Emergency physician's perception of cultural and linguistic barriers in immigrant care: results of a multiple-choice questionnaire in a large Italian urban emergency department
Filippo Numeroso, Mario Benatti, Caterina Pizzigoni, Elisabetta Sartori, Giuseppe Lippi, Gianfranco Cervellin
1Emergency Department, Academic Hospital of Parma, Parma, Italy
2Service of Clinical Governance, Academic Hospital of Parma, Parma, Italy
3Laboratory of Clinical Chemistry and Hematology, Academic Hospital of Parma, Parma, Italy
Emergency physician's perception of cultural and linguistic barriers in immigrant care: results of a multiple-choice questionnaire in a large Italian urban emergency department
Filippo Numeroso1, Mario Benatti1, Caterina Pizzigoni1, Elisabetta Sartori2, Giuseppe Lippi3, Gianfranco Cervellin1
1Emergency Department, Academic Hospital of Parma, Parma, Italy
2Service of Clinical Governance, Academic Hospital of Parma, Parma, Italy
3Laboratory of Clinical Chemistry and Hematology, Academic Hospital of Parma, Parma, Italy
BACKGROUND:A poor communication with immigrants can lead to inappropriate use of healthcare services, greater risk of misdiagnosis, and lower compliance with treatment. As precise information about communication between emergency physicians (EPs) and immigrants is lacking, we analyzed difficulties in communicating with immigrants in the emergency department (ED) and their possible associations with demographic data, geographical origin and clinical characteristics.
METHODS:In an ED with approximately 85 000 visits per year, a multiple-choice questionnaire was given to the EPs 4 months after discharge of each immigrant in 2011.
RESULTS:Linguistic comprehension was optimal or partial in the majority of patients. Signif cant barriers were noted in nearly one fourth of patients, for only half of them compatriots who were able to translate. Linguistic barriers were mainly found in older and sicker patients; they were also frequently seen in patients coming from western Africa and southern Europe. Non-linguistic barriers were perceived by EPs in a minority of patients, more frequently in the elderly and frequent attenders. Factors independently associated with a poor f nal comprehension led to linguistic barriers, non-linguistic obstacles, the absence of intermediaries, and the presence of patient's fear and hostility. The latter probably is a consequence, not the cause, of a poor comprehension.
CONCLUSION:Linguistic and non-linguistic barriers, although quite infrequent, are the main factors that compromise communication with immigrants in the ED, with negative effects especially on elderly and more seriously ill patients as well as on physician satisfaction and appropriateness in using services.
Linguistic barriers; Cultural barriers; Immigrants; Emergency department
INTRODUCTION
According to the most recent statistics of the United Nations (UN), immigrants account for approximately 3% of the worldwide population, with a peak of nearly 9% in Europe.[1]Due to constantly growing migratory f uxes, also observed in our country,[2]the healthcare services have to face the issue of serving an increasing number of immigrants and providing equity of access to healthcare services for this population.
The utilization of primary and specialized care carries several problems for immigrants, which mainly include language barriers and lack of knowledgeof system organization (e.g., how to access to these services). Consequently, the emergency departments (EDs) are the first, if not the only, reference healthcare settings, especially for irregular immigrants; although scarce and often controversial data are available on utilization of the EDs by immigrants, some reports seem to conf rm higher rates of access.[3–10]
In 2011, the Regional Health and Social Care Agency published a dossier on the health status immigrants in the Emilia Romagna Region, that is the region where our Hospital is located, confirming that despite hospitalization is overall lower among immigrants than among the native population (after excluding obstetric causes), immigrants, especially irregular immigrants, tend to undergo urgent hospitalization more frequently.[11]
A successful management of patient needs is largely dependent on bridging the gap in the mutual expectations between patients and physicians, with communicative aspects being one of the most crucial issues.[12–14]Several reasons for non-effective communication have been investigated, such as cultural differences, linguistic barriers and educational level.[15–17]
Linguistic difficulties, that are the most frequent among these possible obstacles, may lead to many negative consequences, such as poor therapeutic compliance, feelings of fear and desire of "different" care.[18–19]
Some studies[14,20–22]have shown more misunderstandings between physicians and ethnic minority subjects than native patients, thus leading to inappropriate use of healthcare services, greater risk of misdiagnosis, and lower compliance with treatment. Other studies[12–14,23,24]showed that physician workload is higher with ethnic minority patients due to different means of communication, distinct needs, and higher frequency of visits.
