Effects of antiarrhythmic peptide 10 on acute ventricular arrhythmia
Bing Sun, Jin-Fa Jiang, Cui-Mei Zhao, Chao-Hui Hu
Department of Cardiology, Tongji University Affiliated Tongji Hospital, Shanghai 200065, China
Effects of antiarrhythmic peptide 10 on acute ventricular arrhythmia
Bing Sun, Jin-Fa Jiang, Cui-Mei Zhao, Chao-Hui Hu*
Department of Cardiology, Tongji University Affiliated Tongji Hospital, Shanghai 200065, China
ARTICLE INFO
Article history:
Received 15 December 2014
Received in revised form 20 January 2015
Accepted 15 February 2015
Available online 20 March 2015
Cx43
Objective: To observe the effects antiarrhythmic peptide 10 (AAP10) aon acute ventricular arrhythmia and the phosphorylation state of ischemic myocardium connexin. Methods: Acute total ischemia and partial ischemia models were established by ceasing perfusion and ligating the left anterior descending coronary artery in SD rats. The effects of AAP10 (1 mg/L) on the incidence rate of ischemia-induced ventricular arrhythmia were observed. The ischemic myocardium was sampled to detect total-Cx43 and NP-Cx43 by immunofluorescent staining and western blotting. the total-Cx43 expression was detected through image analysis system by semi-quantitative analysis. Results: AAP10 could significantly decrease the incidence of ischemia-induced ventricular tachycardia and ventricular fibrillation. During ischemic stage, total ischemia (TI) and AAP10 total ischemia (ATI) groups were compared with partial ischemia (PI) and AAP10 partial ischemia (API) groups. The rates of incidence for arrhythmia in the ATI and API groups (10% and 0%) were lower than those in the TI and PI groups (60% and 45%). The difference between the two groups was statistically significant (P=0.019, P=0.020). The semi-quantitative analysis results of the ischemic myocardium showed that the total-Cx43 protein expression distribution areas for TI, ATI, PI and API groups were significantly decreased compared with the control group. On the other hand, the NP-Cx43 distribution areas of TI, ATI, PI and API groups were significantly increased compared with the control group (P>0.05). AAP10 could increase the total-Cx43 expression in the ischemic area and decrease the NP-Cx43 expression. Western blot results were consistent with the results of immunofluorescence staining. Conclusions: AAP10 can significantly decrease the rate of incidence of acute ischemia-induced ventricular tachycardia and ventricular fibrillation. Acute ischemic ventricular arrhythmias may have a relationship with the decreased phosphorylation of Cx43 induced by ischemia. AAP10 may stimulate the phosphorylation of Cx43 by increasing the total-Cx43 expression and decreasing the NP-Cx43 expression in the ischemic area, so as to decrease ventricular arrhythmia.
1. Introduction
The gap junction (GJ), which is located between myocardial cells, provides a direct communication pathway between ions and small molecular substances, to mediate intercellular communication. As the neighboring cells uncouple, the connecting channel of the gap closes, and subsequently induce slow and heteroplasmic electrical conductions that easily promote arrhythmia[1]. Cx43 is a major ventricular GJ protein, and its functional status is regulated based on the state of phosphorylation. Previous studies showed that Cx43 dephosphorylation may have an active role during the GJ channel closing process[2-5].
Antiarrhythmic peptide (AAP)[3] was named from its potent antiarrhythmic effects. In the AAP family, AAP10 has the same pharmacological effect[4]. Stains et al[5] considered the eliciting anti-arrhythmic effects of AAP10 through enhancing electrical conduction between the GJ. However, there was no uniformconclusion pertaining to the mechanisms involved in enhancing electrical conduction. Li et al[6] speculated that AAP10 may have some protective effect on the Cx43 expression. AAP10 can reduce the rate of incidence of arrhythmia through adjusting the P-Cx43 concentration. However, this viewpoint still falls short of sufficient experimental validation. To further explore the effects of AAP10 on acute ventricular arrhythmia, the author and his team established isolated acute cardiac ischemia SD rat models, and explored the possible mechanisms of the antiarrhythmic effects of AAP10 on acute ventricular arrhythmia from the Cx43 phosphorylation perspective.
