Redo Coronary Artery Bypass Grafting: On-Pump and Off-Pump Coronary Artery Bypass Grafting Revascularization Techniques
Department of Cardiac Surgery, Peking University Third Hospital, Beijing 100191, China
Redo Coronary Artery Bypass Grafting: On-Pump and Off-Pump Coronary Artery Bypass Grafting Revascularization Techniques
Song Wu*, Feng Wan, Zhe Zhang, Hong Zhao, Zhong-qi Cui, and Ji-yan Xie
Department of Cardiac Surgery, Peking University Third Hospital, Beijing 100191, China
reoperation; coronary artery bypass grafting; on pump; off pump; transmyocardial laser revascularization
ObjectiveTo analyze the short-term outcomes of redo coronary artery bypass grafting (CABG) using on-pump and off-pump CABG techniques.
MethodsFrom January 2003 to August 2013, non-randomized 80 patients were treated with redo CABG in the Department of Cardiac Surgery, Peking University Third Hospital. Among these patients, 40 underwent on-pump CABG technique (redo-ONCAB group) and 40 underwent off-pump CABG technique (redo-OPCAB group). Furthermore, transmyocardial laser revascularization was performed in high-risk patients who were not suitable to conventional grafting. Clinical data of the two groups were recorded and analyzed including operation time, coronary grafts, incomplete revascularization, postoperative ventilation, perioperative stroke, and low output syndrome, etc.
ResultsThere were no significantly differences in age, gender distribution, incidences of hypertension, stroke, and other clinical characteristics between redo-OPCAB group and redo-ONCAB group (all p>0.05), except for incidences of renal dysfunction and pulmonary disease (all p<0.05). The number of grafting vessels in the redo-ONCAB and redo-OPCAB groups was 2.1 ± 0.74 and 1.4 ±0.52 respectively. There was significant difference between the two groups (p=0.0243). Compared with the redo-ONCAB group, there was shorter operation time (p=0.0045), postoperative ventilation (p=0.0211) and intensive care unit stay (p=0.0400), as well as fewer use of platelet (p=0.0338) and blood transfusion (p=0.0034) in the redo-OPCAB group. The incidence of incomplete revascularization (p=0.0253) and the use of transmyocardial laser revascularization (p=0.0052) were higher in the redo-OPCAB group than those in the redo-ONCAB group (all p<0.05). However, no significant differences were showed for the incidence of the use of intra aortic balloon pump and continuous renal replacement therapy, perioperative stroke, low output syndrome, and in-hospital mortality between the two groups (all p>0.05).
ConclusionRedo CABG is the safety and efficacy surgical procedure, and redo-OPCAB technique with better outcomes is commended especially in high-risk patients.
Chin Med Sci J 2015; 30(1):28-33
IN China, redo coronary artery bypass grafting (redo CABG) has gradually increased over the years. Morbidity and mortality associated with redo CABG are higher than those for first-time CABG.1-3The benefits of off-pump CABG (OPCAB) have been demonstrated, yet the application of beating heart surgery for redo CABG remains limited because of safety concerns, technical challenges, and the higher incomplete revascularization rate.4-9The surgery strategies of redo CABG have been developed in our hospital since 2003. In this study, we retrospectively analyzed the short-term outcomes of redo CABG by either on-pump CABG (ONCAB) or OPCAB in non-randomized patients.
PATIENTS AND METHODS
Patient selection
From January 2003 to August 2013, 80 patients were treated with redo CABG in the Department of Cardiac Surgery, Peking University Third Hospital. The mean duration from the first CABG to redo CABG was 12±5 years. Among these patients, 40 patients underwent ONCAB (redo-ONCAB group) and 40 patients underwent OPCAB (redo-OPCAB group). The exclusion criteria were: CABG combined with cardiac valve or ventricular surgery; those who had combined with major vascular surgery. OPCAB was primarily performed in cases that the ascending aorta was not suitable for proximal anastomosis or clamp (for example, porcelain ascending aorta) and cases with a high risk of organ dysfunction after operation. The final decision of procedure depended on the surgeon expert responsible for the operation. Furthermore, transmyocardial laser revascularization (TMLR) was performed in high-risk patients with poor vessel quality and diffuse distal diseases which were not suitable to conventional grafting in order to promote blood flow. All patients underwent open surgery using median sternotomy for the previous surgery. These operations were performed by the same surgeon.
