Robotic distal ureterectomy with psoas hitch and ureteroneocystostomy:Surgical technique and outcomes
Joseph Pugh,Amy Farkas,Li-Ming Su*
Department of Urology,University of Florida,Gainesville,FL,USA
CASE REPORT
Robotic distal ureterectomy with psoas hitch and ureteroneocystostomy:Surgical technique and outcomes
Joseph Pugh,Amy Farkas,Li-Ming Su*
Department of Urology,University of Florida,Gainesville,FL,USA
Robotic distal
ureterectomy;
Psoas hitch;
Ureteroneo
cystostomy
Use of the da Vinci®surgical robotic system has expanded to numerous upper and lower urinary tract procedures.We describe our surgical technique and perioperative outcome ofrobotic distalureterectomy with psoas hitch and ureteroneocystostomy fordistalureteralpathologies.Eight patients with a median age of 69.5 years old underwent robotic distal ureterectomy with psoas hitch and ureteroneocystostomy between April 2009 and August 2014.The entirety of all cases was performed robotically by a single surgeon at a tertiary academic medical center.Median operative time was 285 min(range:210-360 min),estimated blood loss was 50 mL(range:50-75 mL)and median length of hospital stay was 2.5 days(range:1-6 days). There was one post-operative complication,a readmission for dehydration(Clavien I).It suggests that robotic distal ureterectomy with psoas hitch and ureteroneocystostomy is a safe and effective minimally invasive alternative for patients with distal ureteral pathology.
©2015 Editorial Office of Asian Journal of Urology.Production and hosting by Elsevier (Singapore)Pte Ltd.This is an open access article under the CC BY-NC-ND license(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
1.Introduction
Laparoscopic ureterectomy was first described by Chadhoke and colleagues in 1993[1].More recently robotic surgery has expanded to address lower urinary tract procedures including ureteral pathologies following the success of robotic prostatectomy and partial nephrectomy [2-5].Herein,we present our institutional experience and description of robotic distal ureterectomy with psoas hitch and ureteroneocystostomy for distal ureteral pathology.
2.Patients and metho ds
Following institutional review board approval,a retrospective chart review was performed at a large tertiary care academic institution to identify patients who underwent robotic distal ureterectomy for the treatment ofdistal ureteral pathology including urothelial carcinoma or benign stricture disease from April 2009 to August 2014.All patients underwent appropriate diagnostic imaging and evaluation including history and physical examination, cystoscopy,routine serum chemistries and cross sectional imaging with CT or MRI.Patients were offered all reasonable options depending on their underlying pathology to include surveillance,endoscopic,open,laparoscopic and robotic management with their attendant risks and benefits.The entirety of all procedures was performed robotically by a single surgeon at a tertiary academic medical center.
3.Technique
3.1.Preoperative preparation
The patient is given one bottle of magnesium citrate the day prior to surgery and diet is limited to clears.A broadspectrum antibiotic such as cefazolin is administered intravenously within 30 min of incision.Sequential compression stockings are placed on the lower extremities. After the induction of anesthesia,an orogastric tube is placed.
3.2.Patient positioning and port placement
Patient positioning is similar to that for robotic prostatectomy.The patient is positioned supine and the arms are tucked to the sides.The patient legs are adducted and slightly flexed.The patient is secured to the operating table using 3 inch cloth tape over the chest.An 18 Fr urethral catheter is placed at the beginning of the case. A Veress needles is used to create pneumoperitoneum. A 12-mm trocar is placed at or slightly above the level of the umbilicus.The patient is then placed in steep Trendelenburg.Two 8-mm trocars are placed lateral to the rectus muscle on either side near the anterior axillary line and just below the level of the umbilicus.An additional 8-mm trocar is placed two to three finger breadths above the iliac crest on the left to accommodate the fourth robotic arm.For the assistant,a 12-mm trocar is placed in the right lower quadrant.
3.3.Exposure of ureter
Maryland bipolar forceps and curved monopolar scissors are used for the left and robotic arms respectively.The fourth arm contains a Prograsp forceps.A 30-degree down lens was used throughout the dissection.The posterior peritoneum is incised at the level of the iliac vessels above the ureter of interest.Once identified,the ureter is dissected distally towards the posterior bladder to the level of the ureterovesical junction.Division of the ipsilateral vas deferens in a male patient or suspensory/broad,round and infundibulopelvic ligaments in a female patient may aid in identification and exposure of the distal ureter.Importantly,necessary division of the ipsilateral medial umbilical ligament allows for the bladder to be rotated medially,thus improving exposure and visualization of the ureterovesical junction(Fig.1).Additionally,the superior and sometimes inferior vesical arteries require division to fully mobilize the ipsilateral bladder.When the surgery is being performed for urothelial cancer of the ureter,the ureter can be clipped early in the dissection thus containing the cancer and reducing the risk of tumor seeding the lower urinary tract(Fig.2).