Since few studies[25]have assessed the issue of communication problems between emergency physicians (EPs) and immigrants, we analyzed the difficulties in communicating with immigrants because of linguistic or non-linguistic barriers (related to cultural factors, educational level or external inf uences) and the possible associations with demographic data, geographical origin and clinical characteristics.
METHODS
Study design
We conducted an observational, cross sectional, descriptive study in accordance with the Declaration of Helsinki. According to the rules of our country,[26]we obtained ethical board approval because the study was based on an internal survey administered to the EPs, without any implication in therapeutic decisions.
Study setting and population
The study was carried out in the ED of the University Hospital of Parma, a large urban ED with approximately 85 000 visits yearly. The foreign-born population represents almost 13% of overall residents in the city of Parma, with immigrants from 137 countries currently residing in the city and its neighborhoods. The most important community is composed of immigrants from Moldavia, followed by Albania, Romania, Morocco and Tunisia.
Study protocol and measurements
During a period of four or three months in 2011 after discharge of each immigrant patient, a multiplechoice questionnaire (Figure 1) was administrated to the EPs, covering the following aspects: linguistic barrier; physician perception about the final level of patient understanding; final satisfaction of the EP; EP's perception of patient's fear and hostility; nonlinguistic barriers (related to the level of education, cultural factors or religious beliefs) or external inf uences (often represented by coworkers or family members). The questionnaire was developed in this way in order to investigate the presence of any condition that can impact communication, such as linguistic and nonlinguistic barriers but also external factors (presence of intermediaries, influences related to family or work,medical or patient aversion). It should be emphasized that the aim of the study was to investigate the EP's perception of cultural and linguistic barriers in immigrant care, and not the actual prevalence of cultural or linguistic barriers; as such, the questionnaire was administered only to the physicians whereas no matching questionnaire was administered to the patients, mainly for practical reasons (it would have been virtually impossible to ensure the presence of multilingual interpreters into the ED 24 hours a day for research purposes).
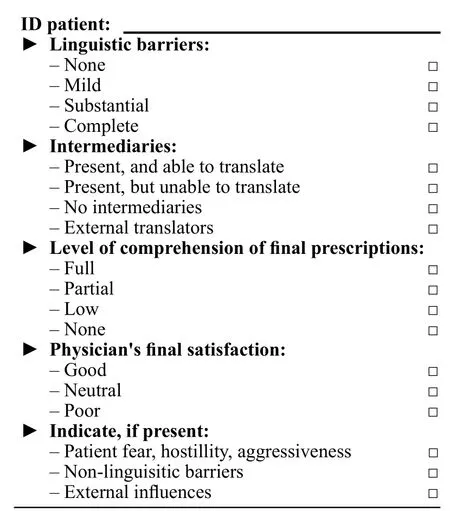
Figure 1. The questionnaire.
At the same time, information on demographic data (age and gender), geographical origin (classified according to the UN geo-scheme),[27]priority triage code (using the following color-coding system: red, high priority; yellow, medium priority; green, low priority; white, non-urgent cases), administrative status (i.e., registration with the NHS) and frequency of ED visit (classif ed on the basis of ED visits in the previous year as occasional, <3 visits/year, habitual, 3–6 visits/year, frequent, >6 visits/year) were collected.
Data analysis
All data were put into a SPSS statistical file (V 17.0) and analyzed by a contingency table. The Chisquare test was used to look for significant associations between variables and a linear regression analysis was made to highlight characteristics of patients with very poor or null final comprehension and some potentially problematic subgroups of patients (elderly patients, i.e. >60 years old; high priority codes, i.e. yellow or red; habitual or frequent attenders; patients with a poor physician final satisfaction) and also to individulize factors independently associated with a poor final comprehension.
