Effect of complex reinforcing-reducing manipulation on lower limb motion and balance disorder in patients with subacute combined degeneration of the spinal cord
Zhang Chao-hong (张朝红), Li Qi (李旗)
1 Rehabilitation Department, the 2nd Hospital Affiliated to Luohe Medical College, Henan 462300, China
2 College of Traditional Chinese Medicine, Hebei United University, Hebei 063000, China
Effect of complex reinforcing-reducing manipulation on lower limb motion and balance disorder in patients with subacute combined degeneration of the spinal cord
Zhang Chao-hong (张朝红)1, Li Qi (李旗)2
1 Rehabilitation Department, the 2nd Hospital Affiliated to Luohe Medical College, Henan 462300, China
2 College of Traditional Chinese Medicine, Hebei United University, Hebei 063000, China
Objective:To observe the effect of complex reinforcing [Shao Shan Huo(Mountain-burning Fire)] and reducing [Tou Tian Liang(Heaven-penetrating Cooling)] manipulations on motion and balance of the lower limbs in patients with subacute combined degeneration of the spinal cord (SCD).
Acupuncture Therapy; Method of Reinforcing-reducing;Shao Shan Huo(Mountain-burning Fire);Tou Tian Liang(Heaven-penetrating Cooling); Vitamin B12Deficiency
Subacute combined degeneration of spinal cord (SCD) refers to degeneration of the posterior and lateral columns of the spinal cord as well as peripheral nerve system damage as a result of vitamin B12deficiency. This condition is clinically characterized by parasthesias, sensory ataxia and spastic paraplegia[1-2]. SCD patients often have severe sequelae of motor and balance disorders of the lower limbs[3], which may greatly affect the patients’ quality of life. To explore the effective treatment protocol for SCD-induced motor and balancedisorders of the lower limbs, we’ve observed the effect of complex reinforcing [Shao Shan Huo(Mountainburning Fire)] and reducing [Tou Tian Liang(Heavenpenetrating Cooling)] manipulations. The results are now summarized as follows.
1 Clinical Materials
1.1 Diagnostic criteria
This was based on the diagnostic criteria for SCD in theNeurology[4]: onset in midlife; signs and symptoms of degenerated posterior and lateral columns of the spinal cord and nerve system damage; presence of antihistamine-related achlorhydria, megaloblastic anemia and low contents of serum B12.
In Chinese medicine, this condition was diagnosed as a Wei-flaccidity syndrome[5]: weakness or flaccidity of the limbs; muscle atrophy or paralysis in severe cases.
1.2 Inclusion criteria
Those who met the above diagnostic criteria; aged between 40 and 70 years with no gender differences; having duration lasting from 2 weeks to 6 months.
1.3 Exclusion and rejection criteria
Those who didn’t meet the above diagnostic or inclusion criteria; lower limb dysfunctions due to other medical conditions; and those who dropped out during the treatment.
1.4 Statistical method
The SPSS 17.0 version software was used for statistical analysis. Thet-test was used for inter-group comparison, which was expressed in the form of mean ± standard deviationThe Chi-square test was used for rate comparison. APvalue of less than 0.05 indicates a statistical difference.
1.5 General data
A total of 60 eligible cases treated in the Rehabilitation Department, 2nd Hospital Affiliated to Luohe Medical College between January 2012 and August 2014 were recruited in this study. They were randomly allocated into an observation group and a control group by the visit sequences, 30 in each group. There were no between-group statistical differences in baseline data (P>0.05), indicating that the two groups were comparable (Table 1).

Table 1. Between-group comparison of baseline data
2 Treatment Methods
2.1 Observation group
2.1.1 Basic Western medical treatment
Mecobalamin Injection (500 µg/mL, manufactured by Eisai China Inc.) was adopted for intravenous dripping, 2 000 for each dose, once a day. In addition, patients took Folic Acid (Tianjin Lisheng Pharmaceutical Co., Ltd.) orally, 10 mg for each dose, 3 times a day for 2 months[6].
