosis: a review and metaanalysis.Schizophr Bull. 2013; 39(4): 740-747. doi: http://dx.doi.org/10.1093/schbul/sbt065
54. Bebbington PE, Jonas S, Kuipers E, King M, Cooper C, Brugha T, et al. Sexual abuse and psychosis: data from an English National Survey.Br J Psychiatry. 2011; 199(1): 29-37. doi:http://dx.doi.org/10.1192/bjp.bp.110.083642
55. van Dam DS, van der Ven E, Velthorst E, Selten JP, Morgan C, de Haan L. childhood bullying and the association with psychosis in non-clinical and clinical samples:a review and meta-analysis.Psychol Med. 2012; 42: 2463-2474. doi: http://dx.doi.org/10.1017/S0033291712000360
56. Vassos E, Pedersen CB, Murray RM, Collier DA, Lewis CM. Meta-analysis of the association of urbanicity with schizophrenia.Schizophr Bull. 2012 38(6): 1118-1123. doi:10.1093/schbul/sbs096.
57. Padhy SK, Sarkar S, Davuluri T, Patra BN. Urban living and psychosis - An overview.Asian J Psychiatr. 2014; 12C:17-22. doi: http://dx.doi.org/10.1016/j.ajp.2014.09.006
58. Morrison AP. The interpretation of intrusions in psychosis:an integrative cognitive approach to hallucinations and delusions.Behav Cogn Psychother. 2001; 29(3): 257-276.doi: http://dx.doi.org/10.1017/S1352465801003010
59. Freeman D, Garety P, Kuipers E, Fowler D, Bebbington PE. A cognitive model of persecutory delusions.Br J Clin Psychol.2002; 41: 331-347. doi: http://dx.doi.org/10.1348/014466502760387461
60. Garety P, Kuipers E, Fowler D, Freeman D, Bebbington P. Theoretical paper: A cognitive model of the positive symptoms of psychosis.Psychol Med. 2001; 31: 189-195
61. Kuipers E, Garety P, Fowler D, Freeman, D, Dunn G,Bebbington P. Cognitive, emotional and social processes in psychosis: refining cognitive behavioural therapy for persistent positive symptoms.Schizophr Bull. 2006; 32(suppl 1): S24-S31. doi: http://dx.doi.org/10.1093/schbul/sbl014
62. Csikszentmihalyi M, Larson R. Validity and reliability of the Experience-Sampling Method.J Nerv Ment Dis. 1987; 175:526-536
63. Myin-Germeys I, van Os J, Schwartz JE, Stone AA, Delespaul PA. Emotional reactivity to daily life stress in psychosis.Arch Gen Psychiatry. 2001; 58(12): 1137-1144. doi: http://dx.doi.org/10.1001/archpsyc.58.12.1137
64. Myin-Germeys I, van Os J. Stress-reactivity in psychosis:evidence for an affective pathway to psychosis.Clin Psychol Rev. 2007; 27: 409-424. doi: http://dx.doi.org/10.1016/j.cpr.2006.09.005
65. Green CE, Freeman D, Kuipers E, Bebbington P, Fowler D,Dunn G, et al. Paranoid explanations of experience: a novel experimental study.Behav Cogn Psychother. 2011; 39(1): 21-34. doi: http://dx.doi.org/10.1017/S1352465810000457
66. Freeman D, Slater M, Bebbington PE, Garety PA, Kuipers E, Fowler D, et al. Can virtual reality be used to investigate persecutory ideation?J Nerv Ment Dis. 2003; 191: 509-514.doi: http://dx.doi.org/10.1097/01.nmd.0000082212.83842.fe
67. Collip D, Wigman JT, Myin-Germeys I, Jacobs N, Derom C, Thiery E, et al. From epidemiology to daily life: linking daily life stress reactivity to persistence of psychotic experiences in a longitudinal general population study.PLoS One. 2013; 8: e62688. doi: http://dx.doi.org/10.1371/journal.pone.0062688
68. O’Driscoll C, Laing J, Mason O. Cognitive emotion regulation strategies, alexithymia and dissociation in schizophrenia, a review and meta-analysis.Clin Psychol Rev. 2014; 34: 482-495. doi: http://dx.doi.org/10.1016/j.cpr.2014.07.002
