Association of low non-invasive near-infrared spectroscopic measurements during initial trauma resuscitation with future development of multiple organ dysfunction
Department of Emergency Medicine, Wake Forest School of Medicine, 2nd Meads Hall, Medical Center Boulevard, Winston Salem, NC 27157, USA
Original Article
Association of low non-invasive near-infrared spectroscopic measurements during initial trauma resuscitation with future development of multiple organ dysfunction
Bret A. Nicks, Kevin M. Campos, William P. Bozeman
Department of Emergency Medicine, Wake Forest School of Medicine, 2nd Meads Hall, Medical Center Boulevard, Winston Salem, NC 27157, USA
BACKGROUND:Near-infrared spectroscopy (NIRS) non-invasively monitors muscle tissue oxygen saturation (StO2). It may provide a continuous noninvasive measurement to identify occult hypoperfusion, guide resuscitation, and predict the development of multiple organ dysfunction (MOD) after severe trauma. We evaluated the correlation between initial StO2and the development of MOD in multi-trauma patients.
METHODS:Patients presenting to our urban, academic, Level I Trauma Center/Emergency Department and meeting standardized trauma-team activation criteria were enrolled in this prospective trial. NIRS monitoring was initiated immediately on arrival with collection of StO2at the thenar eminence and continued up to 24 hours for those admitted to the Trauma Intensive Care Unit (TICU). Standardized resuscitation laboratory measures and clinical evaluation tools were collected. The primary outcome was the association between initial StO2and the development of MOD within the f rst 24 hours based on a MOD score of 6 or greater. Descriptive statistical analyses were performed; numeric means, multivariate regression and rank sum comparisons were utilized. Clinicians were blinded from the StO2values.
RESULTS:Over a 14 month period, 78 patients were enrolled. Mean age was 40.9 years (SD 18.2), 84.4% were male, 76.9% had a blunt trauma mechanism and mean injury severity score (ISS) was 18.5 (SD 12.9). Of the 78 patients, 26 (33.3%) developed MOD within the first 24 hours. The MOD patients had mean initial StO2values of 53.3 (SD 10.3), signif cantly lower than those of non-MOD patients 61.1 (SD 10.0);P=0.002. The mean ISS among MOD patients was 29.9 (SD 11.5), significantly higher than that of non-MODS patients, 12.1 (SD 9.1) (P<0.0001). The mean shock index (SI) among MOD patients was 0.92 (SD 0.28), also signif cantly higher than that of non-MODS patients, 0.73 (SD 0.19) (P=0.0007). Lactate values were not signif cantly different between groups.
CONCLUSION:Non-invasive, continuous StO2near-infrared spectroscopy values during initial trauma resuscitation correlate with the later development of multiple organ dysfunction in this patient population.
Near-infrared spectroscopy; Multiple organ dysfunction; Injury severity score; Shock index; Lactate
INTRODUCTION
Traditional methods for identifying shock states are notoriously insensitive and remain problematic in acute resuscitation of traumatic patients. For example, systemic hypotension is considered a late sign of shock and a poor indicator of systemic hypoperfusion.[1–6]The information gathered from tests of serum lactate and base def cit, even delayed bedside test, can be altered by numerous chronic illness states and regional perfusion abnormalities, or normalized early in shock states.[7]Invasive monitoring of central venous pressure (CVP) and central venous oxygen saturation (SvO2), which is common in intensive care unit (ICU), may not adequately reflect early shock states or influence outcomes beyond directed resuscitation.[8–10]As there is no individual definitive gold standard for the early diagnosis of shock and multiple organ dysfunction, these surrogates frequently serve this purpose in combination.