2.1.2 Acupuncture therapy
Points: First group [Zuwuli (LR 10), Jimen (SP11), Xuehai (SP 10), Yinlingquan (SP 9), Diji (SP 8), Lougu (SP 7) and Sanyinjiao (SP 6)]. Second group [Biguan (ST 31), Yinshi (ST 33), Liangqiu (ST 34), Zusanli (ST 36), Shangjuxu (ST 37), Xiajuxu (ST 39) and Fenglong(ST 40)].
Method: Disposable needles of 0.35 mm in diameters and 40 mm in length were used. After routine sterilization, the abovementioned points were punctured perpendicularly. TheTou Tian Liang(Heaven-penetrating Cooling) reducing manipulation was applied to points in the first group, whereasShaoShan Huo(Mountain-burning Fire) manipulation was applied to points in the second group. Needles were retained for 30 min, once a day, 15 d made up one treatment course. The patients were treated for 4 courses and there was a 1-day interval between two courses.
2.2 Control group
Patients in the control group only received the same basic Western medical treatment (drug, dose, administration and treatment course) as those in the observation group.
3 Outcome Observation
3.1 Evaluation parameters
3.1.1 Joint range of motion, muscle force and muscle tone
The lower limb functions were assessed using the Lokomat system manufactured by Hocoma Medical Technology Company (Switzerland). The range of motion (L-ROM), muscle force (L-FORCE) and muscle tone (L-STIFF) were measured respectively[7].
3.1.2 The parameters of center of pressure (COP) shifting path
Before and after treatment, the B-PHY type balance function check training system was used to measure the patients’ COP path length, peripheral area, COP path length per unit area, left-right offset and rectangular area.
3.2 Therapeutic efficacy criteria[7]
Recovery: Almost full recovery of muscle force and parasthesia, coupled with almost normal walking.
Improvement: Improved muscle force and parasthesia, coupled with increased walking ability.
Failure: Signs and symptoms remained unchanged after treatment.
3.3 Results
3.3.1 Hip and knee joint ROM, muscle force and tone Before treatment, there were no between-group statistical differences in hip and knee joint ROM, muscle force and tone (P>0.05), indicating that the two groups were comparable. After treatment, the control group showed no intra-group statistical differences in the above parameters (P>0.05); however, the observation group showed intra-group statistical differences in the above parameters (P< 0.05); and there were between-group statistical differences in the above parameters (P<0.01), indicating a better improvement in hip/knee joint ROM, muscle force and tone than that in the control group (Table 2-Table 4).