69. Koenigsberg HW. Affective instability: toward an integration of neuroscience and psychological perspectives.J Pers Disord. 2010; 24(1): 60-82. doi: http://dx.doi.org/10.1521/pedi.2010.24.1.60
70. Perugi G, Fornaro M, Akiskal HS. Are atypical depression,borderline personality disorder and bipolar II disorder overlapping manifestations of a common cyclothymic diathesis?World Psychiatry. 2011; 10: 45-51. doi: http://dx.doi.org/10.1002/j.2051-5545.2011.tb00013.x
71. Bebbington PE, Craig T, Garety P, Fowler D, Dunn G, Colbert S, et al. Remission and relapse in psychosis: operational definitions based on case-note data.Psychol Med.2006; 36: 1551-1562. doi: http://dx.doi.org/10.1017/S0033291706008579
72. Strauss GP, Kappenman ES, Culbreth AJ, Catalano LT, Lee BG,Gold JM. Emotion regulation abnormalities in schizophrenia:cognitive change strategies fail to decrease the neural response to unpleasant stimuli.Schizophr Bull. 2013; 39:872-883. doi: http://dx.doi.org/10.1093/schbul/sbs186
73. Marwaha S, Broome M, Bebbington P, Kuipers E, Freeman D.Mood instability and psychosis: analyses of British national survey data.Schizophr Bull. 2014; 40(2): 269-277. doi:http://dx.doi.org/10.1093/schbul/sbt149
74. Freeman D, Emsley R, Dunn G, Fowler D, Bebbington P,Kuipers E, et al. The stress of the street for patients with persecutory delusions: a test of the symptomatic and psychological effects of going outside into a busy urban area.Schizophr Bull. 2014; pii: sbu173. doi: http://dx.doi.org/10.1093/schbul/sbu173
75. Garety P, Waller H, Emsley R, Jolley S, Kuipers E, Bebbington P, et al. Cognitive mechanisms of change in delusions: an experimental investigation targeting reasoning to effect change in paranoia.Schizophr Bull. 2014; 41: 400-410 pii:sbu103. doi: http://dx.doi.org/10.1093/schbul/sbu103
76. Wing JK, Brown GW.Institutionalism and schizophrenia.Cambridge UK: Cambridge University Press; 1970
77. Brown GW, Birley JL, Wing JK. Influence of family life on the course of schizophrenic disorders: a replication.Br J Psychiatry. 1972; 121: 241-258
78. Bebbington P, Kuipers L. The predictive utility of expressed emotion in schizophrenia: an aggregate analysis.Psychol Med. 1994; 24(3): 707-718. doi: http://dx.doi.org/10.1017/S0033291700027860
79. Kuipers E, Onwumere J, Bebbington P. Cognitive model of caregiving in psychosis.Br J Psychiatry. 2010; 196(4): 259-265. doi: http://dx.doi.org/10.1192/bjp.bp.109.070466
80. Leff J, Kuipers L, Berkowitz R, Eberlein-Vries R, Sturgeon D.A controlled trial of social intervention in the families of schizophrenic patients.Br J Psychiatry. 1982; 141: 121-134
81. Pilling S, Bebbington P, Kuipers E, Garety P, Geddes J, Orbach G, et al. Psychological treatments in schizophrenia: I. Metaanalysis of family intervention and cognitive behaviour therapy.Psychol Med. 2002; 32(5): 763-782. doi: http://dx.doi.org/10.1017/S0033291702005895
82. Brown GW, Birley JL. Crises and life changes and the onset of schizophrenia.J Health Soc Behav. 1968; 9: 203-214
83. Janssen I, Krabbendam L, Bak M, Hanssen M, Vollebergh W, de Graaf R, et al. Childhood abuse as a risk factor for psychotic experiences.Acta Psychiatr Scand. 2004;109(1): 38-45. doi: http://dx.doi.org/10.1046/j.0001-690X.2003.00217.x
