低位直肠癌经括约肌间切除的现状和进展
何 苗,范 晶,王子卫(综述),赵和照※(审校)
( 1.重庆市肿瘤研究所胃肠外科,重庆 400030; 2.重庆医科大学附属第一医院 a.急诊科,b.普通外科,重庆 400016)
低位直肠癌经括约肌间切除的现状和进展
何苗1,范晶2a,王子卫2b(综述),赵和照1※(审校)
(1.重庆市肿瘤研究所胃肠外科,重庆 400030; 2.重庆医科大学附属第一医院 a.急诊科,b.普通外科,重庆 400016)
摘要:低位直肠癌的手术治疗通常采用经腹会阴联合切除术(APR),该术式无法保留肛门,不可避免行永久结肠造口,明显改变患者生活习惯。近年经括约肌间切除术(ISR)成为研究热点,其可实现低位直肠癌的手术根治并保留肛门。该文综述ISR术的背景、类型、适应证、禁忌证、并发症、疗效及对排便功能的影响,发现若病例选择适当,ISR术可能是低位直肠癌手术治疗的新选择。
关键词:直肠癌;经括约肌间切除;现状;进展
低位直肠癌(肿瘤下缘距齿状线﹤5 cm)的治疗一直以经腹会阴联合切除(abdomino perineal resection,APR)术为经典方法,加上全直肠系膜切除及新辅助化疗的应用,该疾病的治疗效果已有显著改善。但人们对术后生活质量的讨论已逐渐增多,APR术无法保留肛门,不可避免地行永久结肠造口,明显改变患者生活习惯。近年,经括约肌间切除(intersphincteric resection,ISR)术逐渐成为低位直肠癌外科治疗的研究热点,该术式意在保留肛门外括约肌及部分内括约肌,行结肠肛门吻合,从而达到低位直肠癌手术根治并保留肛门的目的。该文回顾ISR相关文献,综述其现状及进展。
1ISR术背景
1992年,Braun等[1]首先应用ISR治疗超低位直肠癌,其术式经发展可简述为:在腹腔遵全直肠系膜切除原则游离直肠至肛提肌平面;在肛门于括约肌间沟切开肛管皮肤,分离内括约肌直至将直肠和内括约肌全部(或部分)切除,再行结肠-肛管吻合,从而实现低位直肠癌根治及保肛;其中近端结肠可作J型袋再与肛管吻合,也可行回肠造口术,于2~12个月后还纳造瘘肠段。超低位的直肠前切除(利用双吻合技术)不属于ISR范畴。ISR与APR术在腹腔操作部分基本一致,其区别体现在肛门操作:①前者保留肛门及肛门外括约肌,后者完整切除肛门及肛门内外括约肌;②前者行结肠肛门吻合,后者行结肠造口并关闭盆底。ISR术难度在于找准括约肌间隙及结肠肛管吻合。一般认为ISR术和APR术在手术时间上差异无统计学意义。目前尚未对ISR的适应证达成一致意见,但也形成部分共识。首先需利用肛门指检、直肠镜检查、磁共振成像及超声内镜等技术对直肠癌进行术前评估,特别关注肿瘤与齿状线、肛门括约肌的关系及其浸润深度;一般认为ISR的手术指征为:①肿瘤在直肠壁内或仅浸润肛门内括约肌;②术前良好的括约肌功能及排便功能;③无肿瘤远处转移[2]。