Surgical technique for redo ONCAB
All operations were performed under general anesthesia. Redo sternotomy was performed using an oscillating saw. After completing the dissection around the heart, the standard ONCAB technique was applied.10Procedures of the redo ONCAB were performed using standard cardiopulmonary bypass (CPB), which was established by using ascending aortic and two-stage venous cannulation. Redo ONCAB is a beating heart procedure without clamping the aorta or hypothermia.
Surgical technique for redo OPCAB
After completing the dissection around the heart, a standard OPCAB technique was applied.11A cardiac stabilizer (MEDOS, China) was used for the distal anastamosis, and an Enclose II manual proximal anastomotic device (Surgical Systems, Inc., CA, USA) was used for the proximal anastomosis. If the redo OPCAB procedure was switched to beating redo ONCAB, the distal and proximal anastomoses were also completed except that standard CPB was installed.
Surgical technique for TMLR
When CABG technique was finished, TMLR was performed in the target areas of the left ventricle which are not suitable to conventional grafting. Multiple transmural channels of 1 mm in diameter were created individually by high energy CO2laser (PLC Medical Systems, Inc., MA, USA) in the posterolateral wall of the left ventricle. Transmural penetration by the laser was confirmed by transesophageal echocardiography. Bleeding from the channels was stopped with external pressure.12,13
Data collection
Patients data in the redo-ONCAB group and redo-OPCAB group were recorded and analyzed by comparing various preoperative, perioperative, and postoperative parameters, including operation time, coronary grafts, incomplete revascularization, postoperative ventilation, perioperative stroke, low output syndrome, blood transfusion requirement, intensive care duration, and in-hospital mortality.
Statistical analysis
Statistical analysis was performed using the SAS 9.1 software (SAS Institute, Cary, NC, USA). Continuous variables were expressed as mean ± standard deviation (SD) and categorical variables as frequency or percentage. Continuous variables of inter-group were compared using Student’s t test. Categorical variables were compared using χ2or Fisher’s exact test. P<0.05 was considered statistically significant.
RESULTS
Baseline characteristics
The preoperative demographic data of the two groups are showed in Table 1. There were no significantly differences in incidence of previous mitral insufficiency, atrial fibrillation rhythm, peripheral vascular disease, hypertension, hypercholesterolaemia, smoking, stroke and diabetes mellitus between the two groups (all P>0.05), but the incidences ofrenal dysfunction and pulmonary disease were higher in the redo-OPCAB group than those in the redo-ONCAB group (P=0.0180 and 0.0284). (Table 1)
Comparison of perioperative and postoperative clinical data