84. Morgan C, Fisher H. Environment and schizophrenia:environmental factors in schizophrenia: childhood trauma--a critical review.Schizophr Bull. 2007; 33(1): 3-10. doi: http://dx.doi.org/10.1093/schbul/sbl053
85. Shevlin M, Murphy J, Read J, Mallett J, Adamson G, Houston JE. Childhood adversity and hallucinations: a communitybased study using the National Comorbidity Survey Replication.Soc Psychiatry Psychiatr Epidemiol. 2011;46(12): 1203-1210. doi: http://dx.doi.org/10.1007/s00127-010-0296-x
86. Shevlin M, O’Neill T, Houston JE, Read J, Bentall RP, Murphy J. Patterns of lifetime female victimisation and psychotic experiences: a study based on the UK Adult Psychiatric Morbidity Survey 2007.Soc Psychiatry Psychiatr Epidemiol. 2013; 48(1): 15-24. doi: http://dx.doi.org/10.1007/s00127-012-0573-y
87. Varese F, Smeets F, Drukker M, Lieverse R, Lataster T, Viechtbauer W, et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control,prospective- and cross-sectional cohort studies.Schizophr Bull. 2012; 38(4): 661-671. doi: http://dx.doi.org/10.1093/schbul/sbs050
88. van Winkel R, van Nierop M, Myin-Germeys I, van Os J.Childhood trauma as a cause of psychosis: linking genes,psychology, and biology.Can J Psychiatry. 2013; 58: 44-51
89. Bentall RP, de Sousa P, Varese F, Wickham S, Sitko K, Haarmans M, et al. From adversity to psychosis: pathways and mechanisms from specific adversities to specific symptoms.Soc Psychiatry Psychiatr Epidemiol. 2014; 49(7):1011-1022. doi: http://dx.doi.org/10.1007/s00127-014-0914-0
90. Velikonja T, Fisher HL, Mason O, Johnson S. Childhood trauma and schizotypy: a systematic literature review.Psychol Med. 2014; 2: 1-17. doi: http://dx.doi.org/10.1017/S0033291714002086
91. Cutajar MC, Mullen PE, Ogloff JR, Thomas SD, Wells DL, Spataro J. Schizophrenia and other psychotic disorders in a cohort of sexually abused children.Arch Gen Psychiatry. 2010; 67(11): 1114-1119. doi: http://dx.doi.org/10.1001/archgenpsychiatry.2010.147
92. Fisher HL, Schreier A, Zammit S, Maughan B, Munafò MR, Lewis G, et al. Pathways between childhood victimization and psychosis-like symptoms in the ALSPAC birth cohort.Schizophr Bull. 2013; 39(5): 1045-1055. doi:http://dx.doi.org/10.1093/schbul/sbs088
93. Thompson AD, Nelson B, Yuen HP, Lin A, Amminger GP,McGorry PD, et al. Sexual trauma increases the risk of developing psychosis in an ultra high-risk “prodromal”population.Schizophr Bull. 2014; 40: 697-706. doi: http://dx.doi.org/10.1093/schbul/sbt032
94. Bebbington PE. Towards a social aetiology of psychosis:the case of child sexual abuse. In: A.S. David AS, Kapur S, McGuffin P, editors.Schizophrenia: The Final Frontier:A Festschrift for Robin M Murray. Hove and New York:Psychology Press; Taylor & Francis group; 2011. p: 259-272
95. Read J, Bentall RP, Fosse R. Time to abandon the biobio-bio model of psychosis: Exploring the epigenetic and psychological mechanisms by which adverse life events lead to psychotic symptoms.Epidemiol Psichiatr Soc. 2009; 18: 299-310. doi: http://dx.doi.org/10.1017/S1121189X00000257
96. Jonas S, Bebbington P, McManus S, Meltzer H, Jenkins R,Kuipers E, et al. Sexual abuse and psychiatric disorder in England: results from the 2007 Adult Psychiatric Morbidity Survey.Psychol Med. 2011; 41(4): 709-719. doi: http://dx.doi.org/10.1017/S003329171000111X