2. Materials and methods
2.1. Experimental animals and equipment
A total of 60 SD rats, half male and half female, were provided by the Experimental Animal Center of Shanghai Traditional Chinese Medicine University, weighing (300±50) g. The rats were initially anesthetized with 3% sodium pentobarbital 30 mg/kg (US Biotopped Co.), and treated with 250 μ/kg heparin (Shanghai Fudan Fuhua Pharmaceutical Co., Ltd.), as an anticoagulant. After anesthesia, the costal margin of the abdominal wall below the xiphoid process was explored, and the diaphragm was cut open. The chest wall was cut along the anterior axillary line, turning up to the side of the head. Three branches of the aortic arch were clamped by micro surgery forceps. The aorta (retaining 3-4 mm from the root of heart), pulmonary artery, pulmonary vein, and inferior vena cava were rapidly interrupted. After exposure of the aortic arch, the complete heart was cut along the aortic stump, which was cut below aortic arch. The heart was cut off and was placed into an ice-cold Kreb-Henseleit (K-H) solution (4 ℃); residual blood was gently washed away. The edges of the ascending aorta were clamped with two micro-surgical forceps. The filling canals of the aorta were inserted, fixed by an artery clamp, and the Langendorff perfusion device (AD Instruments Pty Ltd, Australia) was rapidly connected, and fixed by line 0. It was then perfused with a modified K-H buffer, and saturated with 95% O2and 5% CO2. The perfusion fluid temperature was kept at 37 ℃ with a PH value of 7.4. During the experiment, the perfusion pressure was kept at 80-100 cmH2O and the perfusion flow was 8-10 mL/min. After the heart perfusion model was successfully established, the isolated heart started to re-beat within seconds. When the heart re-started and cardiac functions became stable, a pressure-measuring catheter balloon was inserted into the left ventricle through the mitral valve, and the other end of the pressuremeasuring catheter was connected to Multi physiological recorder through pressure sensor.
A 0.3 mm diameter silver wire was used as a pair of electrodes to record the epicardial electrical diagram; the lead wire was connected to the physiological recorder (Shanghai Alcott Biotechnology Co., Ltd.). One of the electrodes was fixed at the right ventricular free wall, the another electrode was fixed at the left ventricular free wall[6].
The ischemia animal model was established by ligating the left anterior descending artery (LAD). Between the left atrial appendage and arterial cone, a wire was used to bypass the LAD; both ends of wire were passed through a hollow plastic tube, which was ligated on another short rubber hose. Myocardial ischemia was induced, and it was observed for 30 minutes.
2.2. Experimental scheme
2.2.1. Grouping and establishment of ischemia-reperfusion model
Rats in control group (Control) and total ischemia group (TI) received isolated heart infusion for 30 minutes, then perfusion was stopped for 30 min. Rats in partial ischemia group (PI) received isolated heart infused for 30 minutes, then regional ischemia was induced by ligating LAD for 30 minutes. After 15 minutes of pretreatment, rats in AAP10 total ischemia (ATI) group were treated with perfusion fluid containing 1 mg/L concentration of AAP10 for another 15 minutes, and perfusion was stopped for 30 minutes. Rats in AAP10 partial ischemia (API) group were treated with perfusion fluid containing 1 mg/L AAP10 concentration for another 15 minutes, then regional ischemia was induced by ligating LAD for 30 minutes.
After pretreatment, the heart was isolated in a K-H solution for 15 minutes; and the stability of the cardiac functions was measured. Time was set to 0 min at the beginning of the experiment. The heart was treated with different perfusion fluids, according to the different groups; then perfusion was stopped to induce total heart ischemia or ligated LAD to induce a partial ischemia (except the control group) for 30 minutes. The experiment was stopped when there was continuous ventricular tachycardia (>1 min) or ventricular fibrillation. The control group did not receive any intervention, and the other processes were the same as above.