The operation time was significantly shorter in the redo-OPCAB group (P=0.0045). The number of vessels of CABG in the redo-ONCAB group was significantly less than that in the redo-OPCAB group (P=0.0243). Compared with the redo-ONCAB group, there were shorter postoperative ventilation (P=0.0211) and intensive care unit stay (P= 0.0400), as well as fewer use of platelet (P=0.0338) and blood transfusion (P=0.0034) in the redo-OPCAB group. Another significant differences were the higher incidence of incomplete revascularization (P=0.0253) and the use of TLMR (P=0.0052) in the redo-OPCAB group. However, no significant differences were showed for the incidence of the use of continuous renal replacement therapy and intra aortic balloon pump, perioperative stroke, low output syndrome, and in-hospital mortality between the two groups (all P>0.05). (Table 2)

Table 1.Comparison of preoperative characteristics between redo-ONCAB and redo-OPCAB groups (n=40)
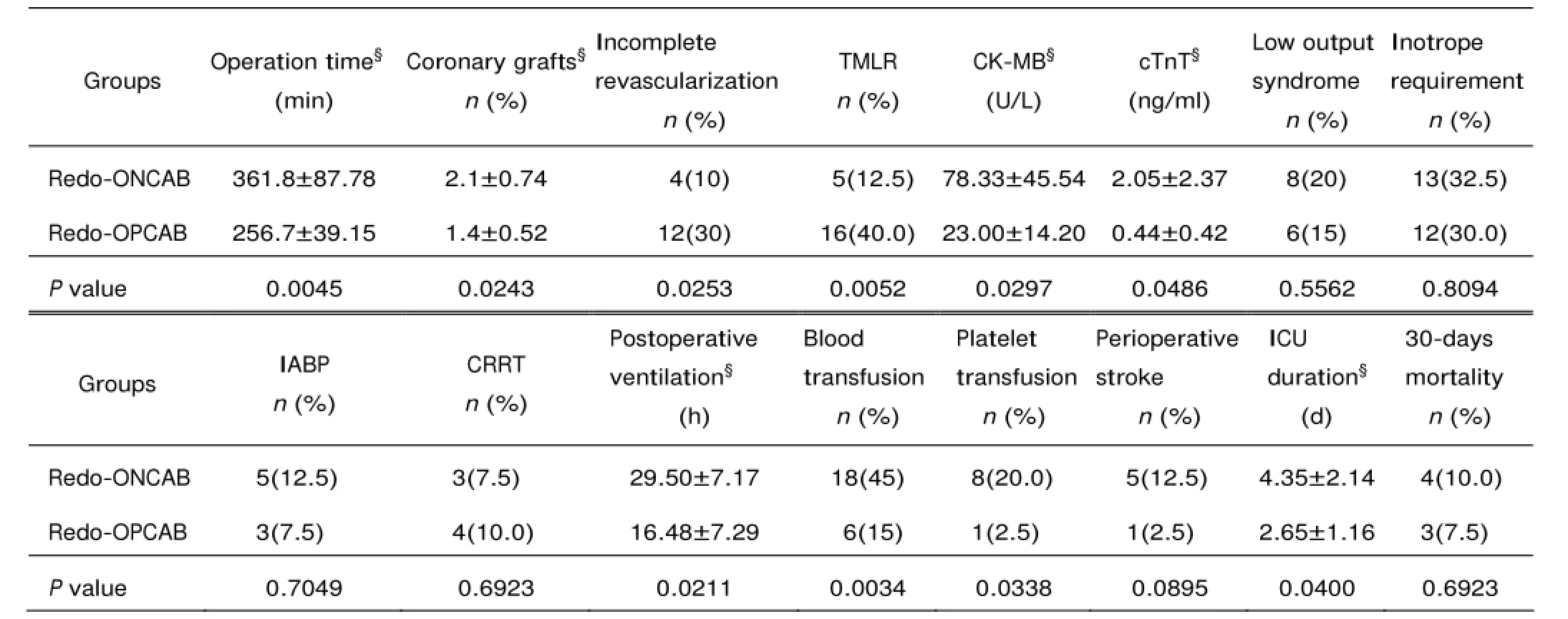
Table 2.Comparison of postoperative characteristics between redo-OPCAB and redo-ONCAB groups (n=40)
DISCUSSION
Redo CABG provides several technical challenges that distinguish it from conventional CABG. The benefits of OPCAB have been demonstrated, yet the application of beating heart surgery to redo CABG remains limited because of safety concerns, technical challenges and the higher incomplete revascularization rate, especially in highrisk patients with poor vessel quality and diffuse distal disease. Another drawback of this technique is the hemodynamic deterioration which can occur in manipulation of the heart during surgery. Conventional non-beating heart ONCAB is still the standard technique used in coronary artery surgery in many hospitals and believed to help to acquire complete revascularization. Complications in relation to this technique are due to the release of inflammatory mediators, the use of cardioplegia, aortic cross clamping, and hypothermia. Blood contact with the artificial surfaces of the CPB circuit produces a well-documented diffuse inflammatory response which affects multiple organ systems. Virtually all detrimental effects of this diffuse inflammatory response are associated with long duration of CPB.14Considering the above mentioned reasons, we established the surgical strategy for redo CABG in our cardiac center. The major indications for redo OPCAB were cases in which the ascending aorta was not suitable for proximal anastomosis or clamp and cases with a high risk of postoperative organ dysfunction (such as kidney insufficiency or lung insufficiency). Some high-risk patients with poor vessel quality and diffuse distal disease adopted redo OPCAB combined with TMLR (redo-OPCAB+TMLR). As for other cases, the standard ONCAB technique was applied without clamping the aorta and without hypothermia. This technique can not only avoid some complications in relation with the use of cardioplegia, aortic cross clamping, and hypothermia of CPB, but also it may achieve complete revascularization and lower difficulty of operation. Allen et al10,15reported that an important criticism of off-pump (beating heart) operation focuses on the accuracy of anastomosis compared with OPCAB.