对于T3-4(肿瘤穿透肠壁甚至累及邻近组织器官)及淋巴结阳性的病例有通过新辅助放化疗实现直肠癌降级降期后再行ISR术的报道[3]。但对于侵袭外括约肌、肛提肌、耻骨直肠肌及T4(肿瘤侵入邻近器官)的直肠癌,若又对新辅助放化疗不敏感,或术前肛门功能差,又或病理类型为未分化癌的病例则为ISR禁忌证;ISR术根据肛门内括约肌的切除范围可分完全、次全及部分切除3种:当癌肿侵犯齿状线,远切缘在括约肌间沟时,内括约肌被完整切除,即为完全ISR;当肿瘤远端距齿状线>2 cm,远切缘在齿状线和括约肌间沟之间时,即为次全ISR;若癌肿距齿状线较远,远切缘距离齿状线较远,则为部分ISR(图1[4])。术中注意,远切缘必须冰冻病理切片证实无癌细胞浸润,否则改行APR术。目前ISR治疗低位直肠癌的腹腔操作部分可通过腹腔镜[5]或机器人辅助完成[6]。
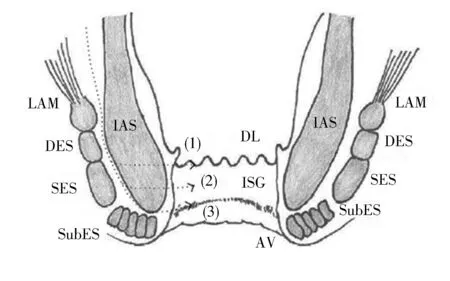
①部分ISR:内括约肌远切缘在齿状线;②次全ISR:内括约肌远切缘在齿状线与括约肌间沟之间;③完全ISR:内括约肌远切缘在括约肌间沟。AV:肛缘;DES:外括约肌深部;DL:齿状线;IAS:肛门内括约肌;ISG:括约肌间沟;LAM:肛提肌;SES:外括约肌浅部;SubES:外括约肌皮下部
图1经括约肌间切除切除(ISR)术分类
2ISR术现状
2.1ISR术后并发症与病死率ISR术常见并发症包括吻合口瘘、吻合口狭窄、直肠阴道瘘、盆腔感染、出血、直肠脱垂等(表1)。其中吻合口瘘需特别重视,因其导致盆腔感染和直肠阴道瘘,并且和心肌梗死、急性肺栓塞是患者术后死亡的重要原因[3]。若出现术后吻合口瘘,建议行回肠造口术(若ISR术中未作)或经皮穿刺引流术,虽然造口术并不一定防止吻合口瘘发生,但能缓解吻合口瘘造成的局部感染[4]。有资料认为,术中输血及肺部疾病是吻合口瘘的独立危险因素[7]。而如果吻合口瘘原因是肠管缺血,则需重新吻合或改行APR术。ISR术后30 d病死率一般<1%,在可接受范围内(表1)。
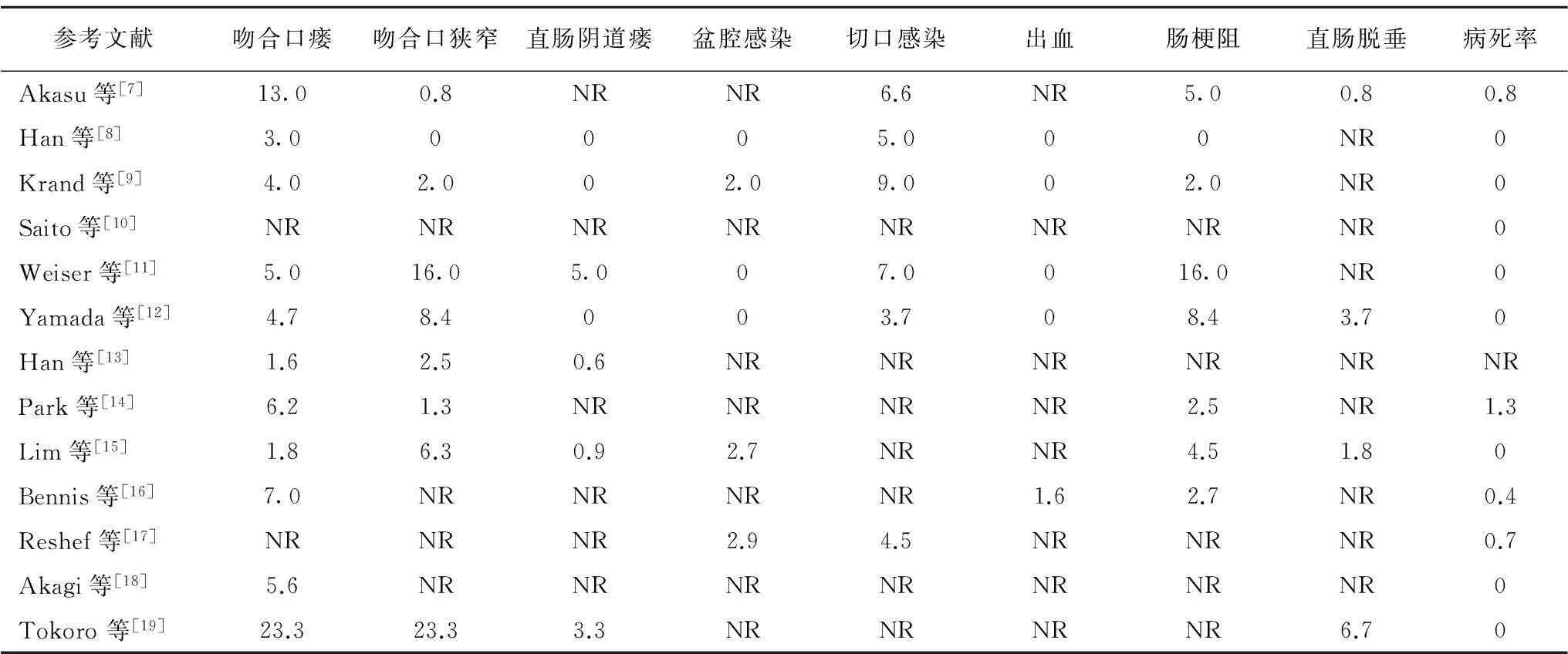
表1 ISR术后并发症发生率与病死率 (%)
ISR:经括约肌间切除;NR:未记录
2.2ISR治疗直肠癌的效果研究发现,ISR术后直肠癌局部复发率在2%~13.3%,T3的复发率通常高于Tis-T2[19],而ISR术并不增加直肠癌术后局部复发率[10]。一般认为局部复发的原因包括:未完整切除直肠系膜、远切缘癌累及、癌肿侵及外括约肌、盆腔淋巴结转移、癌细胞脱落、CA19-9>37 000 U/L、肿瘤细胞分化差等[4,15,20]。直肠癌ISR术后5年总生存率为66%~97%,而5年无瘤生存率为68%~87%(表2)。有研究发现,ISR术后平均5年生存率及5年无瘤生存率分别为86.3%和78.6%[3]。而ISR术后肿瘤局部复发率及总5年生存率可能比APR术更具优势[10,21],提示ISR术可获得较理想的直肠癌治疗效果。