2.2.2. Detection of the protein expression
After perfusion in the partial ischemia group, the Evans blue dye test was carried out. The aizen area represented the non-ischemic area, and the undyed area represented the ischemic area. TTC stain was carried out to the cardiac muscle at the undyed area; the red area represented the ischemic area, and the unstained area represented the infarct area. Myocardial ischemia was detected by immunofluorescence staining and analyzed by a laser scanning confocal microscope. The hearts from the control group were directly detected by the above method at the LAD perfusion area.
Western blot detection was also carried out on the myocardial of the groups at the same time. A total of 100 mg of myocardialtissues were obtained from each group. After cryogenic grinding with liquid nitrogen, 1 mL RIPA Lysis buffer (NanJing SunShine Biotechnology Co., LTD) was added for tissue lysis. Protein was obtained, after 2 minutes of high speed centrifugation at 12 000 g. A small amount of supernatant was used for quantitative measurement. The protein samples were adjusted to equal the concentrations. After polyacrylamide gel electrophoresis, the membrane was transferred and prepared for blocking. Primary antibodies were added and washed; secondary antibodies were added and washed again. Scan and analysis was carried out after luminescence identification.
2.3. Statistical analysis
All data were analyzed by SSPS19.0 statistics software, and the data were expressed as mean±SD values. t-test was applied in comparing the two groups. χ2test was used to count the data; P<0.05 was considered as significant difference.
3. Results
3.1. Results of the Langendorff isolated perfused SD rat models
The number of cases that occurred during the ischemic period, as well as the number of ventricular tachycardia and ventricular fibrillation cases for each group is shown in Table 1. During the ischemic stage, the rate of incidence for arrhythmia in the ATI and API groups (10% and 0%) were lower than the TI and PI groups (60% and 45%). The difference was statistically significant between the two groups (P = 0.019, P = 0.020).
3.2. Protein expression results
he relative gray values of the total-Cx43 protein bands for the TI and PI groups were lower than the control group. The relative gray values of the total-Cx43 protein bands for the ATI and API groups were lower than the TI and PI groups. The relative gray values of the NP-Cx43 protein bands for the TI and PI groups were higher than the control group. The relative gray values of the NP-Cx43 protein bands for the ATI and API groups were lower than the TI and PI groups. All of the differences were statistically significant (P<0.05) (Figure 1).

Table 1 Effects of AAP10 on the number of ventricular tachycardia and ventricular fibrillation cases.
In the TI and PI groups, total-Cx43 was decreased in number, but NP-Cx43 was increased in number. For the ATI and API groups, the fluorescence signal intensity of total-Cx43 was stronger than the TI and PI groups, while the signal intensity of NP-Cx43 was lower than the TI and PI groups (Figure 2). The semi-quantitative analysis results of Cx43 are shown in Table 2.
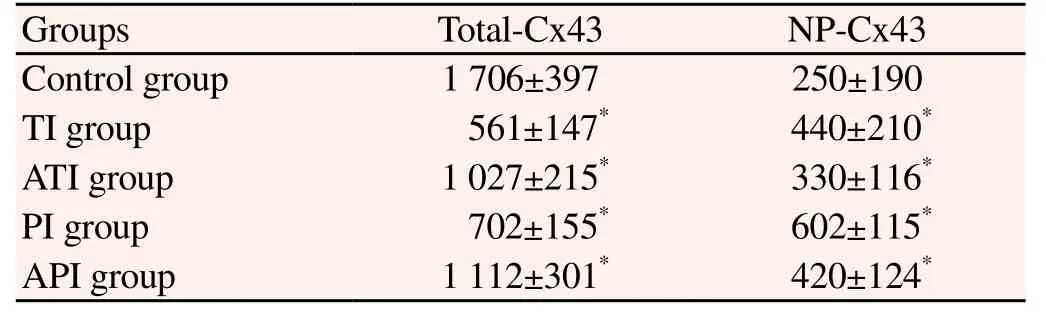
Table 2 Cx43 semi-quantitative analysis results (μm2).