An ideal monitoring would rapidly, noninvasively and continuously reflect the states of tissue perfusion in a patient, i.e. initial and ongoing assessment of shock, response to therapy and prediction of multiple organ dysfunction (MOD). Near-infrared spectroscope (NIRS), a non-invasive monitor of muscle tissue oxygen saturation (StO2) using infrared light absorption, has been studied in many traumatic and surgical patients. Recent studies[11–16]have asserted that StO2normalization is associated with improved outcomes during resuscitation of patients in hemorrhagic shock. In this study, we prospectively assessed the monitoring of StO2in the resuscitation period to predict the development of MOD, further validating previous studies in a large sample of trauma patients.[19,20]We also analyzed the association of StO2measurements with lactate and shock indexes of the predef ned trauma patients.
METHODS
Study design
This prospective, observational, nonrandomized cohort study was conducted at a Level I trauma center with an annual emergency department (ED) volume of 92 000 patients and an average of over 900 trauma alert patients per year. The study went through a 15 month period between April 2005 and July 2006.
Inclusion criteria
Included were adult patients aged 18 years or over who arrived at the emergency department within 3 hours of traumatic injury and met the standardized trauma team activation criteria (Table 1).
Exclusion criteria
Figure 1 shows a complete list of exclusion criteria. Excluded patients included those known to be pregnant, those with known “Do Not Resuscitate” order, and those requiring isolation of both hands for forensic gunshot residue testing. In addition, patients with bilateral upper extremity fractures or absence of adequatetissue remaining over the thenar eminence were also excluded because of the inherent interference with StO2measurement. Additional exclusion criteria were related to logistical issues related to device availability and continuous data acquisition.
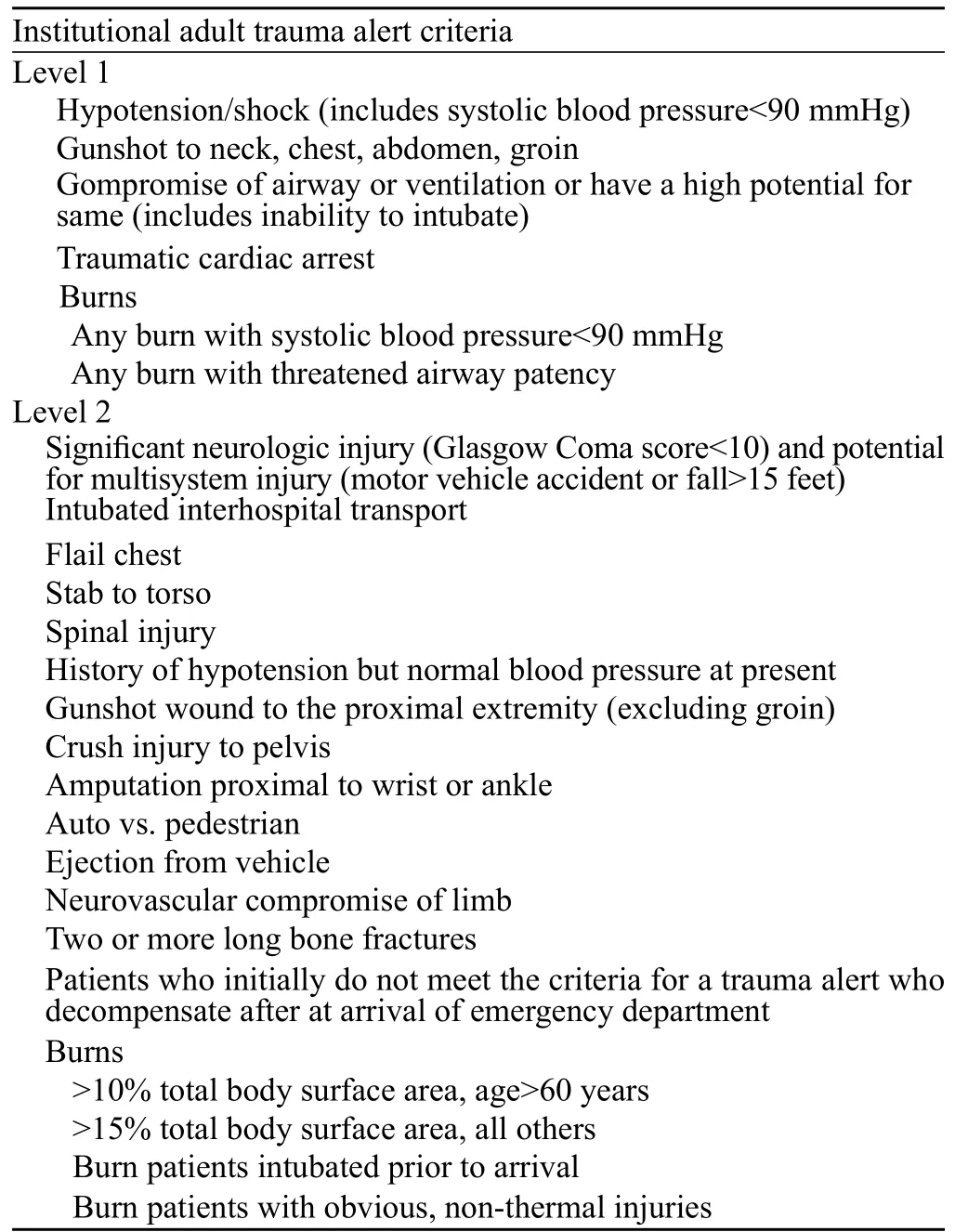
Table 1. Institutional trauma alert criteria
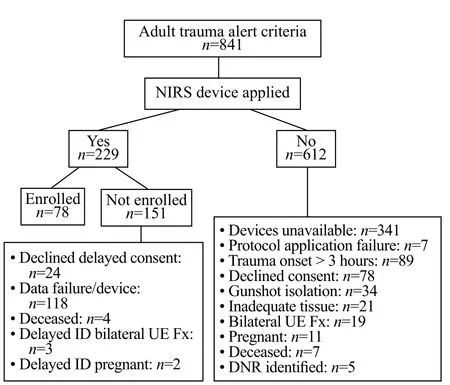
Figure 1. Patient enrollment.
Experimental device
NIRS-derived StO2was measured using the T.Ox™Tissue Oximeter (ViOptix Inc, Fremont, Ca) which was applied to each patient through a small adhesive sensor attached to the thenar eminence of an uninjured upper extremity.
