Effect of Feeding Management on Aspiration Pneumonia in Elderly Patients with Dysphagia☆
Min Li,Zheng Wang,Wei-Jia Han,Shi-Yin Lu,Ya-Zhen Fang
Geriatric ward,Huadong Hospital Affiliated to Fudan University,Shanghai 200040,China
Original article
Effect of Feeding Management on Aspiration Pneumonia in Elderly Patients with Dysphagia☆
Min Li,Zheng Wang*,Wei-Jia Han,Shi-Yin Lu,Ya-Zhen Fang
Geriatric ward,Huadong Hospital Affiliated to Fudan University,Shanghai 200040,China
A R T I C L E I N F O
Article history:
13 April 2015
Accepted 22 June 2015
Published 20 September 2015
Elderly
Dysphagia
Feeding management
Aspiration pneumonia
Objective:To investigate the effects of feeding safety instructions and dietary intervention on aspiration pneumonia in elderly patients with dysphagia.
Methods:The study included 40 long-term hospitalized elderly patients with dysphagia who needed oral intake.According to the voluntary and matching principle,participants were divided into the intervention group(n=20)and control group(n=20).We formed a multi-disciplinary team including clinical nurses,rehabilitation therapists and nutritionists.Clinical nurses collaborated with nutritionists and rehabilitation therapists to carry out feeding management.The patients in the control group were fed with semi-solid food,thick liquid,a partial mushy diet and so on according to their swallowing situations and tastes or preferences.The patients in the intervention group were fed with an all mushy diet.Patients in both groups were able to eat foods on their own or with assistance.
Results:After a three-month intervention,the incidence of aspiration pneumonia in both groups was decreased,and the difference was statistically significant(P<0.05).In the control group,seven patients had aspiration pneumonia,including two cases who died after nasogastric feeding due to aggravated dysphagia.In the control group,seven patients had aspiration pneumonia,including two cases was given nasogastric feeding due to aggravated dysphagia and then one case died.In the intervention group,four patients had aspiration pneumonia.There was no dropouts in either group.
Conclusions:Elderly patients with dysphagia require a multidisciplinary team to work closely with them to carry out feeding management.Nurses should conduct safety guidance for care catering and encouraging patients to actively eat a mushy diet.The diet can reduce the incidence of aspiration pneumonia,maintain oral intake and improve the quality of life.
©2015Shanxi Medical Periodical Press.Production and hosting by Elsevier B.V.This is an open access article under the CC BY-NC-ND license(http://creativecommons.org/licenses/by-nc-nd/4.0/).
1.Introduction
Dysphagia,also known as swallowing disorders,is due to the lower jaw,lips,tongue,soft palate,throat,esophagus or esophageal sphincter function impaired. People with dysphagia cannot put food from the mouth to the stomach safely and effectively to get adequate nutrition and water feeding is difficult.1
A questionnaire was given to 931 senior citizens who live in nursing home in the Shanghai area.The survey showed that the incidence of dysphagia for 80 to 89 years olds,90 to 99 year olds and 100 year old and older segment was 35.6%,43.7%,and 50.0%,respectively.2In addition,the incidence of dysphagia rises with increasing age.Aspiration is the most common complication.It can cause recurrent aspiration pneumonia and even asphyxia,which are life threatening.Japanese researchers3found that pneumonia was the third cause of death in elderly over 65 years of age and was the first cause in elderly over 85 years of age and older,of which more than 60 percent was caused by dysphagia.It is predicted that Chinese senior citizens over 80 years of age will reach 24 million in the“Twelfth Five-Year Plan”period.Although domestic dysphagia rehabilitation work has been carried out,professional speech therapists and physical therapists are still lacking.This study was carried out to evaluate feeding management through the formation of multi-disciplinary teams.We provided diet safety instructions and dietary intervention to elderly patients with dysphagia and observed the occurrence of aspiration pneumonia.
2.Material and Methods
2.1.Participants
We selected long-term hospitalized elderly patients in the geriatric ward in Huadong Hospital between March 2011 and September 2012 who needed oral intake of foods and drinks.The inclusion criteria were:(1)A known case of dysphagia diagnosed by specialists based on the Standardized Swallowing Assessment(SSA);4(2)mild-to-moderate dysphagia as assessed by Caiteng’s rating method(divided into seven levels;level 7 was normal,level 6 were mild,level 3-5 were moderate,level 1-2 were severe);and(3)stable disease.The exclusion criteria were:(1)Severe malnutrition;(2)acute phase of lung infections and gastrointestinal diseases. This study evaluated a total of 95 cases of elderly patients and found 68 cases(71.6%)had dysphagia.After patients signed informed consent,20 cases were assigned into the intervention group.Then,we chose another 20 cases from those who met the inclusion criteria to form a control group according to the matching principle.Patients in both groups had a similar age,gender,underlying diseases,dietary habits,degree of dysphagia and other basic characteristics.There was no significant difference between the intervention and control groups in clinical data(P>0.05,Table 1).

Table 1The clinical data of the two groups of patients[cases(%)].
2.2.Methods
2.2.1.Formation of a multi-disciplinary team5
Our team included two rehabilitation technicians,one administrative dietitian,ten primary care nurses and one resident physician.(1)Training for team members:Our team members were trained by rehabilitation technicians and administrative dietitians on a rating scale of SSA and related knowledge of dysphagia.(2)The mission of the team members is clear-cut and involves collaboration. After nurses confirmed patients with dysphagia,they informed rehabilitation technicians to perform a further evaluation based on Caiteng’s rating method.We held the first official case discussion and invited patients’fam-ily members to participate.In the discussion,rehabilitation technicians decided the appropriate swallowing function training for patients according to their swallowing function and explained the relevant considerations.The dietitian was responsible for nutrition management and guidance;they also determined the types,properties and quantity of food.The resident physician assessed the disease and then provided summaries and decided the clinical treatment guidelines.Nurses played a role in keeping the patient’s mouth clean and providing safe eating education.They also assisted patients to take food and gave patients’families eating guidance.Nurses assessed patients’feeding status and informed the resident physician and rehabilitation technicians when they found something abnormal.Then,the resident physician and rehabilitation technicians reassess the patients.Families provided mental support and observed the patients in a non-treatment period.