According to our present retrospective study, we confirmed the safety and efficacy for both surgical procedures of redo CABG, and the redo OPCAB technique with better outcomes was applied especially in high-risk patients. Our results indicated that redo OPCAB patients had shorter operation time, less postoperative blood loss, shorter postoperative ventilation, and intensive care unit stay.
Stroke is a devastating complication that increases mortality, morbidity, hospital stay and cost. Although there was no statistically significant difference in perioperative stroke between the two groups, the incidence of perioperative stroke in the redo-ONCAB group was higher than that in the redo-OPCAB group in this study (P=0.0895). In the redo-OPCAB group, we performed an aortic no-touch procedure, in which there was no surgical manipulation of the ascending aorta compared with the standard CABG. Patients received vein grafts with an anastomosis assist device, Enclose II. Completely avoidance of “side-biting” clamps in redo OPCAB could reduce the incidence of neurological complications in the case of severe atheromatous aortas occurred frequently in elderly patients. The more applications of no-touch technique to avoid any manipulation of atheromatous and calcified ascending aortas, the stroke rate appeared lower in the redo-OPCAB group. Furthermore, among patients receiving transfusions, there were fewer different blood products administered in the redo-OPCAB group compared with the redo-ONCAB group. Transfusion of blood products after CABG has a strong, dose-dependent association with the risk of stroke. The use of platelet transfusions seems to have an even stronger impact on the development of stroke than red blood cell transfusions.16
Acute renal failure (ARF) after cardiac surgery has been clearly associated with higher mortality rate in the early postoperative period.17In most cases, ARF is not the single complication following cardiac surgery and is associated either with inflammatory response (systemic inflammatory response syndrome, especially sepsis or septic shock) or cardiogenic dysfunction combined with diuretic drug resistance.18It is known that the CPB and pulmonarymyocardial reperfusion activate the innate and adaptive immune systems. The extent of this immune reaction has been linked to postoperative complications also occurred in redo CABG.19Therefore, the avoidance of CPB and subsequent myocardial ischemia reperfusion has been proposed in order to greatly reduce postoperative complications, such as renal dysfunction.20In 2005, continuous renal replacement therapy (CRRH) was regarded as the preferred therapeutic strategy for all patients who would develop ARF with diuretic drug resistance and cardiogenic shock after cardiac surgery. In this study, the incidence of preoperative renal insufficiency in the redo-OPCAB group (22.5%) was higher than that in the redo-ONCAB group (2.5%), while the rate of renal failure requiring postoperative CRRH was similar between the two groups (10.0% versus 7.5%, P=0.6923).
OPCAB has also been shown to lead to better recoveryof myocardial oxidative metabolism, myocardial function, and a lower requirement for inotropic agents.21,22In this study, we found that the level of cardiac troponin T was higher in the redo ONCAB group than that in the redo-OPCAB group, which reflected the greater heart trauma associated with redo ONCAB. It was also found that the need for installation of intra aortic balloon pump was higher in the redo-ONCAB group than that in the redo-OPCAB group after operation, which may be associated with reduced cardiac contractility as a result of myocardial edema secondary to global ischaemia and greater reperfusion injury after redo ONCAB.