Protocol
The StO2monitor was placed upon the arrival of trauma patients to the ED/Trauma Center. The study protocol was reviewed and approved by the institutional review board (IRB). Because of the minimal risk of the non-invasive monitoring device and the critical nature of trauma resuscitations, permission was granted by the IRB to routinely place the noninvasive NIRS monitoring device upon the arrival of all trauma alert patients. Informed consent to participate in the study and allow record abstraction was obtained from all participants during their ED or hospital stay.
StO2values were automatically recorded by the NIRS device. The lowest value during the initial 5 minutes of sampling was used as the initial value, and hourly timeaveraged values were used thereafter. The device remained in place on all patients admitted to the trauma ICU for 24 hours. For those patients admitted to a non-ICU bed, discharged, or deceased, the monitor was removed after completion of the ED care course. StO2values were not made available to the clinical team during patient care, and therefore had no impact on the usual care provided.
Data collected by the research staff included demographic information, date, time, mechanism/ cause, referral hospital information, prehospital interventions including vital signs, intravenous fluids (IVF) and procedures, and initial assessment on ED arrival. Our standardized trauma protocol includes performance of vital signs at least every 10 minutes for the first 60 minutes of resuscitation and the following standardized trauma labs: complete blood count (CBC), comprehensive metabolic profile (CMP), coagulation profile with international normalized ratio (INR), serum lactate, arterial blood gas (ABG), and urine drug screening (UDS). All intravenous fluids and blood products administered were recorded.
Repeat labs were obtained from patients admitted to the ICU and to the floor as needed for clinical management by the trauma team. Invasive monitoring was done in the ICU in terms of central venous pressure, SvO2, pulmonary capillary wedge pressure, cardiac indices, systemic vascular resistance, oxygen consumption, and oxygen delivery. Clinical values and final injury severity score (ISS) were collected and entered the secure database.