2.3ISR术后肛门功能ISR术的重要目的是保留肛门对排便节律的控制,并达到理想的术后生活质量。虽然不同文献报道ISR术后肛门排便功能差异大,并且所采用的评估方法也不同(表3),但总体趋势是:ISR术后短期有明显肛门失禁,术后12个月较术后3个月有显著肛门功能改善,并逐渐恢复至术前水平[22]。影响 ISR术后肛门功能的因素有:①腹部手术未按全直肠系膜切除原则进行,未保护好相关神经,导致术后大小便失禁、阳痿等;②肿瘤远端与肛门直肠环的距离<1 cm,吻合口与肛缘的距离<2 cm,影响术后肛门功能[23];③高龄或本身肛门括约肌松弛[24],无法实现术后理想肛门功能;④有研究发现术前放化疗不利术后肛门功能恢复[22,25-26];⑤术中切除肛门内括约肌越多,术后肛门功能恢复越差[4]。故有人建议将T3~4需要术前放化疗的患者及老年患者均排除在ISR术适应证外;此外,术中行近端结肠J型袋或结肠成形术可一定程度改善肛门失禁[27],但ISR术前仍需告知患者术后肛门功能失调可能。
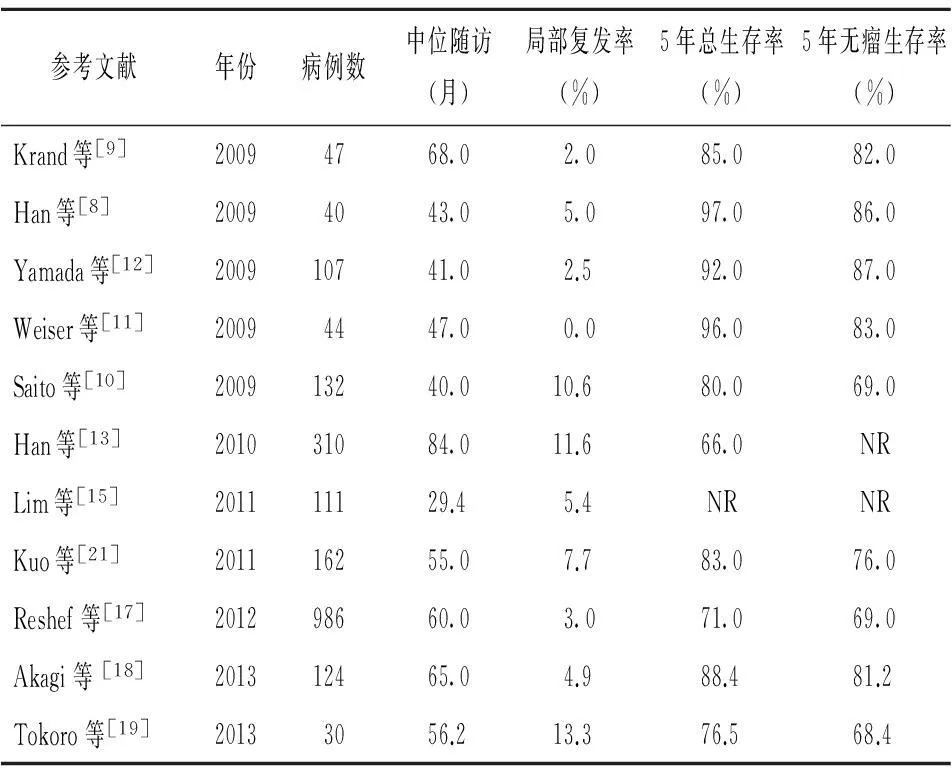
表2 ISR术治疗直肠癌的效果
ISR:经括约肌间切除;NR:未记录
2.4ISR与APR术的疗效比较ISR与APR术的手术适应证并不一致,所以行ISR与APR术的患者存在一定异质性(如APR组的患者年龄较大,低分化直肠癌较多等)[11]。故目前尚无法理想比较ISR与APR术的优劣,但大多观点认为,ISR术后5年总生存率及无瘤生存率与APR术比较并无差异,甚至更好[10-11],故若筛选患者合适,ISR术具有代替APR术的潜力(表4)。
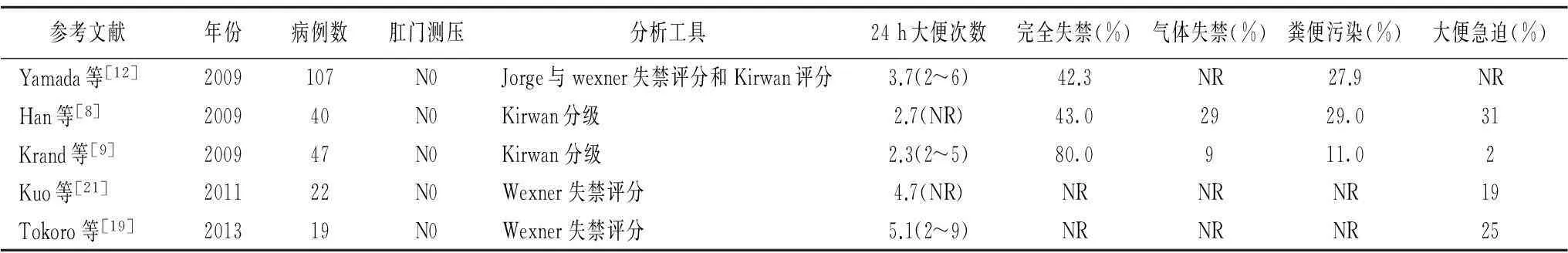
表3 ISR术后肛门功能
ISR:经括约肌间切除;NR:未记录;N0:未进行肛门测压
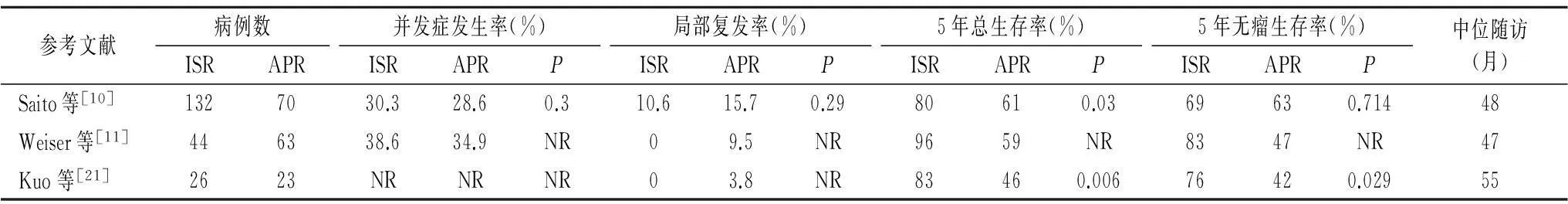
表4 ISR与APR的疗效比较
ISR:经括约肌间切除;APR:经腹会阴联合切除;NR:未记录
3展望
手术治疗低位直肠癌必须兼顾根治切除和生活质量两方面需求,ISR术提供低位直肠癌保肛的可能。ISR术前必须对低位直肠癌患者进行仔细评估,一般认为术前肛门外括约肌受侵犯、肛门功能差、低分化或未分化癌不宜行ISR术。而早期、高分化、对新辅助放化疗敏感的低位直肠癌较适合ISR术。新辅助放化疗虽可使直肠癌降期,但可能不利于ISR术后肛门功能的恢复(特别是术前放疗)。目前ISR术和APR术的比较研究尚少,但如果能获得足够的远切缘,ISR术后肿瘤复发率、并发症、病死率及生存时间均可接受,甚至优于APR术。ISR术可能是低位直肠癌手术治疗的又一选择。
参考文献