在玉米播种的过程中,必须要选择紧凑型的品种,并且要保证每亩用量为2.5kg,每公顷保苗6.0-6.5万株,在播种期间应该要保证更曾在5-10cm左右,并且低温温度恒定在六至7℃,所以最佳的播种期应该是在4月下旬或5月上旬左右,在播种时可以利用人工刨煤种,以及机械播种的方法,尽量保证一次全苗播种,播种时必须要做到深浅一致。
In this study, the efficacy of TMLR was also evaluated, which as an adjunct to CABG in some patients who had distal, diffuse coronary artery disease and not amenable to optimal revascularization by conventional means. TMLR may avoid the disturbance of the hemodynamic deterioration and lower difficulty of the operation. Despite with encouraging clinical results, objective evidence for improved myocardial blood following TMLR remains controversial. Many studies showed that TMLR provided a long-term improvement in quality of life including Canadian Cardiovascular Society (CCS) angina class or New York Heart Association classification (NYHA) heart functional class for about 70% patients with severe angina pectoris.12The various shapes of myocardial laser channels would always be visible after TMLR by the color Doppler velocity technique. The survival rate of 5-years of TMLR as a sole treatment in Chinese patients was 64%.23Although it is impossible for some cases to realize the complete revascularization using TMLR combined with CABG, the results were also satisfied. We considered that complete revascularization, the long-term patency of the small bypass grafts depended on various factors. If it takes our 20-30 minutes or risk of haemodynamic instability to reconstruct each graft anastomosis, the negative effects of a prolonged operation outweigh benefit of multiple complete revascularizations of small vessels.
This study had several limitations: firstly, our study is the retrospective single-center methodology and not a randomized clinical trial; secondly, the small sample size used in this study remains as a limitation for further analysis.
In conclusion, the present study demonstrated that the safety and efficacy for both ONCAB and OPCAB techniques. Furthermore, the redo OPCAB or redo-CABG+TMLR technique tends to have a better prognosis in this selective patients. Our strategy is very effective in preventing haemodynamic instability and reducing morbidity in high-risk patients.
REFERENCES
1. Akins CW, Buckley MJ, Daggett WM, et al. Reoperative coronary grafting: Changing patient profiles, operative indications of techniques and results. Ann Thorac Surg 1994; 58:359-65.
2. He GW, Acuff TE, Ryan WH, et al. Determinants of operative mortality in reoperative coronary artery bypass grafting. J Thorac Cardiovasc Surg 1995; 110:971-8.
3. Yamamuro M, Lytle BW, Sapp SK, et al. Risk factors and outcomes after coronary reoperation in 739 elderly patients. Ann Thorac Surg 2000; 69:464-74.
4. Buffolo E, de Andrade CS, Branco JN, et al. Coronary artery bypass grafting without cardiopulmonary bypass. Ann Thorac Surg 1996; 61:63-6.
5. Edmunds LH Jr. Why cardiopulmonary bypass makes patients sick: Strategies to control the blood-synthetic surface interface. Adv Card Surg 1995; 6:131-67.
6. Subramanian VA, McCabe JC, Geller CM. Minimally invasive direct coronary artery bypass grafting: Two-year clinical experience. Ann Thorac Surg 1997; 64:1648-53.
7. Légaré JF, Buth KJ, Hirsch GM. Conversion to on pump from OPCAB is associated with increased mortality: Results from a randomized controlled trial. Eur J Cardiothorac Surg 2005; 27:296-301.
8. Miyahara K, Matsuura A, Takemura H, et al. On-pump beating-heart coronary artery bypass grafting after acute myocardial infarction has lower mortality and morbidity. J Thorac Cardiovasc Surg 2008, 135:521-6.
9. Calafiore AM, Di Mauro M, Contini M, et al. Myocardial revascularization with and without cardiopulmonary bypass in multivessel disease: Impact of the strategy on early outcome. Ann Thorac Surg 2001; 72:456-62.