There are a number of scoring systems that have been used to describe organ dysfunction and failure in critically ill and injured patients. The Marshall Score or multiple organ dysfunction (MOD) score has been extensively used in injured patients (Table 2).[10,19,21-27]Given that initial MOD calculations would reflect the traumatic injury and not subsequently prolong organ dysfunction, MOD occurred 72 hours later. The MOD score was not summation score, but rather daily score obtained up to 7 days of hospitalization, a duration commonly used in the recent literature to account for prolonged organ dysfunction after trauma. A P value less than 0.05 was considered statistically signif cant for all tests.
Analysis
This study was designed to determine the statistical significance (P<0.05) of StO2for MOD based on the incidence of 14%–42% (MOD score 6 or greater excluding GCS) in high-risk trauma patients with multiple organ failure.[17]Calculations of the error rate and power required that 26 MOD patients be enrolled in the study. The patients were grouped by the presence or absence of MOD, and initial serum lactate values were classif ed into no shock (lactate <2 mmol/L), mild shock (lactate 2–4 mmol/L), and moderate/severe shock (lactate>4 mmol/L) groups.[28,29]Shock index, the ratio of pulse to systolic blood pressure, was categorized as normal (<1.0) or abnormal (≥1.0).[30,31]
Multivariate regression and rank-sum comparison were used to compare the groups (InStat v 3.0, GraphPad Software, La Jolla, CA, USA). Regression analyses were done initially with NIRS values as the dependentvariables, tested against the values of lactate and shock index as independent variables. They were then performed with each of the independent variables tested against the other. The primary outcome was the measurement of the association between initial StO2and the development of MOD. Secondary outcomes included the association between StO2values, serum lactate, and shock index calculations used during initial trauma resuscitation.

Table 2. Multiple organ dysfunction (Marshall) score
RESULTS
In the period of study, 841 adults had trauma activations. Of these patients, 229 had the NIRS device placed during trauma activations from which 78 patients completed the enrollment process (Figure 1). Their mean age was 40.9 years (SD 18.2) and 84.6% of the patients were male. Of these patients, 79% had a blunt trauma. The mean injury severity score (ISS) of all the patients was 18.3 (SD 9.9).
Twenty-six of the 78 (33.3%) patients developed MOD after the first 72 hours (Table 3). The mean ISS in MOD patients was 29.9 (SD 11.5), which was signif cantly higher than that in non-MOD patients, 12.1 (SD 9.1; P<0.0001). The mean initial StO2value (53.3; SD 10.3) was significantly lower in the MOD patients than in the non-MOD patients (61.1; SD 10.0) (P=0.002). The mean shock index (SI) in the MOD patients was 0.92 (SD 0.28), which was also signif cantly higher than that in the non-MOD patients (0.73; SD 0.19) (P=0.0007). Lactate values were not significantly different between the two groups (P=0.168).
Comparison of the inclusion and exclusion populations demonstrated that the study had a representative sample of your trauma population (Table 4). Male patients in the excluded population were less than 81% compared to 85%, but this was not statistically significant. Also, ISS, shock index and lactates were slightly higher in theexcluded group but this observation was not statistically signif cant. There was no signif cant difference in mode of arrival or level of trauma activation.