[1]Braun J,Treutner KH,Winkeltau G,etal.Results of intersphincteric resection of the rectum with direct coloanal anastomosis for rectal carcinoma[J].Am J Surg,1992, 163(4):407-412.
[2]Spanos CP.Intersphincteric resection for low rectal cancer:an overview[J].Int J Surg Oncol,2012,2012:241512.
[3]Martin ST,Heneghan HM,Winter DC.Systematic review of outcomes after intersphincteric resection for low rectal cancer[J].Br J Surg,2012,99(5):603-612.
[4]Cipe G,Muslumanoglu M,Yardimci E,etal.Intersphincteric resection and coloanal anastomosis in treatment of distal rectal cancer[J].Int J Surg Oncol,2012,2012:581258.
[5]Shiomi A,Kinugasa Y,Yamaguchi T,etal.Feasibility of laparoscopic intersphincteric resection for patients with cT1-T2 low rectal cancer[J].Dig Surg,2013,30(4-6):272-277.
[6]Baek SJ,Al-Asari S,Jeong DH,etal.Robotic versus laparoscopic coloanal anastomosis with or without intersphincteric resection for rectal cancer[J].Surg Endosc,2013,27(11):4157-4163.
[7]Akasu T,Takawa M,Yamamoto S,etal.Risk factors for anastomotic leakage following intersphincteric resection for very low rectal adenocarcinoma[J].J Gastrointest Surg,2010,14(1):104-111.
[8]Han JG,Wei GH,Gao ZG,etal.Intersphincteric resection with direct coloanal anastomosis for ultralow rectal cancer:the experience of People′s Republic of China[J].Dis Colon Rectum,2009,52(5):950-957.