97. Freeman D, McManus S, Brugha T, Meltzer H, Jenkins R, Bebbington P. Concomitants of paranoia in the general population.Psychol Med. 2011; 41(5): 923-936. doi: http://dx.doi.org/10.1017/S0033291710001546
98. Freeman D, Stahl D, McManus S, Meltzer H, Brugha T, Wiles N, Bebbington P. Insomnia, worry, anxiety and depression as predictors of the occurrence and persistence of paranoid thinking.Soc Psychiatry Psychiatr Epidemiol. 2012; 47(8):1195-1203. doi: http://dx.doi.org/10.1007/s00127-011-0433-1
99. Bentall RP, Wickham S, Shevlin M, Varese F. Do specific earlylife adversities lead to specific symptoms of psychosis? A study from the 2007 the Adult Psychiatric Morbidity Survey.Schizophr Bull. 2012; 38: 734-740. doi: 10.1093/schbul/sbs049
100. Wickham S, Taylor P, Shevlin M2, Bentall RP. The impact of social deprivation on paranoia, hallucinations, mania and depression: the role of discrimination social support, stress and trust.PLoS One. 2014; 9(8): e105140. doi: http://dx.doi.org/10.1371/journal.pone.0105140
101. Hanssen M, Bak M, Bijl R, Vollebergh W, van Os J. The incidence and outcome of subclinical psychotic experiences in the general population.Br J Clin Psychol. 2005; 44(Pt 2):181-191. doi: http://dx.doi.org/10.1348/014466505X29611
102. Cougnard A, Marcelis M, Myin-Germeys I, De Graaf R, Vollebergh W, Krabbendam L, et al. Does normal developmental expression of psychosis combine with environmental risk to cause persistence of psychosis?A psychosis proneness-persistence model.Psychol Med.2007; 37: 513-527. doi: http://dx.doi.org/10.1017/S0033291706009731
103. van Nierop M, van Os J, Gunther N, van Zelst C, de Graaf R,ten Have M, et al. Does social defeat mediate the association between childhood trauma and psychosis? Evidence from the NEMESIS-2 Study.Acta Psychiatr Scand. 2014; 129(6):467-476. doi: http://dx.doi.org/10.1111/acps.12212
104. Fisher HL, Lereya ST, Thompson A, Lewis G, Zammit S, Wolke D. Childhood parasomnias and psychotic experiences at age 12 years in a United Kingdom birth cohort.Sleep. 2014;37(4): 475-482. doi: http://dx.doi.org/10.5665/sleep.3478
105. Fisher HL, Caspi A, Poulton R, Meier MH, Houts R, Harrington H, et al. Specificity of childhood psychotic symptoms for predicting schizophrenia by 38 years of age: a birth cohort study.Psychol Med. 2013; 43(10): 2077-2086. doi: http://dx.doi.org/10.1017/S0033291712003091
106. Houston JE, Murphy J, Adamson G, Stringer M, Shevlin M. Childhood sexual abuse, early cannabis use,and psychosis: testing an interaction model based on the National Comorbidity Survey.Schizophr Bull. 2008;34(3): 580-585. doi: http://dx.doi.org/10.1093/schbul/sbm127
107. Sitko K, Bentall RP, Shevlin M, O’Sullivan N, Sellwood W.Associations between specific psychotic symptoms and specific childhood adversities are mediated by attachment styles: an analysis of the National Comorbidity Survey.Psychiatry Res. 2014; 217: 202-209. doi: http://dx.doi.org/10.1016/j.psychres.2014.03.019
108. Delespaul P, deVries M, van Os J. Determinants of occurrence and recovery from hallucinations in daily life.Soc Psychiatry Psychiatr Epidemiol. 2002; 37(3): 97-104. doi:http://dx.doi.org/10.1007/s001270200000