RESULTS
During the study period, 479 questionnaires filled on a voluntary basis by all physicians of the ED (21 EPs, all native to Italy, mostly able to speak English as a bridge-language) were collected with a slight difference in individual participation rate. Due to the large number of immigrant patients consulting the ED on a daily basis (36 patients per day on average represent approximately 15% of the whole number of visits), the total number of questionnaires completed reflected a rather low response rate (approximately 15%), mostly attributable to the chaotic activity in the ED environment. The characteristics of the patients are shown in Table 1.
Most of the patients were relatively young (mean age 38 year) with a low priority triage code (white and green codes accounting for approximately 84% of cases) as reported previously.[10]Approximately 83% of the patients were occasional attenders, with less than 3 visits during the previous year. The prevalence of ethnicity was in substantial agreement with the number of representatives of each ethnic groups of our city, with the notable exception of patients born in western Africa (17.8% of overall questionnaires versus the prevalence of residents lower than 5%).
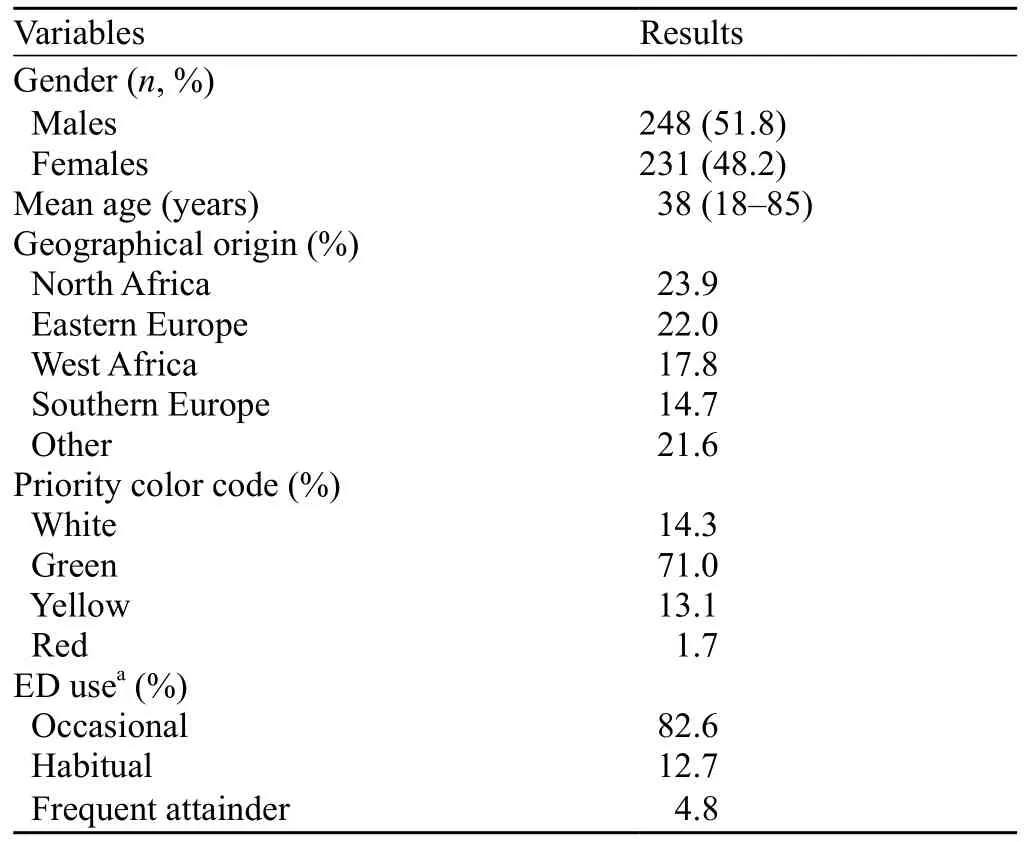
Table 1. The characteristics of patients
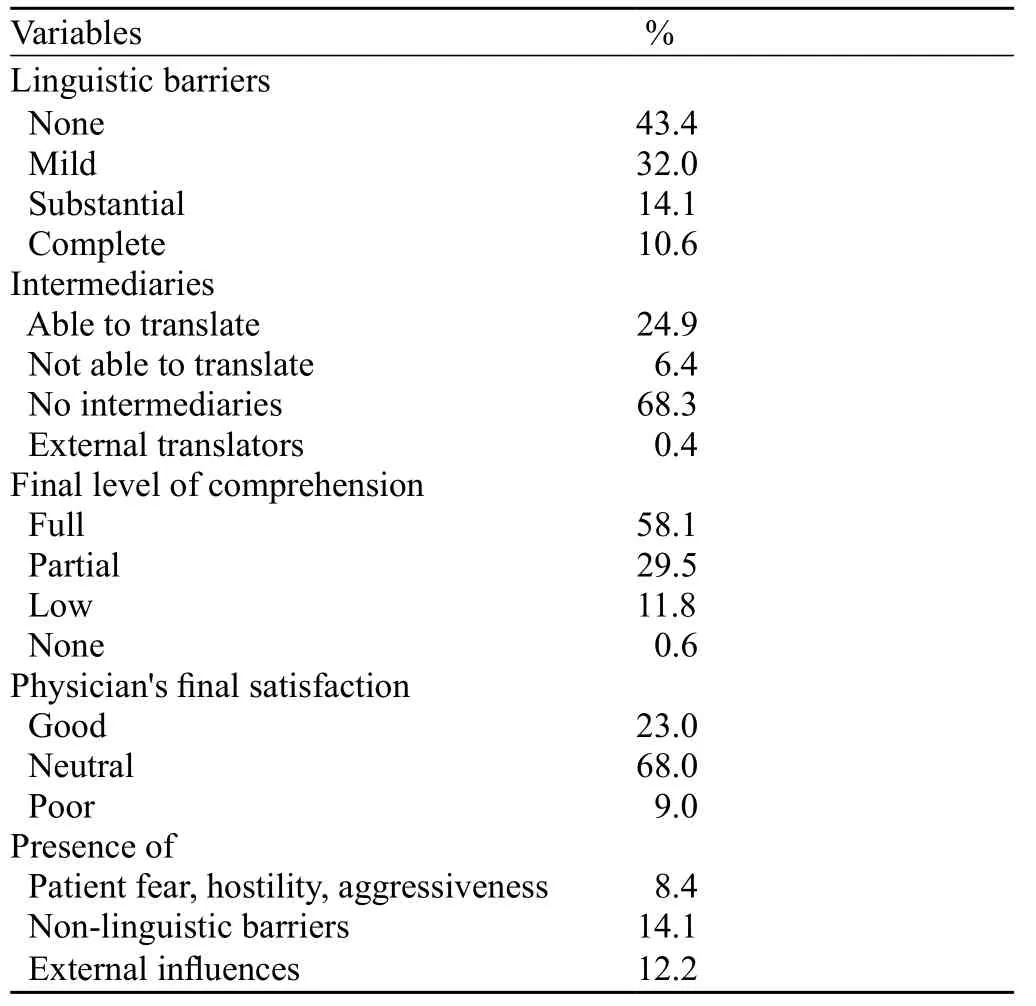
Table 2. Summary of EPs' responses

Table 3. Percentage of general population, patients with very poor or null f nal comprehension and some potentially problematic subgroups of patients
A summary of EPs' responses is shown in Table 2, whereas Table 3 shows the characteristics of patients with very poor or null f nal comprehension and those of the above mentioned potentially problematic subgroups of patients.
The level of linguistic comprehension was full (43.4%) or partial (32.0%) in most of visits, with significant linguistic barriers (that is substantial or complete) recorded in nearly one fourth of the patients (24.8%). Linguistic barriers were found most frequently in the elderly (58.3% in patients aged 60 years or older) and most notably in those with serious diseases (43.8% in patients with red or yellow triage codes). Higher levels of linguistic barriers, with poor or non-linguistic comprehension, were found in patients born in western Africa (35.0%) and southern Europe (33.8%), mainly Albania.