3.4.Excision of diseased segment
When performing a distal ureterectomy for ureteral cancer, intravesical mitomycin C(40 mg)is instilled 1 h prior to cystotomy and excision of the ureteral orifice.In addition, the bladder is thoroughly rinsed with 300-400 mL of sterile saline to ensure complete clearance of mitomycin C from the bladder.The diseased segment of the ureter and a formal bladder cuff is excised in an extravesical approach with visual confirmation of complete excision of the ipsilateral ureteral orifice.The disease segment is immediately entrapped within a specimen sack for later extraction.The cystotomy is then closed with a two-layered sutured repair using a 3-0 polyglactin suture(Fig.3).
3.5.Mobilization of the bladder
In preparation for psoas hitch reconstruction,the bladder is further dissected from the anterior abdominal wall by dividing the urachus and contralateral medial umbilical ligament(Fig.4).In our experience dividing the contralateral pedicle has not been necessary.However,care must be taken to leave adequate blood supply if the ipsilateral pedicle is taken during mobilization of the bladder to remove the distal ureter and bladder cuff for cancer cases.
3.6.Psoas hitch
When performing a psoas hitch,the psoas minor tendon is identified immediately superior and lateral to the ipsilateral common iliac vessels.A 2-0 PDS suture is used to fix the ipsilateral dome of the bladder to the psoas muscle and tendon.Care must be taken to avoid injury to the nearby genitofemoral nerve(Fig.5).
3.7.Ureteroneocystostomy
An approximately 1.5 cm incision is made in the bladder dome along the anterolateral surface in a location where the remnant ureter can be implanted in a tension free manner.The ureter is spatulated posteriorly and an extravesical mucosa to mucosa anastomosis is performed using 4-0 polyglactin suture in an interrupted fashion (Fig.6).Prior to closing the anterior portion of the anastomosis,a ureteral stent is placed in a retrograde fashion with the aid of a guide wire(Fig.7).The anastomosis is tested by filling the bladder with 150-200 mL of normal saline.A closed suction drain is then placed(Fig.8).The specimen is extracted and all port sites are closed.
3.8.Post-operative care
Most patients can be safely discharged by postoperative day 2.The pelvic drain can be removed prior to discharge as long as outputs are low.The urethral catheter is removed7-10 days after surgery.A cystogram can be performed prior to removal of the urethral catheter.In this series no patient required a cystogrambecause allpatients had a water closure intraoperatively and low drain output postoperatively.The ureteral stent is removed 4 weeks after surgery.
4.Results
Table 1 lists patient demographics and perioperative data for the robotic distal ureterectomy group.The median age was 69.5 years(46-91).The median operative time was 285 min(range:210-330 min),estimated blood loss was 50 mL(range:50-75 mL),median length of stay was 2.5 days(1-6),and there was one complication in this group involving readmission for failure to thrive and dehydration (Grade II).Four of the patients underwent surgery for ureteral strictures secondary to stone disease with pathology demonstrating fibrosis.The remaining four patients underwent surgery for upper tract urothelial carcinoma. Pathology was carcinoma in situ(CIS)in one patient,pT1 in one patient,pT2 in one patient and pT3 in one patient. Lymph node dissection was performed in all four patients and they were N0 collectively.All surgical margins were negative.The remaining four patients were done for stricture disease/fibrosis.
5.Discussion
With the recent expansion of robotic surgery in the field of urology,the robotic platform has being applied to treat many genitourinary disease processes in both the upper and lower urinary tract.For appropriately selected patients, robotic distal ureterectomy is a viable treatment option. The robotic platform has some distinct advantages over both open and laparoscopic approaches.The articulating wrist of the robot facilitates easier intracorporeal suturing for the psoas hitch and the anastomosis as compared to conventional laparoscopy.The 10×magnification allows forbetter visualization and more precise dissection.As compared to open surgery,the same standards of surgical repair can be achieved in a minimally invasive fashion with less incisional morbidity and postoperative convalescence.