109. Oorschot M, Kwapil T, Delespaul P, Myin-Germeys I.Momentary assessment research in psychosis.Psychol Assess. 2009; 21(4): 498-505. doi: http://dx.doi.org/10.1037/a0017077
110. Thewissen V, Bentall RP, Oorschot M, A Campo J, van Lierop T, van Os J, et al. Emotions, self-esteem, and paranoid episodes: an experience sampling study.Br J Clin Psychol. 2011; 50(2): 178-195. doi: http://dx.doi.org/10.1348/014466510X508677
111. Collip D, Oorschot M, Thewissen V, Van Os J, Bentall R, Myin-Germeys I. Social world interactions: how company connects to paranoia.Psychol Med. 2011; 41(5): 911-921. doi: http://dx.doi.org/10.1017/S0033291710001558
112. Hartley S, Haddock G, Vasconcelos E Sa D, Emsley R,Barrowclough C. An experience sampling study of worry and rumination in psychosis.Psychol Med. 2014; 44: 1605-1614.doi: http://dx.doi.org/10.1017/S0033291713002080
113. So SH, Peters ER, Swendsen J, Garety PA, Kapur S. Changes in delusions in the early phase of antipsychotic treatment - an experience sampling study.Psychiatry Res. 2014; 215: 568-573. doi: http://dx.doi.org/10.1016/j.psychres.2013.12.033
114. Udachina A, Varese F, Myin-Germeys I, Bentall RP. The role of experiential avoidance in paranoid delusions:an experience sampling study.Br J Clin Psychol. 2014; 53(4):422-432. doi: http://dx.doi.org/10.1111/bjc.12054
115. Freeman D, Pugh K, Antley A, Slater M, Bebbington P, Gittins M, et al. Virtual reality study of paranoid thinking in the general population.Br J Psychiatry. 2008; 192(4): 258-263.doi: http://dx.doi.org/10.1192/bjp.bp.107.044677
116. Freeman D, Pugh K, Vorontsova N, Antley A, Slater M. Testing the continuum of delusional beliefs: an experimental study using virtual reality.J Abnorm Psychol. 2010; 119(1): 83-92.doi: http://dx.doi.org/10.1037/a0017514
117. Freeman D, Evans N, Lister R, Antley A, Dunn G,Slater M. Height, social comparison, and paranoia: an immersive virtual reality experimental study.Psychiatry Res. 2014; 218: 348-352. doi: http://dx.doi.org/10.1016/j.psychres.2013.12.014
118. Freeman D, Antley A, Ehlers A, Dunn G, Thompson C,Vorontsova N, et al. The use of immersive virtual reality (VR)to predict the occurrence 6 months later of paranoid thinking and posttraumatic stress symptoms assessed by self-report and interviewer methods: a study of individuals who have been physically assaulted.Psychol Assess. 2014;26(3): 841-847. doi: http://dx.doi.org/10.1037/a0036240
119. Atherton S, Antley A, Evans N, Cernis E, Lister R, Dunn G, et al. Self-Confidence and paranoia: an experimental study using an immersive virtual reality social situation.Behav Cogn Psychother. 2014; 11: 1-9. doi: http://dx.doi.org/10.1017/S1352465814000496
120. Freeman D, Dunn G, Startup H, Pugh K, Cordwell J, Mander H, et al. Effects of cognitive behaviour therapy for worry on persecutory delusions in patients with psychosis (WIT):a parallel, single-blind, randomised controlled trial with a mediation analysis.Lancet Psychiatry. 2015; [Epub ahead of print]. doi: http://dx.doi.org/10.1016/S2215-0366(15)00039-5
121. Sheaves B, Onwumere J, Keen N, Stahl D, Kuipers E. Nightmares in patients with psychosis: the relationship with sleep, psychotic, affective and cognitive symptoms.Can J Psychiatry. 2014. (In Press)