[9]Krand O,Yalti T,Tellioglu G,etal.Use of smooth muscle plasty after intersphincteric rectal resection to replace a partially resected internal anal sphincter:long-term follow-up[J].Dis Colon Rectum,2009,52(11):1895-1901.
[10]Saito N,Sugito M,Ito M,etal.Oncologic outcome of intersphincteric resection for very low rectal cancer[J].World J Surg,2009,33(8):1750-1756.
[11]Weiser MR,Quah HM,Shia J,etal.Sphincter preservation in low rectal cancer is facilitated by preoperative chemoradiation and intersphincteric dissection[J].Ann Surg,2009,249(2):236-242.
[12]Yamada K,Ogata S,Saiki Y,etal.Long-term results of intersphincteric resection for low rectal cancer[J].Dis Colon Rectum,2009,52(6):1065-1071.
[13]Han F,Li H,Zheng D,etal.A new sphincter-preserving operation for low rectal cancer:ultralow anterior resection and colorectal/coloanal anastomosis by supporting bundling-up method[J].Int J Colorectal Dis,2010,25(7):873-880.
[14]Park JS,Choi GS,Jun SH,etal.Laparoscopic versus open intersphincteric resection and coloanal anastomosis for low rectal cancer:intermediate-term oncologic outcomes[J].Ann Surg,2011,254(6):941-946.