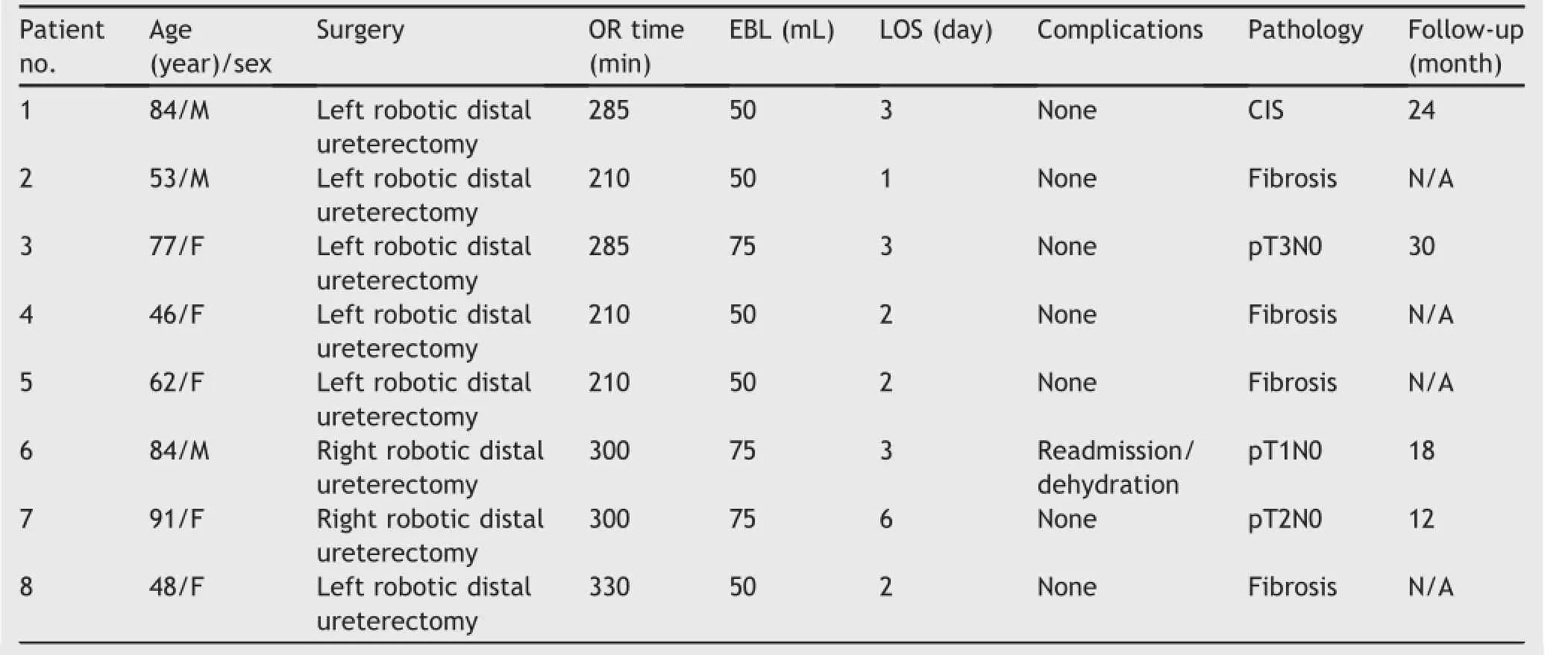
Table 1Patient demographics and operative details.
6.Conclusion
The technique of robotic distal ureterectomy with psoas hitch and ureteroneocystostomy is an excellent alternative to other surgical techniques for treating various distal ureteral pathologies.Advantages include ease and precision of excision of the ureter and bladder cuff as well as efficiency in intracorporeal suturing.
Conflicts of interest
The authors declare no conflict of interest.
[1]Chadhoke PS,Clayman RV,Kerbl K,Figenshau RS, McDougall EM,Kavoussi LR,et al.Laparoscopic ureterectomy: initial clinical experience.J Urol 1993;149:992-7.
[2]Phillips EA,Wang DS.Current status of robot-assisted laparoscopic ureteral reimplantation and reconstruction.Curr Urol Rep 2012;13:190-4.
[3]Kozinn SI,Canes D,Sorcini A,Moinzadeh A.Robotic versus open distal ureteral reconstruction and reimplantation for benign stricture disease.J Endourol 2012;26:147-51.
[4]Baldie K,Angell J,Ogan K,Hood N,Pattaras JG.Robotic management of benign mid and distal ureteral strictures and comparison with laparoscopic approaches at a single institution.Urology 2012;80:596-601.
[5]McClain PD,Mufarrij PW,Hemal AK.Robot-assisted reconstructive surgery for ureteral malignancy:analysis of efficacy and oncologic outcomes.J Endourol 2012;26:1614-7.
Received 22 October 2014;received in revised form 3 December 2014;accepted 19 January 2015 Available online 16 April 2015
*Corresponding author.
E-mail address:sulm@urology.uf l.edu(L.-M.Su).
Peer review under responsibility of Chinese Urological Association and SMMU.
http://dx.doi.org/10.1016/j.ajur.2015.04.017
2214-3882/©2015 Editorial Office of Asian Journal of Urology.Production and hosting by Elsevier(Singapore)Pte Ltd.This is an open access article under the CC BY-NC-ND license(http://creativecommons.org/licenses/by-nc-nd/4.0/).
 Asian Journal of Urology2015年2期
Asian Journal of Urology2015年2期
- Asian Journal of Urology的其它文章
- All about Peyronie’s disease
- Testis sperm extraction
- Surgical management of nonobstructive azoospermia
- Non-invasive transcutaneous electrical stimulation in the treatment of overactive bladder
- Contemporary review of the 532 nm laser for treatment of benign prostatic hyperplasia
- Percent free prostate-specific antigen for prostate cancer diagnosis in Chinese men with a PSA of 4.0-10.0 ng/mL:Results from the Chinese Prostate Cancer Consortium