Compared with the control group, the number of total-Cx43 in the TI, ATI, PI and API groups was significantly decreased; while the number of NP-Cx43 was significantly increased. Both of the differences were statistically significant (P<0.05). This suggests that GJ functions was reduced with the decrease of P-Cx43, which may induce ischemic ventricular arrhythmias. AAP10 could partially reverse the extent of total-Cx43 reduction and reduce the number of NP-Cx43, thus, maintain the quantity of P-Cx43 protection and improve the GJ function, which may reduce ischemic ventricular arrhythmias.
4. Discussion
AAP obviously has an anti-arrhythmic effect; but its specific effects and mechanisms are still unclear. GJ play an important role in maintaining normal heart rhythm and in the material exchange process between cells[7-14]. This study applied isolated perfusion experiments to explore the effects of AAP10 on acute ventricular arrhythmia, and the relationship of AAP10 with the Cx-43 protein of the GJ. This research clearly shows the mechanism of AAP10 and provides new ideas for the prevention and treatment of ventricular arrhythmia.
4.1. Effect of AAP10 on ischemic arrhythmias
In this study, the rate of incidence of ventricular arrhythmias occurred to nearly half of the 21 animals for the TI and PI groups, and occurred only once among 19 animals for the ATI and API groups. These results suggest that AAP10 can significantly decrease the incidence rate of acute ischemia-induced ventricular tachycardia and ventricular fibrillation; AAP10 can increase the expression of total-Cx43 and decrease the expression of NP-Cx43, specifically increasing the quantity of functional P-Cx43. This effect may improve and restore the consistency of electrical conductions between cells; which could be good for breaking the reentrant loop and suppressing the occurrence of ventricular fibrillation and ventricular tachycardia[15].
4.2. Relationship of Cx43 and arrhythmia
From the results of this study, Cx43 phosphorylation and Cx43 dephosphorylation were both found on normal myocardial cellular surfaces. The ischemic results of the Western blot and immunofluorescence staining tests revealed a decrease in total-Cx43 and an increase in NP-Cx43 quantities; these results mean that the functional P-Cx43 levels also decreased, which were related to previous studies[15,16]. Last 2000, Verrier et al[16] found that P-Cx43 levels decreased and NP-CX43 levels increased due to ischemia aggravation in the acute ischemic myocardial tissues. In this experiment, either total heart ischemia or partial ischemia can increase the occurrence of ventricular fibrillation and ventricular tachycardia. This suggests that due to the probable decrease of P-Cx43, the GJ function was reduced in acute myocardial ischemia; which slowed down the electrical conduction speed of myocardial cells, thus, forming a material foundation for reentrant arrhythmia; and malignant arrhythmia, such as ventricular tachycardia and ventricular fibrillation, were prone to accrue. Some studies showed that inhibiting GJ functions have some effect on arrhythmias[17-19]. The experimental results revealed that total-Cx43 in the ischemic myocardium significantly reduced, compared to that of the normal myocardium, which suggests that myocardial ischemia damagedthe existing GJs. There are several possible mechanisms involved in this process, such as intracellular accumulation of acidic substances, large generation of oxygen free radicals, gathering of lipid metabolites, etc. The decreased Cx43 phosphorylation level and myocardial ischemia can cause intracellular ATP hydrolysis; wherein, the number of ATP cases dropped significantly, leading to connexin dephosphorylation. The reduced total-Cx43 and phosphorylation levels are signs of myocardial injury and protective responses of the heart. Studies have reported that in myocardial necrosis, harmful substances can pass through the GJs between the cells and expand the ischemic necrosis area[20,21]. The decreased values and functions of GJs is a self-limiting response, when damage increases up to a certain extent[22,23].