Table 3. Demographic information and measures of shock in the study population
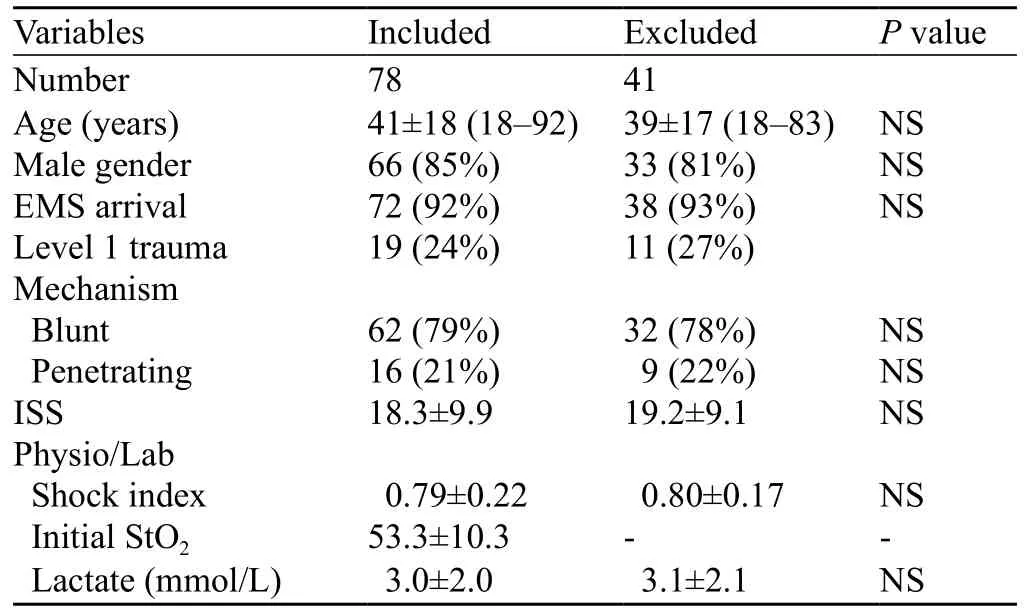
Table 4. Demographic comparison of the included and excluded populations
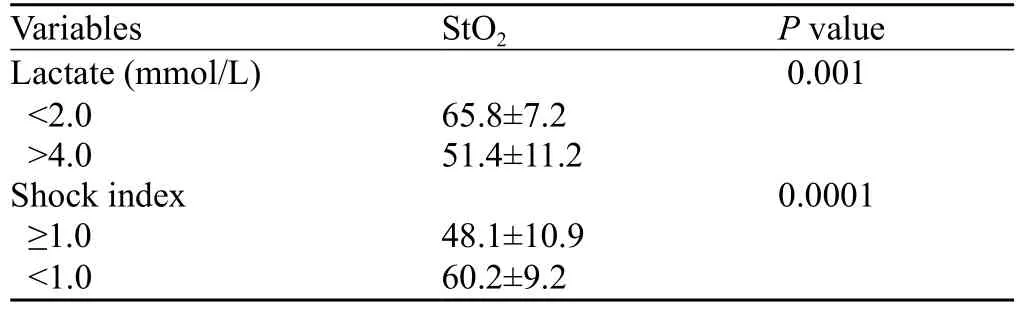
Table 5. NIRS associations with lactates and shock index
NIRS values discriminated between those with moderate-severe shock (lactates>4 mmol/L, n=21) on arrival and those without shock (lactate<2, n=34) with mean StO2values of 51.4 (SD 11.2) vs. 65.8 (SD 7.2), respectively (P<0.001). NIRS was unable to discriminate those with mild shock defined by mid-range (2.0–4.0 mmol/L) lactates (P>0.05). However, NIRS was able to distinguish those with an abnormal shock index (≥1.0) from those with a normal SI (<1.0), with mean StO2values of 48.1 (SD 10.9) vs. 60.2 (SD 9.2), respectively (P<0.0001) (Table 5).
DISCUSSION
The traditional methods for identifying and monitoring shock vary, and it is accepted that monitoring a patient's response to ongoing resuscitation efforts, or lack thereof, is essential. Patients may remain inadequately or be under-resuscitated despite normalizing blood pressure measurements, leading to persistent hypoperfusion and tissue ischemia with the development of multiple organ dysfunction (MOD) syndrome and the resultant increase of morbidity and mortality.[10]
StO2values were evaluated as a marker of resuscitation and a method of identifying a cohort of patients potentiallyat risk for developing multiple organ dysfunction or being predictive of death.[11–20]In most circumstances, the values were not initiated at the immediate point of care in the ED but within 60 minutes after arrival. In this study, the patient population included all patients that met the established trauma criteria (Table 1), and monitoring began at the point of arrival at the ED which allows for better data correlation in the acute resuscitation period and potentially great decrease of predictive capabilities.