Table 2. Between-group comparison of joint range of motion
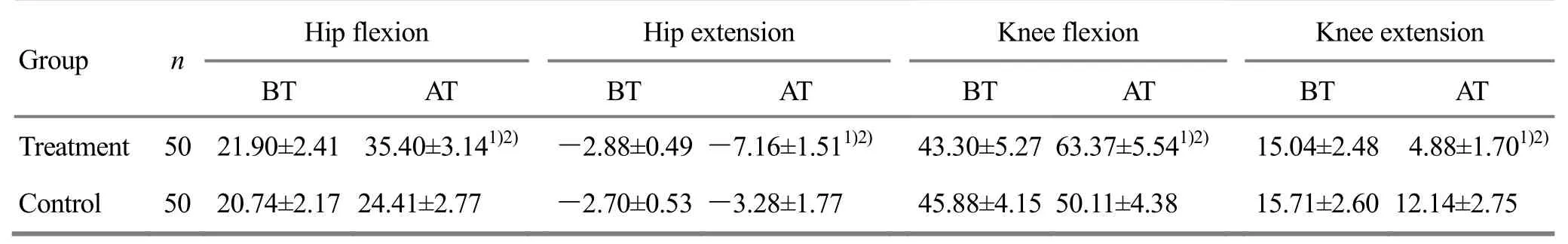
Table 2. Between-group comparison of joint range of motion
Note: BT=Before treatment; AT=After treatment; intra-group comparison before and after treatment, 1) P<0.05; compared with the control group after treatment, 2) P<0.05
Group n Hip flexion Hip extension Knee flexion Knee extension BT AT BT AT BT AT BT AT Treatment 50 21.90±2.41 35.40±3.141)2)-2.88±0.49-7.16±1.511)2) 43.30±5.27 63.37±5.541)2)15.04±2.48 4.88±1.701)2)Control 50 20.74±2.17 24.41±2.77 -2.70±0.53-3.28±1.77 45.88±4.15 50.11±4.38 15.71±2.60 12.14±2.75
Table 3. Between-group comparison of muscle force

Table 3. Between-group comparison of muscle force
Note: BT=Before treatment; AT=After treatment; Intra-group comparison before and after treatment, 1) P<0.05; compared with the control group after treatment, 2) P<0.05
Group n Hip flexion Hip extension Knee flexion Knee extension BT AT BT AT BT AT BT AT Treatment 50 26.27±3.10 42.65±6.301)2) 24.40±3.40 38.30±5.751)2) 28.37±2.03 50.27±4.771)2)30.17±2.74 50.68±7.931)2)Control 50 25.33±3.65 31.85±4.14 23.03±2.92 27.56±4.45 29.06±1.99 35.81±4.63 31.48±3.07 38.16±5.12
Table 4. Between-group comparison of muscle tone
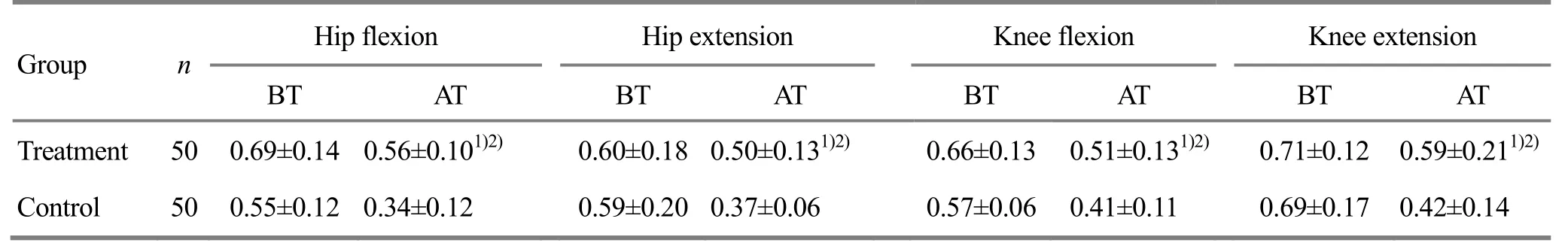
Table 4. Between-group comparison of muscle tone
Note: BT=Before treatment; AT=After treatment; Intra-group comparison before and after treatment, 1) P<0.05; compared with the control group after treatment, 2) P<0.05
Group n Hip flexion Hip extension Knee flexion Knee extension BT AT BT AT BT AT BT AT Treatment 50 0.69±0.14 0.56±0.101)2) 0.60±0.18 0.50±0.131)2) 0.66±0.13 0.51±0.131)2)0.71±0.12 0.59±0.211)2)Control 50 0.55±0.12 0.34±0.12 0.59±0.20 0.37±0.06 0.57±0.06 0.41±0.11 0.69±0.17 0.42±0.14
3.3.2 The COP shifting path
Before treatment, there were no between-group statistical differences in path length, path length per unit area and rectangular area (P>0.05), indicating that the two groups were comparable. After treatment, the above parameters were markedly improved in both groups (P<0.01), and there were between-group statistical differences (P<0.05), indicating a better balance function in the observation group than that in the control group (Table 5).