4.3. Deficiency and prospect of this paper
Although the result of the experiment was satisfactory, there are still some shortcomings in the experimental process: first of all, the sample size was small. With limited funds and more groupings, the sample size in each group became smaller. Excluding ligation failure, 10 out of 12 cases were effective in each group. A small sample size may cause bigger errors, therefore, the results obtained from this study does not have enough representation. In future experiments, we should enlarge the sample size, as well as increase the number of groups and the sample size in each group, in order to achieve a more objective and accurate result. Secondly, this study explored the antiarrhythmic mechanisms of AAP10 in acute ischemia from the Cx43 phosphorylation perspective, but no further study was done on the mechanisms that pertain to the regulation of AAP10 in Cx43 phosphorylation. Existing experimental results have confirmed that there is a connection between AAP10 and Cx43, therefore, the interaction mechanism between them deserves careful study. In the future, additional studies can be carried out to explore the relative mechanisms between these, and provide new ideas for developing new anti-arrhythmic drugs.
4.4. Conclusion
In summary, AAP10 can significantly decrease the rate of incidence of acute ischemia-induced ventricular tachycardia and ventricular fibrillation. In acute myocardial ischemia, myocardial cell intercellular communication slows down based on the decreased quantity of total-Cx43 and the changes on the state of phosphorylation. AAP10 may play its role by promoting Cx43 phosphorylation and increasing the quantity of total-Cx43. However, the specific regulating mechanism of GJ phosphorylation is still not that clear, and needs to be further explored.
Conflict of interest statement
We declare that we have no conflict of interest.
[1] O’Quinn MP, Palatinus JA, Harris BS, Hewett KW, Gourdie RG. A peptide mimetic of the connexin43 carboxyl terminus reduces gap junction remodeling and induced arrhythmia following ventricular injury. Circ Res 2011; 108(6): 704-715.
[2] Sánchez JA, Rodríguez-Sinovas A, Barba I, Miró-Casas E, Fernández-Sanz C, Ruiz-Meana M, et al. Activation of RISK and SAFE pathways is not involved in the effects of Cx43 deficiency on tolerance to ischemia–reperfusion injury and preconditioning protection. Basic Res Cardiol 2013; 108(3): 1-13.
[3] Phé V, Behr-Roussel D, Oger-Roussel S, Rouprêt M, Chartier-Kastler E, Lebret T, et al. Involvement of connexins 43 and 45 in functional mechanism of human detrusor overactivity in neurogenic bladder. Urology 2013; 81(5): 1108. e1-1108. e6.
[4] Yuan MJ, Huang H, Tang YH, Wu G, Gu YW, Chen YJ, et al. Effects of ghrelin on Cx43 regulation and electrical remodeling after myocardial infarction in rats. Peptides 2011; 32(11): 2357-2361.
[5] Stains JP, Watkins MP, Grimston SK, Hebert C, Civitelli R. Molecular mechanisms of osteoblast/osteocyte regulation by connexin43. Calcified Tissue Int 2014; 94(1): 55-67.
[6] Li J, Goossens S, van Hengel J, Gao E, Cheng L, Tyberghein K. Loss of αT-catenin alters the hybrid adhering junctions in the heart and leads to dilated cardiomyopathy and ventricular arrhythmia following acute ischemia. J Cell Sci 2012; 125(4): 1058-1067.
[7] Laird DW. Syndromic and non-syndromic disease-linked Cx43 mutations. Febs Lett 2014; 588(8): 1339-1348.
[8] Wang D, Zhang F, Shen W, Chen M, Yang B, Zhang Y, et al. Mesenchymal stem cell injection ameliorates the inducibility of ventricular arrhythmias after myocardial infarction in rats. Int J Cardiol 2011; 152(3): 314-320.
[9] Ryzhak AP, Kuznik BI , Rutkovskaya VN, Ryzhak GA, Titkov IS. Antiarrhythmic action of natural peptide geroprotector. Adv Gerontol 2013; 3(1): 67-69.