The StO2minimum value during the first 60 minutes of resuscitation has been used as the predictive measurement for subsequent adverse effects.[17–20]Also, as the different devices used for StO2assessment can obtain varied samples over time, a time-average value for trend assessments is frequently predef ned for each study.
Since initial MOD calculations would ref ect traumatic injury and not subsequent prolonged organ dysfunction, MOD was calculated after the initial 72 hours.[24–27]We also modified the MOD score to exclude GCS because of the bias of possible underlying brain injury in trauma. The MOD score was not summation scoring, but rather daily scores obtained up to 7 days of hospitalization. This approach remains consistent with previous analyses showing the delayed effects of multi-organ failure due to trauma.[28]
Impaired cellular oxygen utilization has been recognized as potential evidence for the development of multiple organ dysfunction.[9]Additional small studies[13,14]have identif ed StO2values of skeletal muscle as a consistent measurable indicator of resuscitation status. Further studies[19,20]identif ed the thenar eminence as a more reproducible location for tissue oximetry measurement regardless of the StO2device utilized. In addition, values have been established for determination of severe shock from non-severe shock state.[19,20,27]However, data acquisition and the associated trend values are far more predictive of persistent shock state, but may be more predictive of the development of MOD.[29–31]
Cohn et al[19]found that StO2was useful in discriminating patients who would later develop MOD after major trauma from those who would not. As the study differred in the onset time and duration of monitoring, the underlying data were supportive of the same results. Similarly, a pre-hospital model identified the decreasing tissue oximetry levels associated with in-hospital life-saving interventions.[32]
LIMITATIONS
This observational study has several limitations. As a pilot study of feasibility regarding immediate NIRS device placement under a pre-existent standardized trauma protocol, the study was not able to explicitly predict those who will develop MOD. In addition, the study was limited by the number of devices available for the enrollment process, and convenient sampling was based on the availability of NIRS monitors and study staff. However, the enrollment did have a representative sample of the entire trauma population. Numerous patients were excluded from the study because of powering down of the device and absence of continuous StO2measurements during the period of resuscitation. Possibly, the second limitation was due to the small number of enrolled patients and those with MOD. Moreover, there was enrollment bias induced by clinicians who were familiar with the device and the study. We also did not investigate the trends in StO2measurements over time and their relationship to events occurring in the ICU setting, but the lowest values in the initial resuscitation and subsequent patient outcomes. In addition, this study was not able to detect StO2differences between mild- and moderate-severe shock.
In conclusion, we found that non-invasive, continuous StO2near-infrared spectroscopy values during initial trauma resuscitation correlate with subsequent development of multiple organ failure and also with shock index in the acute resuscitation of multi-trauma patients. NIRS can also discriminate between those with no and moderate-severe shock as determined by intermittent invasive serum lactate test.
As a continuous non-invasive measure of hypoperfusion, we believe that StO2values may provide further objective data to overcome the existing limitations of traditional assessments of hypoperfusion and shock. In addition, as an early indicator of hypoperfusion, StO2measurement may assist with not only dynamic resuscitation guidance, but with early identif cation of post-resuscitation decline with the potential to assuage recurrent hypoperfusion in all modalities of shock.
Further studies are warranted to ascertain the validity of these findings, with an emphasis on non-invasive predictive modeling, impact of early intervention from trending data, and outcome measures including the length of ICU stay, morbidity/mortality, and cost savings. Expansion into the pre-hospital setting, especially for regions with extended transport durations for trauma patients, may prove useful in guiding outcome-based resuscitation protocols within trauma systems.
Funding:None.
Ethical approval:The study protocol was reviewed and approved by the Institutional Review Board (IRB).
Conf icts of interest:The authors declare that there is no conf ict of interest.
Contributors:Nicks BA proposed the study. All authors contributed to the design and interpretation of the study, and approved the f nal manuscript.