Table 5. Between-group comparison of COP shifting path parameters before and after treatment
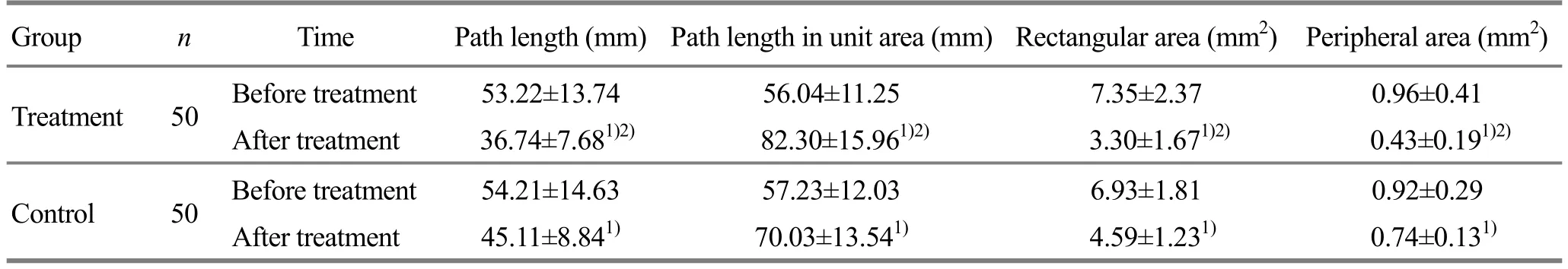
Table 5. Between-group comparison of COP shifting path parameters before and after treatment
Note: Intra-group comparison before and after treatment, 1) P<0.05; compared with the control group after treatment, 2) P<0.05
Group n Time Path length (mm)Path length in unit area (mm)Rectangular area (mm2) Peripheral area (mm2) Treatment 50 Before treatment 53.22±13.74 56.04±11.25 7.35±2.37 0.96±0.41 After treatment 36.74±7.681)2) 82.30±15.961)2) 3.30±1.671)2) 0.43±0.191)2)Control 50 Before treatment 54.21±14.63 57.23±12.03 6.93±1.81 0.92±0.29 After treatment 45.11±8.841) 70.03±13.541) 4.59±1.231) 0.74±0.131)
3.3.3 Between-group comparison of clinical effects
The total effective rate was 83.3% in the observation group, versus 60.0% in the control group, showing a statistical difference (P<0.05) and indicating a better effect in the observation group than that in the control group (Table 6).

Table 6. Between-group comparison of clinical effects (case)
4 Discussion
In remissive stage of subacute degeneration of the spinal cord, due to substantial decrease in muscle force of the affected limb, hypertonia, decrease in active control, diminished balancing, and abnormal motor pattern, patients often manifest balance disorders, unstable walking or inability to walk[8-10]. In addition, due to central nerve damage, loss of control over motor function, hyperreflexia, diminished or loss of muscle coordination and decreased balancing, patients fail to maintain normal postures and COP distribution and thus develop balance disorder[11-12]. Acupuncture has been proven to be effective for nervous system disorders. Research findings over the past decades have confirmed its scientific foundation[13-17]. The reinforcing [Shao Shan Huo (Mountain-burning Fire)] and reducing [Tou Tian Liang (Heaven-penetrating Cooling)] manipulations aim to balance yin and yang by reducing points of yin meridians (medial sides of the lower limbs) and reinforcing points of yang meridians (lateral sides of the lower limbs). Furthermore, this can help to regulate the patients’ muscle force, tone and motor function.
This study employed complex reinforcing and reducing manipulation for affected limbs in SCD patients and observed the patients’ lower limb motor and balance function using the Lokomat lower limb function assessment system and B-BHY type balance function check training system. After treatment, the ROM of hip/knee joints in the treatment group was increased, the muscle forces of hip/knee flexor and extensor were improved and the muscle tones were decreased, showing better effects when compared with that in the control group. The balancing parameters were more significantly improved in the observation group than that in the control group. Consequently, the reinforcing [Shao Shan Huo (Mountain-burning Fire)] and reducing [Heaven-penetrating Cooling)] manipulations can effectively increase the hip/knee joint ROM, increase the muscle force, decrease the muscle tone and substantially improve the balance function.
Thanks to the use of Lokomat gait training and analysis system, this study has enabled gait analysis to be more objective, accurate and reliable, allowing doctors to target specific gait problems, adjust treatment protocol and further improve the patients’walking ability. In the meantime, this system has also laid theoretical foundation for standardized rehabilitation therapy for gait abnormality.