122. Freeman D, Brugha T, Meltzer H, Jenkins R, Stahl D,Bebbington P.Persecutory ideation and insomnia: findings from the second British National Survey of Psychiatric Morbidity.J Psychiatr Res. 2010; 44: 1021-1026. doi: http://dx.doi.org/10.1016/j.jpsychires.2010.03.018
123. Smith MT, Perlis ML, Park A, Smith MS, Pennington J, Giles DE, et al. Comparative meta-analysis of pharmacotherapy and behavior therapy for persistent insomnia.Am J Psychiatry. 2002; 159(1): 5-11. doi: http://dx.doi.org/10.1176/appi.ajp.159.1.5
124. Morin CM, Vallières A, Guay B, Ivers H, Savard J, Mérette C,et al. Cognitive behavioral therapy, singly and combined with medication, for persistent insomnia: a randomized controlled trial.JAMA. 2009; 301(19): 2005-2015. doi: http://dx.doi.org/10.1001/jama.2009.682
125. Myers E, Startup H, Freeman D. Cognitive behavioural treatment of insomnia in individuals with persistent persecutory delusions: a pilot trial.J Behav Ther Exp Psychiatry. 2011; 42: 330-336. doi: http://dx.doi.org/10.1016/j.jbtep.2011.02.004
126. Freeman D, Startup H, Myers E, Harvey A, Geddes J, Yu LM,et al. The effects of using cognitive behavioural therapy to improve sleep for patients with delusions and hallucinations(the BEST study): study protocol for a randomized controlled trial.Trials. 2013; 14: 214. doi: http://dx.doi.org/10.1186/1745-6215-14-214
127. Shakoor S, McGuire P, Cardno AG, Freeman D, Plomin R,Ronald A. A shared genetic propensity underlies experiences of bullying victimization in late childhood and self-rated paranoid thinking in adolescence.Schizophr Bull. 2014;41(3): pii: sbu142. doi: http://dx.doi.org/10.1093/schbul/sbu142
128. Van Winkel M, Peeters F, van Winkel R, Kenis G, Collip D, Geschwind N, et al. Impact of variation in the BDNF gene on social stress sensitivity and the buffering impact of positive emotions: replication and extension of a geneenvironment interaction.Eur Neuropsychopharmacol. 2014;24: 930-938. doi: http://dx.doi.org/10.1016/j.euroneuro.2014.02.005
129. Giusti-Rodríguez P, Sullivan PF. The genomics of schizophrenia: update and implications.J Clin Invest. 2013;123(11): 4557-4563. doi: http://dx.doi.org/10.1172/JCI66031
, 2015-02-01; accepted, 2015-02-23)

Professor Paul Bebbington was born in Scotland and lives in South London. He was educated at Cambridge University where he obtained a First Class Honours (BA) in the Natural Sciences with a Part 2 in psychology and athletics Blue. He undertook clinical training at St Bartholomew’s Hospital in London. He was trained in psychiatry at the Maudsley Hospital and at the Institute of Psychiatry. For nearly 20 years he worked in the Medical Research Council Social Psychiatry Unit at the Institute of Psychiatry, initially under John Wing, and eventually becoming Assistant Director. In 1996, he moved to University College London (UCL) to a Chair in Social & Community Psychiatry. At the same time, he also took up an honorary consultant post with the Camden & Islington National Health Service Trust,working in a series of clinical appointments. The last of these was with the Community Mental Health Inreach Team in Holloway women’s prison, over the six years until September 2010. He was Head of the Department of Mental Health Sciences at UCL from 2004 until November 2009. He became Professor Emeritus at UCL in October 2010 on his retirement.