1 Parks JK, Elliott AC, Gentilello LM, Shafi S. Systemic hypotension is a late marker of shock after trauma: a validation study of Advanced Trauma Life Support principles in a large national sample. Am J Surg 2006; 192: 727–731.
2 Millham FH, LaMorte WW. Factors associated with mortality in trauma: re-evaulation of the TRISS method using the National Trauma Data Bank. J Trauma 2004; 56: 1090–1096.
3 Vassar MJ, Lewis FR Jr, Chambers JA, Mullins RJ, O'Brien PE, Weigelt JA, et al. Prediction of outcome in intensive care unit trauma patients: a multicenter study of Acute Physiology and Chronic Health Evaluation (APACHE), Trauma and Injury Severity Score (TRISS), and a 24-hour intensive care unit (ICU) point system. J Trauma 1999; 47: 324–329.
4 Gando S, Nanzaki S, Kemmotsu O. Disseminated intravascular coagulation and sustained systemic inflammatory response syndrome predict organ dysfunctions after trauma: application of clinical decision analysis. Ann Surg 1999; 229: 121–127.
5 Graham CA, Parke TR. Critical care in the emergency department: shock and circulatory support. Emerg Med J 2005; 22: 17–21.
6 Siegel JH, Fabian M, Smith JA, Kingston EP, Steele KA, Wells MR, et al. Oxygen debt criteria quantify the effectiveness of early partial resuscitation after hypovolemic hemorrhagic shock. J Trauma 2003; 54: 862–880.
7 Tuhay G, Pein MC, Masevicius FD, Kutscherauer DO, Dubin A. Severe hyperlactatemia with normal base excess: a quantitative analysis using conventional and Stewart approaches. Crit Care 2008; 12: R66.
8 Puyana JC, Pinsky MR. Searching for non-invasive markers of tissue hypoxia. Crit Care 2007; 11: R6.
9 The ProCESS Investigators. A Randomized Trial of Protocol-Based Care for Early Septic Shock. N Engl J Med 2014; 370: 1683–1693.
10 Marshall JC, Cook DJ, Christou NV, Bernard GR, Sprung CL, Sibbald WJ. Multiple organ dysfunction score: a reliable descriptor of a complex clinical outcome. Crit Care Med 1995; 23: 1638–1652.
11 Hirano Y, Omura K, Yoshiba H, Ohta N, Hiranuma C, Nitta K, et al. Near-infrared spectroscopy for assessment of tissue oxygen saturation of transplanted jejuna autografts in cervical esophageal reconstruction. Surg Today 2005; 35: 67–72.
12 Rapez A, Oroszy D, Amez ZM. Continuous postoperative monitoring of cutaneous free flaps using near infrared spectroscopy. J Plast Reconstr Aesthet Surg 2008; 61: 71–77.
13 Arbabi S, Brundage SI, Gentilello LM. Near-infrared spectroscopy: a potential method for continuous, trancutaneous monitoring for compartmental syndrome in critically injured patients. J Trauma 1999; 47: 829–833.
14 Creteur J. Muscle StO2in critically ill patients. Curr Opin Crit Care 2008; 14: 361–366.
15 Uilkema RJ, Groeneveld AB. Correlates of thenar near-infrared spectroscopy-derived tissue O2saturation after cardiac surgery. Interact Cardiovasc Thorac Surg 2007; 6: 265–269.
16 Ikossi DG, Knudson MM, Morabito DJ, Cohen MJ, Wan JJ, Khaw L, et al. Continuous muscle tissue oxygenation in critically injured patients: a prospective observational study. J Trauma 2006; 61: 780–788.
17 Cohn SM, Crookes BA, Procter KG. Near-infrared spectroscopy in resuscitation. J Trauma 2003; 54: S199–S202.
18 Smith J, Bricker S, Putnam B. Tissue oxygen saturation predicts the need for early blood transfusion in trauma patients. Am Surg 2008; 74: 1006–1011.
19 Cohn SM, Nathens AB, Moore FA, Rhee P, Puyana JC, Moore EE, et al. Tissue oxygen saturation predicts development of organ dysfunction during traumatic shock resuscitation. J Trauma 2007; 62: 44–55.