[10] Kylmäoja E, Kokkonen H, Kauppinen K, Hussar P, Sato T, Haugan K, et al. Osteoclastogenesis is influenced by modulation of gap junctional communication with antiarrhythmic peptides. Calcified Tissue Int 2013; 92(3): 270-281.
[11] Skyschally A, Walter B, Hansen RS, Heusch G. The antiarrhythmic dipeptide ZP1609 (danegaptide) when given at reperfusion reduces myocardial infarct size in pigs. N-S Arch Pharmacol 2013; 386(5): 383-391. [12] Wang DG, Zhang FX, Chen ML, Zhu HJ, Yang B, Cao KJ. Cx43 in mesenchymal stem cells promotes angiogenesis of the infarcted heart independent of gap junctions. Mol Med Rep 2014; 9(4): 1095-1102.
[13] Ravens U, Poulet C, Wettwer E, Knaut M. Atrial selectivity of antiarrhythmic drugs. J Physiol 2013; 591(17): 4087-4097.
[14] Solan JL, Lampe PD. Specific Cx43 phosphorylation events regulate gap junction turnover in vivo. Febs Lett 2014; 588(8): 1423-1429.
[15] Linz D, Wirth K, Ukena C, Mahfoud F, Pöss J, Linz B, et al. Renal denervation suppresses ventricular arrhythmias during acute ventricular ischemia in pigs. Heart Rhythm 2013; 10(10): 1525-1530.
[16] Verrier RL, Pagotto VPF, Kanas AF, Sobrado MF, Nearing BD, Zeng D, et al. Low doses of ranolazine and dronedarone in combination exert potent protection against atrial fibrillation and vulnerability to ventricular arrhythmias during acute myocardial ischemia. Heart Rhythm 2013; 10(1): 121-127.
[17] Nikolaidou B, Lazaridis A, Doumas M. Antihypertensive therapy after acute ischemic stroke. Jama 2014; 311(22): 2333-2334.
[18] Liang JJ, Prasad A, Cha YM. Temporal evolution and implications of ventricular arrhythmias associated with acute myocardial infarction. Cardiol Rev 2013; 21(6): 289-294.
[19] Williams ES, Viswanathan MN. Current and emerging antiarrhythmic drug therapy for ventricular tachycardia. Cardiol Ther 2013; 2(1): 27-46.
[20] Winkler C, Funk M, Schindler DM, Hemsey JZ, Lampert R, Drew BJ. Arrhythmias in patients with acute coronary syndrome in the first 24 hours of hospitalization. Heart & Lung: J Acute Critical Care 2013; 42(6): 422-427.
[21] Yasukawa H, Oba T, Fukumoto Y. Alterations in coxsackievirus and adenovirus receptor confer susceptibility to ventricular arrhythmia with an ischemic event. J Am Coll Cardiol 2014; 63(6): 560-562.
ent heading
10.1016/S1995-7645(14)60321-7
*Corresponding author: Chao-Hui Hu, MD, Associate Chief Physician, Department of Cardiology, Tongji University Affiliated Tongji Hospital, No. 389, Xincun Road, Putuo District, Shanghai 200065, China.
Tel: 86+21-66112819
E-mail: huchaohui3486@126.com
Foundation project: This project was supported by the National Natural Science Foundation of China (No: 81300150).
Ventricular arrhythmia
Acute myocardial ischemia
 Asian Pacific Journal of Tropical Medicine2015年3期
Asian Pacific Journal of Tropical Medicine2015年3期
- Asian Pacific Journal of Tropical Medicine的其它文章
- Afebrile presentation of 2014 Western Africa Ebolavirus infection: the thing that should not be forgotten
- Dengue in pregnancy: an under-reported illness, with special reference to other existing co-infections
- Relevance of EGFR gene mutation with pathological features and prognosis in patients with non-small-cell lung carcinoma
- Influence of artificial luminous environment and TCM intervention on development of myopia rabbits
- MicroRNA-126 inhibits the proliferation of lung cancer cell line A549
- Expression and significance of netrin-1 and its receptor UNC5C in precocious puberty female rat hypothalamus