解密精神病:社会心理流行病学、发病机制和疾病意义
Bebbington P
流行病学;社会因素;精神病;认知行为治疗
Summary:This paper reviews a revolution in our understanding of psychosis over the last 20 years. To a major extent, this has resulted from a process of cross-fertilization between psychosocial epidemiology and cognitive behavior therapy for psychosis (CBT-p). This encouraged complementary strategies for the acquisition and analysis of data. These include the use of a range of dependent variables related to psychosis,and the exploitation of data from cross-sectional and longitudinal epidemiological surveys, virtual reality experiments, experience sampling methodology, and treatment trials. The key element is to investigate social and psychological measures in relation to each other. This research has confirmed the role of the external social world in the development and persistence of psychotic disorder. In addition, several psychological drivers of psychotic experiences have been identified. There is now persuasive evidence that the influence of social factors in psychosis is significantly mediated by non-psychotic symptoms, particularly mood symptoms and other attributes of affect such as insomnia. Psychotic symptoms are also driven by reasoning biases such as jumping to conclusions and belief inflexibility, though little is known about social influences on such biases. It is now clear that there are many routes to psychosis and that it takes many forms.Treatment of all kinds should take account of this: the dependence of CBT-p on a detailed initial formulation in terms of psychological processes and social influences is an example of the required flexibility. Individual mediators are now being targeted in specific forms of CBT-p, with good effect. This in turn corroborates the hypothesized role of non-psychotic symptoms in mediation, and attests to the power of the approaches described.
[Shanghai Arch Psychiatry. 2015; 27(2): 70-81. Epub 2015 Apr 2.
http://dx.doi.org/10.11919/j.issn.1002-0829.215027]
Division of Psychiatry, Faculty of Brain Sciences, University College London, United Kingdom
correspondence: p.bebbington@ucl.ac.uk
概述:本文回顾了过去20年我们对精神病认识的革命性变化。很大程度上说,这一变化主要得益于社会心理流行病学与针对精神病的认知行为治疗(cognitive behavior therapy for psychosis,CBT-p)的发展和交互促进。而后者也促进了数据的采集和分析方法的补充策略。这些方法包括利用与精神病相关的一系列因变量,如何分析横断面和纵向流行病学调查、虚拟现实研究、经验抽样方法研究及治疗学临床试验中采集到的数据。研究的关键是探索各个社会心理因素的相互关系和作用。这些研究证明了外部社会在精神病性障碍的发生和发展中的作用。此外,一些产生精神病性体验的心理驱动因素也被发现。现已有可靠证据表明,社会因素明显受到非精神病性症状的影响,尤其情绪症状及其他对情感有影响的症状,如失眠。精神病性症状也可以受到归因偏移的影响,如武断下结论、顽固的信念等,但是社会因素对此如何起作用仍所知甚少。现在可以明确的是精神病的成因各异,表现形式多样。对各种类型的治疗都应考虑以下这点:应根据心理过程和社会因素影响在原始的CBT-p方案上进行相应的调整。目前某些特定形式的CBT-p将个体调节因素作为治疗目标并取得良好的效果。这反过来证实了非精神病性症状的调节作用,并证明了所描述方法的有效性。
本文全文中文版从2015年06月06日起在http://dx.doi.org/10.11919/j.issn.1002-0829.215027可供免费阅览下载
- 上海精神医学的其它文章
- The transdiagnostic dimension of psychosis: implications for psychiatric nosology and research
- Finding a solution to psychosis: the emergence of a new path
- Prenatal choline and the development of schizophrenia
- Efficacy and safety of the Chinese herbal medicine shuganjieyu with and without adjunctive repetitive transcranial magnetic stimulation (rTMS) for geriatric depression: a randomized controlled trial
- Gene-based and pathway-based genome-wide association study of alcohol dependence
- Are the revised diagnostic criteria for Alzheimer’s disease useful in low- and middle-income countries?