20 Crookes BA, Cohn SM, Bloch S, Amortegui J, Manning R, Li P, et al. Can near-infrared spectroscopy identify the severity of shock in trauma patients? J Trauma 2005; 58: 806–813.
21 Miner J, Nelson R, Hayden L. The effect of near infrared spectroscopy monitoring on the treatment of patients presenting to the emergency department in shock. Crit Care Med 2010; 38: S861.
22 Lima A, van Bommel J, Jansen TC, Ince C, Bakker J. Low tissue oxygen saturation at the end of early goal-directed therapy is associated with worse outcome in critically ill patients. Crit Care 2009; 13 Suppl 5: S13.
23 Iyegha UP, Conway T, Pokorney K, Mulier KE, Nelson TR, Beilman GJ. Low StO2measurement in surgical intensive care unit patients is associated with poor outcomes. J Trauma Acute Care Surg 2014; 76: 809–816.
24 Jeger V, Jakob SM, Fontana S, Wolf M, Zimmermann H, Exadaktylos AK. 500 ml of blood loss does not decrease noninvasive tissue oxygen saturation (StO2) as measured by near infrared spectroscopy – A hypothesis generating pilot study in healthy adult women. J Trauma Manag Outcomes 2010; 4: 5.
25 Marshall JC. Organ dysfunction as a measure of outcome in clinical trials. Eur J Surg Suppl 1999; 584: 62–67.
26 Buckley TA, Gomersall CD, Ramsay SJ. Validation of the multiple organ dysfunction (MOD) score in critically ill medical and surgical patients. Intensive Care Med 2003; 29: 2216–2222. 27 Ulvik A, Kvåle R, Wentzel-Larsen T, Flaatten H. Multiple organ failure after trauma affects even long-term survival and functional status. Crit Care 2007; 11: R95.
28 Santora RJ, Moore FA. Monitoring trauma and intensive care unit resuscitation with tissue hemoglobin oxygen saturation. Crit Care 2009; 13 Suppl 5: S10. Epub 2009 Nov 30.
29 Paladino L, Sinert R, Wallace D, Anderson T, Yadav K, Zehtabchi S. The utility of base deficit and arterial lactate in differentiating major from minor injury in trauma patients with normal vital signs. Resuscitation 2008; 77: 363–368.
30 Callaway DW, Shapiro NI, Donnino MW, Baker C, Rosen CL. Serum lactate and base def cit as predictors of mortality in normotensive elderly blunt trauma patients. J Trauma 2009; 66: 1040–1044.
31 Beekley AC, Martin MJ, Nelson T, Grathwohl KW, Griff th M, Beilman G, et al. Continuous noninvasive tissue oximetry in the early evaluation of the combat casualty: a prospective study. J Trauma 2010; 69 Suppl 1: S14–25.
32 Guyette FX, Gomez H, Suffoletto B, Quintero J, Mesquida J, Kim HK, et al. Prehospital dynamic tissue oxygen saturation response predicts in-hospital lifesaving interventions in trauma patients. J Trauma Acute Care Surg 2012; 72: 930–935.
Received August 9, 2014
Accepted after revision January 28, 2015
Bret A. Nicks, Email: bnicks@wakehealth.edu
World J Emerg Med 2015;6(2):105–110
10.5847/wjem.j.1920–8642.2015.02.004
 World journal of emergency medicine2015年2期
World journal of emergency medicine2015年2期
- World journal of emergency medicine的其它文章
- Progress in research into the genes associated with venous thromboembolism
- Advances in clinical studies of cardiopulmonary resuscitation
- Instructions for Authors
- Thrombolysis during extended cardiopulmonary resuscitation for autoimmune-related pulmonary embolism
- Effect of sedation on short-term and long-term outcomes of critically ill patients with acute respiratory insuff ciency
- Eff cacy of fascia iliaca compartment nerve block as part of multimodal analgesia after surgery for femoral bone fracture