Conflict of Interest
The authors declared that there was no conflict of interest in this article.
Acknowledgments
This work was supported by Scientific Research Project of Hebei Provincial Administration Bureau of Traditional Chinese Medicine (河北省中医药管理局科研计划项目, No. 2014188); Hebei Tangshan Science and Technology Project (河北省唐山市科技计划项目, No.121302118b).
Statement of Informed Consent
Informed consent was obtained from all individual participants included in this study.
Received: 20 November 2014/Accepted: 28 December 2014
[1] Zhang LR, Chen H, Sun L, Dong YX, Zhao DX, Xiao ZG. Therapeutic observation on treatment of subacute combined degeneration of spinal cord by acupuncture plus medication and rehabilitation. Shanghai Zhenjiu Zazhi, 2013, 32(1): 15-16.
[2] Zuo SM, Zhang WH. A case report on allergic reaction to filiform needles and atypical subacute combined degeneration of the spinal cord. Jiangxi Zhongiyao, 2013, 44(8): 50-51.
[3] Guo XL, Huang XS, Liu SX, Chen ZH. A study of clinical electrophysiological and neuropathological characteristics of subacute combined degeneration of the spinal cord. Chin J Neuroimmunol & Neurol, 2011, 18(2): 83-86.
[4] Wang WZ. Neurology. Beijing: People’s Medical Publishing House, 2004: 142-143.
[5] State Administration of Traditional Chinese Medicine. Criteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine. Nanjing: Nanjing University Press, 1994: 23-24.
[6] Zhu XY, Li J, Dong ZX, Huang GX, Zhou Y. Clinical, magnetic resonance imaging and electrophysiological analysis with high-dose Mecobalamine therapy for subacute combined degeneration. Zhongguo Linchuang Shenjing Kexue, 2009, 17(3): 267-271.
[7] Li Q, Tian FL, Liu GR, Zheng DS, Chen JM, Ma SX, Cui JM, Wang HB, Li XQ. Therapeutic effect of yin-yang meridian acupuncture by reinforcing-reducing with patient’s respiration on low limb function in patients after stroke. Xiandai Yufang Yixue, 2014, 41(15): 2869-2871.
[8] Tian FL, Li Q, Liu GR, Zheng DS, Chen JM, Ma SX, Cui JM, Wang HB, Li XQ. Reinforcing and reducing manipulation by breathing on yin and yang meridian points for motor function of knee joints in patients with ischemic stroke. J Acupunct Tuina Sci, 2014, 12(5): 282-285.
[9] Smith PS, Thompson M. Treadmill training post stroke: are there any secondary benefits? A pilot study. Clin Rehabil, 2008, 22(10-11): 997-1002.
[10] Mao HF, Hsueh IP, Tang PF, Sheu CF, Hsieh CL. Analysis and comparison of the psychometric of three balance measures for stroke patients. Stroke, 2002, 33(4): 1022-1027.
[11] Gu X, Patricia ES. Relationship among walking speed, balance and lower extremity recovery of hemiplegic patients. Zhonghua Wuli Yixue Zazhi, 1998, 20(4): 199-201.
[12] Huang XJ, Dou ZL, Qiu WH, Fu Y, Liao D. Effects of dynamic postural balance training on balance function of hemiplegic stroke patients. Zhongguo Kangfu Yixue Zazhi, 2011, 26(11): 1029-1032.
[13] Li ZR. Experimental Acupuncture Science. Beijing: China Press of Traditional Chinese Medicine, 2003: 3-4.
[14] Liu M. Electroacupuncture increased the muscle force of hemiplegic limb in 40 cases. Henan Zhongyi, 2003, 23(1): 56-57.
[15] Li CF, Jia CS, Li XF, Shi J, Dou ZZ, Sun P. Effect of penetrative needling of otopoints combined with body acupuncture on limb myodynamia and neurofunction in patients with acute cerebral infarction. Zhen Ci Yan Jiu, 2010, 35(1): 56-60.