10. Allen KB, Matheny RG, Robison RJ, et al. Minimally invasive versus conventional reoperative coronary artery bypass. Ann Thorac Surg 1997; 64:616-22
11. Trehan N, Mishra YK, Malhotra R, et al. Off-pump redo coronary artery bypass grafting. Ann Thorac Surg 2000; 70:1026-9.
12. Frazier OH, Tuzun E, Eichstadt H, et al. Transmyocardial laser revascularization as an adjunct to coronary artery bypass grafting a randomized, multicenter study with 4-year follow-up. Tex Heart Inst J 2004; 31:231-9.
13. Pratalia S, Chiaramontia F, Milanob A, et al. Transmyocardial laser revascularization 12 years later. Interact Cardiovasc Thorac Surg 2010; 11:480-1.
14. Rastan AJ, Bittner HB, Gummert JF, et al. On-pump beating heart versus off-pump coronary artery bypasssurgery-evidence of pump-induced myocardial injury. Eur J Cardiothorac Surg 2005; 27:1057-64.
15. Walpoth BH, Bosshard A, Kipfer B, et al. Failed coronary artery bypass anastomosis detected by intraoperative coronary flow measurement. Eur J Cardiothorac Surg 1998; 14 (Suppl 1):S76-81.
16. Mikkola R, Gunn J, Heikkinen J, et al. Use of blood products and risk of stroke after coronary artery bypass surgery. Blood Transfus 2012; 10:490-501.
17. Ostermann ME, Taube D, Morgan CJ, et al. Acute renal failure following cardiopulmonary bypass: A changing picture. Intensive Care Med 2000; 26:565-71.
18. Gaudino M, Luciani N, Giungi S, et al. Different profiles of patients who require dialysis after cardiac surgery. Ann Thorac Surg 2005; 79:825-9.
19. Gummert JF, Bucerius J, Walther T, et al. Requirement for renal replacement therapy in patients undergoing cardiac surgery. Thorac Cardiovasc Surg 2004; 52:70-6.
20. Bellomo R, Raman J, Ronco C. Intensive care unit management of the critically ill patient with fluid overload after open heart surgery. Cardiology 2001; 96:169-76.
21. Suzuki T, Okabe M, Handa M, et al. Usefulness of preoperative intraaortic balloon pump therapy during off-pump coronary artery bypass grafting in high-risk patients. Ann Thorac Surg 2004; 77:2056-9.
22. Vohra HA, Dimitri WR. Elective intraaortic balloon counterpulsation in high-risk off-pump coronary artery bypass grafting. J Card Surg 2006; 21:1-5.
23. Qu Z, Zheng JB, Zhang ZG. Single-center report of 5-year follow-up on 94 patients underwent transmyocardial laser revascularization. Chin Med J 2007; 120:1982-5.
for publication June 19, 2014.
Tel: 86-10-82266950, E-mail: drwusong@163.com
 Chinese Medical Sciences Journal2015年1期
Chinese Medical Sciences Journal2015年1期
- Chinese Medical Sciences Journal的其它文章
- Use of Cataract Surgery in Urban Beijing: a Post Screening Follow-up of the Elderly with Visual Impairment due to Age-related Cataract
- Lipopolysaccharide Challenge Induces Long Pentraxin 3 Expression in Mice Independently from Acute Lung Injury△
- Reliability of a Novel Cobb Protractor for Measuring the Cobb Angle of Radiograph in Scoliosis
- Role of Removing Stasis and Reducing Heat Formula in Clearance of Proximal Ureteral Calculi after Ureteroscopic Ho:YAG Laser Lithotripsy: A Prospective Randomized Study
- MRI Evaluation of Lateral Geniculate Body in Normal Aging Brain Using Quantitative Susceptibility Mapping.△
- Total Glycosides of Ranunculus Japonius Prevent Hypertrophy in Cardiomyocytes via Alleviating Chronic Ca2+Overload