The presence of intermediaries able to translate the language was recorded in 24.9% of patients and most notably in 54% of patients with severe linguistic barriers. Intermediaries were also present in most of elderly patients (63.9%) and in 32.9% of those with a high priority triage code (red plus yellow codes).
Non-linguistic barriers were perceived by EPs in a minority of patients (14.1%), with a higher prevalence rate of 22.2% in the elderly. The ethnic groups with the higher prevalence of non-linguistic barriers were those from eastern Africa (30.0%) and from south Asia (28.8%).
According to EP's perception, the final level of complete comprehension was 58.1%, and that of very poor or null comprehension was 12.4%. A higher percentage of poor comprehension (i.e., patients discharged from the ED not aware of their clinical conditions) was observed in the elderly (19.4% of patients aged >60 years vs. 3% of patients ≤20 years), in those born in western Africa (19.8%), and in those with a high priority triage code (23.3% in patients with red and yellow code). It is also noteworthy, however, that the hospital admission rate for yellow and red codes was higher (45% and 88%, respectively), and the admitted patients can have more opportunities to communicate and be informed during their hospital stay.
Some aspects of fear and hostility were reported in 8.4% of the study population, with a slightly higher frequency (12.3%) in patients with a red and yellow code, whereas these aspects were almost negligible in patients born in southern Europe (2.8%).
The EPs perceived the presence of external inf uences in 12.2% of patients, and mostly in males. The ethnic groups in which external inf uences were represented were those from western Africa (17%) and eastern Africa (30%). EP's final satisfaction was neutral in most of patients (68%), good in 23%, and poor in 9%.
Although frequent attenders did not show a significant degree of linguistic barrier (20.0%), they showed higher levels of external influences (43.5%) and non-linguistic barriers (39.0%). Linguistic barriers (53.4%) and lack of intermediaries able to translate (76.1%) were present in most of patients with poor EP's f nal satisfaction. In this group, higher levels of hostility (27.9%), non-linguistic barriers (37.2%), external influences (30.2%), condition of frequent attenders (37.0%), and poor or null final comprehension (46.5%) were recorded.
The irregular immigrants, who were patients not registered with the Italian NHS, were from South Europe (36.6%). These immigrants demonstrated that linguistic barriers were perceived in 52.1% of them, with poor or no f nal comprehension in 17.4%. In these patients, there were also high levels of non-linguistic barriers, external inf uences, and aspects of fear and hostility.
In the patients with poor or no f nal comprehension, linguistic barrier was present in 83.3% of them, confirming that this still represents the leading obstacle in mutual comprehension between patients and EPs. Thepresence of intermediaries in these patients was different in comparison with the general population (25.3% vs. 25.0%), thus a linguistic "bridge" is often insufficient to fill the gap between EPs and immigrants. In patients with poor or no final comprehension, non-linguistic barriers accounted for 36.6%, fear for 16.6%, external influences for 23.0%, status of frequent attender for 21.1%. Linear regression analysis (Table 4) confirmed that the factors independently associated with a poor f nal comprehension were linguistic barriers, non-linguistic obstacles, absence of intermediaries, and patient's fear and hostility.