[15]Lim SW,Huh JW,Kim YJ,etal.Laparoscopic intersphincteric resection for low rectal cancer[J].World J Surg,2011,35(12):2811-2817.
[16]Bennis M,Parc Y,Lefevre JH,etal.Morbidity risk factors after low anterior resection with total mesorectal excision and coloanal anastomosis:a retrospective series of 483 patients[J].Ann Surg,2012,255(3):504-510.
[17]Reshef A,Lavery I,Kiran RP.Factors associated with oncologic outcomes after abdominoperineal resection compared with restorative resection for low rectal cancer:patient-and tumor-related or technical factors only?[J].Dis Colon Rectum,2012,55(1):51-58.
[18]Akagi Y,Shirouzu K,Ogata Y,etal.Oncologic outcomes of intersphincteric resection without preoperative chemoradiotherapy for very low rectal cancer[J].Surg Oncol,2013,22(2):144-149.
[19]Tokoro T,Okuno K,Hida J,etal.Analysis of the clinical factors associated with anal function after intersphincteric resection for very low rectal cancer[J].World J Surg Oncol,2013,11:24.
[20]Fujita S,Yamamoto S,Akasu T,etal.Risk factors of lateral pelvic lymph node metastasis in advanced rectal cancer[J].Int J Colorectal Dis,2009,24(9):1085-1090.
[21]Kuo LJ,Hung CS,Wu CH,etal.Oncological and functional outcomes of intersphincteric resection for low rectal cancer[J].J Surg Res,2011,170(1):93-98.
[22]Ito M,Saito N,Sugito M,etal.Analysis of clinical factors associ-ated with anal function after intersphincteric resection for very low rectal cancer[J].Dis Colon Rectum,2009,52(1):64-70.
[23]Denost Q,Laurent C,Capdepont M,etal.Risk factors for fecal incontinence after intersphincteric resection for rectal cancer[J].Dis Colon Rectum,2011,54(8):963-968.
[24]Nagayama S,Al-Kubati W,Sakai Y.What is the place of intersphincteric resection when operating on low rectal cancer?[J].ISRN Surg,2012,2012:585484.
[25]Akasu T,Takawa M,Yamamoto S,etal.Intersphincteric resection for very low rectal adenocarcinoma:univariate and multivariate analyses of risk factors for recurrence[J].Ann Surg Oncol,2008,15(10):2668-2676.
[26]Chamlou R,Parc Y,Simon T,etal.Long-term results of intersphincteric resection for low rectal cancer[J].Ann Surg,2007,246(6):916-921.
[27]Bretagnol F,Rullier E,Laurent C,etal.Comparison of functional results and quality of life between intersphincteric resection and conventional coloanal anastomosis for low rectal cancer[J].Dis Colon Rectum,2004,47(6):832-838.
Current Status and Research Progress of ISR for Low Rectal Cancer
HEMiao1,FANJing2a,WANGZi-wei2b,ZHAOHe-zhao1.
(1.DepartmentofGastrointestinalSurgery,ChongqingCancerInstitute,Chongqing400030,China; 2a.DepartmentofEmergency, 2b.DepartmentofGeneralSurgery,theFirstAffiliatedHospitalofChongqingMedicalUniversity,Chongqing400016,China)
Abstract:Abdominoperineal resection(APR,Miles) is a traditional operation for patients with low rectal cancer.But permanent colostomy is inevitable for such operation and will change the patients′ living habits significantly.These years,intersphincteric resection(ISR) has become a hot topic.ISR can radically resect the neoplasm,meanwhile preserve the anus for the patient with low rectal cancer.Here is to make a review of the background,types,indications,contraindications,complications,oncological outcomes and anal functional assessments of ISR,suggesting ISR may offer an alternative to traditional APR for rectal cancer in selected patients.
Key words:Rectal cancer; Intersphincteric Resection; Current status; Progress
收稿日期:2014-05-26修回日期:2014-08-19编辑:郑雪
doi:10.3969/j.issn.1006-2084.2015.07.026
中图分类号:R615; R657.1
文献标识码:A
文章编号:1006-2084(2015)07-1220-03
- 医学综述的其它文章
- 与三叉神经传导通路有关的诱发电位检测