[16] Li PF, Qi HP, Dong Y, Zhang YG, Wang Y, Pu F, Sun PY, Wang T, Liu G. The clinical research of awn needle pricking antagonist muscle combination of muscle tension balanced PNF technique to treat post-stroke lower limb spastic paralysis. Zhenjiu Linchuang Zazhi, 2010, 26(3): 1-5.
[17] Jin Z, Li ZX, Wang YL, Wang LJ, Bao DP. Clinical observations on double-needle acupuncture for the treatment of post-stroke leg hypermyotonia. Shanghai Zhenjiu Zazhi, 2011, 30(2): 93-95.
Translator:Han Chou-ping (韩丑萍)
复式针刺补泻法对脊髓亚急性联合变性下肢运动和平衡功能的影响
目的:观察烧山火、透天凉复式针刺补泻法对脊髓亚急性联合变性下肢运动和平衡功能的影响。方法:将100例脊髓亚急性联合变性患者按就诊顺序随机分为观察组与对照组, 每组50例。观察组患者在西医治疗基础上予以针刺治疗, 采用烧山火、透天凉复式针刺补泻方法, 对照组患者仅予以与观察组相同的西医基础治疗。于治疗前、治疗2个月后, 对患者髋、膝关节肌力, 肌张力以及关节活动度进行运动学参数测定, 以及轨迹长、外周面积、单位面积轨迹长、矩形面积平衡功能参数测定。结果:治疗后, 两组患者的轨迹长、外周面积、单位面积轨迹长、左右偏移、矩形面积、稳定性系数、体重分布系数均较本组治疗前有明显改善(P<0.01); 两组髋、膝关节肌力, 肌张力以及关节活动度差异有统计学意义(P<0.01)。观察组总有效率为83.3%, 对照组为60.0%, 两组总有效率差异具有统计学意义(P<0.05)。结论:复式针刺补泻法能提高脊髓亚急性联合变性下肢运动和平衡功能。
针刺疗法; 针刺补泻; 烧山火; 透天凉; 维生素B12缺乏
R246.6 【
】A
Author: Zhang Chao-hong, vice chief physician.
E-mail: tsslw110@126.com
Methods:A total of 100 SCD cases were randomly allocated into an observation group and a control group by their visit sequence, 50 cases in each group. On the basis of Western medical treatment, cases in the observation group were also treated with acupuncture therapy plus complex reinforcing-reducing manipulation; whereas cases in the control group were only treated with the same Western medical treatment as those in the observation group. Before and 2 months after treatment, kinematic parameters including muscle force, muscle tone and range of motion of the hip and knee joints were measured. In addition, balancing parameters including the path length of center of pressure (COP), peripheral area, COP path length per unit area and rectangular area were also measured before and after treatment.
Results:After treatment, there were statistical intra-group differences in COP path length, peripheral area, COP path length per unit area, left-right offset, rectangular area, coefficient of stability and coefficient of weight distribution (P<0.01). There were statistical inter-group differences in muscle force, muscle tone and range of motion of hip and knee joints (P<0.01). The total effective rate was 83.3% in the observation group, versus 60.0% in the control group, showing a statistical difference (P<0.05).
Conclusion:Complex reinforcing-reducing manipulations can improve the lower limb motion and balance in SCD patients.
 Journal of Acupuncture and Tuina Science2015年3期
Journal of Acupuncture and Tuina Science2015年3期
- Journal of Acupuncture and Tuina Science的其它文章
- Efficacy observation on acupuncture-moxibustion for urinary retention after surgery for cervical cancer
- Therapeutic observation of acupuncture plus heat-sensitive moxibustion for chronic pelvic inflammatory disease
- A controlled study on treatment of acute lumbar sprain by acupuncture at Yaotongdian (EX-UE 7) plus tuina manipulation
- Clinical study on skin needling plus heat-sensitive moxibustion for chronic facial paralysis
- Effect of tuina manipulations on blood pressure and its variability in hypertension patients
- Clinical study on acupoint massage in improving cognitive function and sleep quality of elderly patients with hypertension