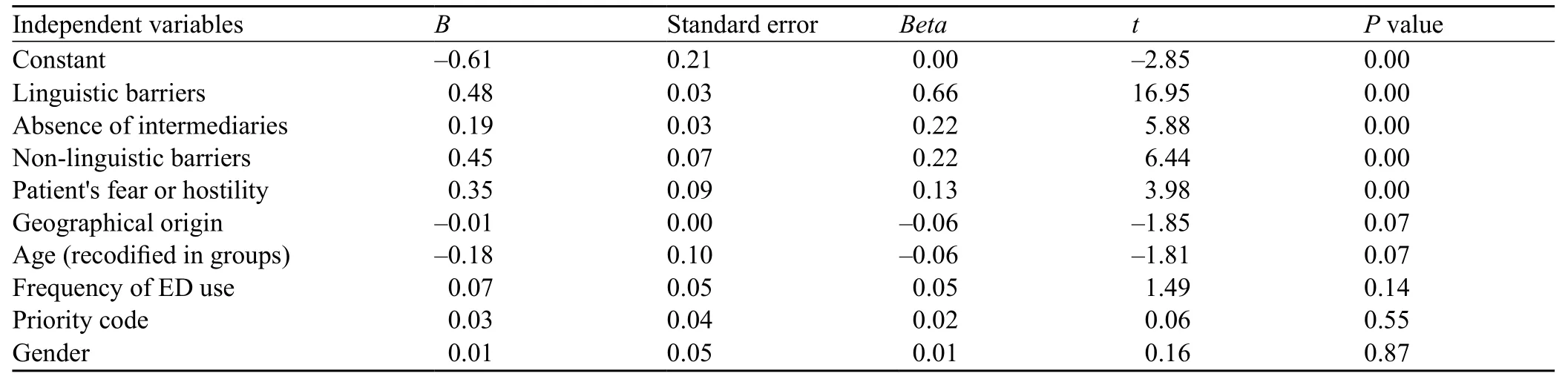
Table 4. Logistic regression analysis for variables potentially related to the level of f nal comprehension
DISCUSSION
This study revealed that significant linguistic barriers exist in nearly one fourth of patients in our institution, and in only half of patients who were able to translate after admission to the ED. The patients with striking linguistic problems come from western Africa and south Europe. It is noteworthy that the vast majority of people living in Italy but coming from south Europe are Albanians, a population that speaks a non-Latin, non Anglo-Saxon language, which represent a challenge for Italian EPs. Linguistic barriers were substantially higher in elderly patients, with difficulties in approximately 58% of patients. A meaningful rate of linguistic problems was also encountered in critically ill patients (43.8%) with a low rate of intermediaries able to translate. However, given the young average age of our patients, we hypothesized that emergencies were often related to professional accidents, with negative external influence (employer, undeclared work). Non-linguistic barriers, although less frequent, play an additional and independent role in worsening the communication between EPs and immigrants, notably in the elderly and those from eastern Africa and south Asia. External inf uences from relatives and work environment represent a further confounding factor, which may frequently amplify the challenges in patient-physician relationship, which is in turn associated with inappropriate use of ED. Hence, in our study habitual and frequent attenders were strongly associated (P<0.01) with non-linguistic barriers (39%), external inf uences (43.5%), and poor or no f nal comprehension of EP's recommendations (16.6%). The average young age and the relatively low frequency of significant linguistic problems (20%) showed that regardless linguistic difficulties, the solution to off was probably more related to the areas of public health and medical care organization in the society.
The f nal level of comprehension of EPs' recommendations was poor or none in a signif cant number of patients (12.4%) although the problem was found to be more pronounced in the elderly (19.4%) and even in critically ill patients (23.3%) with predictable clinical and legal implications. A limit of this study is due to EPs selection bias, but we believe that some groups of immigrants are at a major risk of poor comprehension. The elderly, for example, more often migrate to join their own families, not for work purposes or political issues (e.g., wars, persecutions, etc.). They may be less interested in the integration process, in learning a new language, and in engaging in social affairs or empowering. Patients with high-acuity codes, on the other hand, often present alone to the ED, with the lower presence of intermediaries/translators (32.9%) than the elderly (63.9%) or those with heavy linguistic barriers (54%).
This investigation has three limitations. First, the study is based only on the perception of EPs, without a direct involvement of patients. The most methodological shortcoming is therefore the extrapolation of the subjective perception of a group of doctors to another group of immigrant patients. Second, there is a high risk of bias related to a low response rate (about 15%) and to a possible EPs tendency to experience more diff culties in communication with certain categories of patients, even for personal inclinations. Third, the results are derivedfrom a single institution so that the generalization of our f ndings is questionable.
In conclusion, the present study demonstrates unequivocally that communication difficulties with immigrant patients are a problem strongly felt by emergency physicians, particularly in the elderly and critically ill patients. This could produce dangerous consequences on the serenity (marked aversion in over onethird of the patients with poor final comprehension) and safety of the EPs work, even from a legal point of view.
The priority in emergency services is therefore to improve the communication with different languages. In fact, improving language services might lead to a better utilization of emergency care, while reducing the length of stay in the ED.[28,29]A telephone service of translation, available 24 hours a day, has been implemented in our hospital. For the same purpose, other measures have been taken in this country such as multilingual explanatory leaflets and brochures, the presence of linguistic mediators in the ED and even use of multilingual manuals with colourful pictures.[30]In a constantly growing complexity of western societies, socio-economic conditions, religious beliefs and cultural habits can constitute barriers to the delivery and appropriateness of medical care in the emergency medicine setting.[31]One step toward an improvement of this gap could be the implementation of a cultural competence training for EPs and emergency nurses. In fact, improvement in cultural competence of EPs and ENs can improve personal attitudes towards minority patients and enhance cross-cultural communication.[32]However, cultural competency training is not simple to implement, requiring, as a f rst step, an acknowledgment and respect of cultural practices in different populations, as well as an active work for minimizing the negative effect of cultural differences on the quality and appropriateness of the health care.[32]Moreover, we should recognize that there is a need for a research program for evaluating how cultural competency training can affect patients' satisfaction and outcomes in the ED. Following this way, we will be able to practise and deliver a fair and unbiased emergency medicine.
Funding:None.
Ethical approval:Not needed.
Conflicts of interest:The authors declare that no competing interest and no personal relationships with other people or organizations that could inappropriately inf uence their work.
Contributors:Numeroso F proposed the study and wrote the f rst draft. All authors read and approved the f nal manuscript.
1 United Nations. International migration and development. Report of the Secretary-General United Nations, 2006.
2 Istituto Nazionale di Statistica. Rapporto annuale 2012. La situazione del paese. Available from: http://www.istat.it/it/ f les/2012/05/Rapporto-annuale-2012.pdf (in italian).
3 Norredam M, Nielsen SS, Krasnik A. Migrant's utilization of somatic healthcare services in Europe-a systematic review. Europ J Pub Health 2010; 20: 555–563.
4 Norredam M, Krasnik A, Sorensen TM, Keiding N, Joost Michaelsen J, Sonne Nielsen A. Emergency room utilization in Copenhagen: a comparison of immigrant groups and Danishborn residents. Scand J Public Health 2004; 32: 53–59.
5 Buron A, Cots F, Garcia O, Vall O, Castells X. Hospital emergency department utilisation rates among the immigrant population in Barcelona, Spain. BMC Health Serv Res 2008; 8: 51–60.
6 Rué M, Cabré X, Soler-González J, Bosch A, Almirall M, Serna MC. Emergency hospital services utilization in Lleida (Spain): A cross-sectional study of immigrant and Spanish-born populations BMC Health Services Research 2008; 8: 81–89.
7 Davidovitch N, Filc D, Novack L, Balicer RD. Immigrating to a universal health care system: utilization of hospital services by immigrants in Israel. Health Place 2013; 20: 13–18.
8 Sandvik H, Hunskaar S, Diaz E. Immigrants' use of emergency primary health care in Norway: a registry-based observational study. BMC Health Services Research 2012; 12: 308–319.
9 De Luca G, Ponzo M, Rodríguez Andrés A. Health care utilization by immigrants in Italy. Int J Health Care Finance Econ 2013; 13: 1–31.
10 Zinelli M, Musetti V, Comelli I, Lippi G, Cervellin G. Emergency Department utilization rates and modalities among immigrant population. A 5-years survey in a large Italian urban Emergency Department. Emergency Care Journal 2014; 10: 22–25.
11 Regione Emilia Romagna, Agenzia Sanitaria e Sociale Regionale. "La salute della popolazione immigrata in Emilia Romagna" Dossier 217-2011, ISSN 1591-223X. Available from: http://assr.regione.emilia-romagna.it/it/servizi/pubblicazioni/ dossier/doss217 (in italian).
12 Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR. Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann Intern Med 2003; 139: 907–915.
13 Harmsen H, Bernsen R, Meeuwesen L, Thomas S, Dorrenboom G, Pinto D, et al. The effect of educational intervention on intercultural communication: results of a randomised controlled trial. Br J Gen Pract 2005; 55: 343–350.
14 van Wieringen JC, Harmsen JA, Bruijnzeels MA. Intercultural communication in general practice. Eur J Public Health 2002; 12: 63–68.
15 Flores G. The impact of medical interpreter services on the quality of health care: A systematic review. Med Care Res Rev 2005; 62: 255–299.
16 Lillie-Blanton M, Laveist T. Race/ethnicity, the social environment, and health. Soc Sci Med 1996; 43: 83–91.
17 van Ryn M, Burke J. The effect of patient race and socioeconomic status on physicians' perception of patients. Soc Sci Med 2000; 50: 813–828.
18 Ferguson WJ, Candib LM. Culture, language, and the doctor–patient relationship. Fam Med 2002; 34: 353–361.
19 Ramirez AG. Consumer-provider communication research with special populations. Patient Educ Couns 2003; 50: 51–54.
20 Kiesler DL, Auerbach SM. Integrating measurement of control and aff liation in studies on physician–patient interaction: The interpersonal circumplex. Soc Sci Med 2003; 57: 1707–1722.
21 Saha S, Arbelaez JJ, Cooper LA. Patient–physician relationships and racial disparities in the quality of health care. Am J Public Health 2003; 93: 1713–1719.
22 van Ryn M, Fu SS. Paved with good intentions: Do public health and human service providers contribute to racial/ethnic disparities in health? Am J Public Health 2003; 93: 248–255.
23 Nierkens V, Krumeich A, de Ridder R, van Dongen M. The future of intercultural mediation in Belgium. Patient Educ Couns 2002; 46: 253–259.
24 Kleinman MA. Patients and healers in the context of culture. London: University of California Press; 1980.
25 Ramirez D, Engel KG, Tang TS. Language interpreter utilization in the emergency department setting: a clinical review. J Health Care Poor Underserved 2008; 19: 352–362.
26 Off cial Journal of Italian Republic, n. 76, 31/03/2008: 68–74.
27 United Nations Statistics Division "Composition of macro geographical (continental) regions, geographical sub-regions, and selected economic and other groupings" Available from: http://millenniumindicators.un.org/unsd/methods/m49/m49regin. htm.
28 Mahmoud I, Hou XY, Chu K, Clark M. Language affects length of stay in emergency departments in Queensland public hospitals. World J Emerg Med 2013; 4: 5–9.
29 Mahmoud I, Hou XY, Chu K, Clark M. Language and utilisation of emergency care in Queensland. Emerg Med Australas 2013; 25: 40–45.
30 "Emergency room and immigrants: good practices" An extract from the database of good practices in humanization of Cittadinanza attiva and the Tribunal for Patients' Right from the "Andrea Alesini Prize, 2010". Available from: http://www.scribd. com/doc/47860447/Pronto-soccorso-e-cittadini-migranti-lebuone-pratiche (in Italian).
31 Padela AI, Punekar IR. Emergency medical practice: advancing cultural competence and reducing health care disparities. Acad Emerg Med 2009; 16: 69–75.
32 Beach MC, Price EG, Gary TL, Robinson KA, Gozu A, Palacio A, et al. Cultural competence: a systematic review of health care provider educational interventions. Med Care 2005; 43: 356–373.
Received September 16, 2014
Accepted after revision March 6, 2015
Filippo Numeroso, Email: fnumeroso@ao.pr.it
World J Emerg Med 2015;6(2):111–117
10.5847/wjem.j.1920–8642.2015.02.005
 World journal of emergency medicine2015年2期
World journal of emergency medicine2015年2期
- World journal of emergency medicine的其它文章
- The reliability of the Australasian Triage Scale: a meta-analysis
- Association of low non-invasive near-infrared spectroscopic measurements during initial trauma resuscitation with future development of multiple organ dysfunction
- Assessment of knowledge and attitude about basic life support among dental interns and postgraduate students in Bangalore city, India
- Relationships between genetic polymorphisms of triggering receptor expressed on myeloid cells-1 and septic shock in a Chinese Han population
- B-type natriuretic peptide in predicting the severity of community-acquired pneumonia
- Noninvasive monitoring of intra-abdominal pressure by measuring abdominal wall tension