2.2.2.Screening
Cichero,et al.6considered that nurses are the professionals who contact patients most frequently,so they are fully capable of screening for dysphagia.In this study,two highly qualified nurses assessed the patients’dysphagia situation based on the Standards Swallowing Assessment Scale(SSA).The contents were assessed from easy to difficult according to three steps.First,the nurse checked the patient’s consciousness,postural control and structural functions of lips,tongue,pharynx,and so on. Second,patients were asked to perform the drink-water test,in which the volume of water was gradually increased from 5 mL to 60 mL.If any step of the test appeared abnormal,the test was immediately terminated and the patients were diagnosed with dysphagia.Ma et al.7thought that the SSA was reliable and valid for assessing swallowing function in elderly patients.It is suitable for bedside assessment,and its simple process significantly reduces the risk of a large number of aspirations during the examinations.
2.2.3.Diet safety instructions
Detailed management of oral intake can effectively reduce the incidence of aspiration and other complications in elderly patients with dysphagia and improve patient quality of life.8Helping and guiding elderly patients to eat safely is a nursing intervention that requires professional nursing knowledge and skills.Although it has not received enough attention in China,the UK Department of Health used it as a criterion to assess nurses’work.9Referring to“The Basis of Elderly Care and Technology”,which was compiled by Ma,10our team members all participated in the production of an education handbook titled“Diet Safety Instructions in Elderly Patients”. It was used to provide specific guidance to patients and primary caregivers in both groups.Nurses assessed the patients’general state and feeding status before eating and observed the six eating steps closely:(1)Maintain eating posture;(2)see food;(3)eat food with tableware;(4)place food into the mouth;(5)chew;and(6)swallow.The patients needed help if any one of the above could not be finished independently.11
2.2.3.1.Eating status
Elderly patients can only eat food when they are awake. First,they should make their mouth moist to quickly trigger the swallowing reflex when food enters their mouth. They also need to remain quiet to avoid distractions that will affect swallowing.Our team encouraged elderly patients to feed themselves to improve their eating ability and reduce psychological dependence.
2.2.3.2.Eating posture
Changing the patient’s head or body posture can relieve dysphagia symptoms and improve or relieve swallowing.12Patient posture should match their physical capabilities.Sitting posture is the best.Sitting up straight and putting the body slightly forward a 20°and slightly bending the neck bend forward will allow food to easily enter the esophagus.When patients eat food in the supine position,the correct position is lying on the healthy side,with their head elevated to 45°with the neck and head slightly bent forward.Eating on the healthy side can prevent leakage,and it is conducive to the food delivery from lips to the base of the tongue.Elderly patients should not conduct turning onto their back,oropharyngeal examination,sputum aspiration or other operations immediately after eating to prevent stomach reflux.Sitting for two hours after a meal can reduce the incidence of aspiration pneumonia by 10%.13
2.2.3.3.Tableware selection
Elderly patients should use special tableware.Chopsticks were encouraged to be used because fine motor skills can positively stimulate the brain.Shallow spoons with thick handles,3 cm×5 cm size,were chosen for use.Straws or bottles were used for liquid feeding because the sucking action can easily trigger the swallowing reflex.
2.2.3.4.Focus on the amount of each swallow
The most suitable amount of each swallow usually starts with a small amount(2-4 mL)and builds gradually according to the patients’situation.Swallowing too much each time will make food leak from the mouth or cause aspiration due to residual food in the throat.However,the swallowing reflex is difficult to induce if each swallow is too small.Supine patients’amount of each swallow is less than sitting patients’.Because of this,enough time is given to chew and avoid pressuring them.
2.2.3.5.Control feeding time
If each swallow time of a certain food is more than 10 seconds,this food is prohibited.The optimal time for one meal is less than 30 minutes;a meal time that is too long will lead to aspiration caused by fatigue of the swallowing function.14If each food intake is not enough,the frequency of meals is increased.
2.2.3.6.Observation of breathing
Normal swallowing requires a momentary pause in breathing(throat closed 0.3-0.5 s)to let food go through the pharynx;nasal breathing is used during chewing.It is easy to cause aspiration if patients have shortness of breath during a meal,chew with mouth breathing or swallow while breathing.15
2.2.3.7.Oral hygiene
Patients should use a soft toothbrush and water to moisten and clean the mouth effectively before and after meals.Their dentures should be removed for cleaning,and residue or sputum in the mouth and throat need to be completely eliminated.Oral hygiene is very important for patients with dysphagia.Yoneryama,et al.16observed that eliminating secretions in the mouth in a timely manner can significantly reduce the incidence of aspiration pneumonia caused by aspiration.Professional oral care has been proven to reduce oropharyngeal bacteria and the incidence of pneumonia in elderly patients.17,18
2.2.3.8.Feeding method
Before eating,patients were informed of the food’s raw materials,cooking methods and colors or shapes to promote patients’appetite when they see food.Patients should choose the appropriate size tableware,place it in the middle of the tongue rather than in the depths of mouth and try to make the tableware not contact their teeth.When they drink fluids,they place a straw into their mouth from their lips.The straw should be inserted into the bottom of the utensils to avoid swallowing air and causing bloating.Patients need to use two straws to prevent the mixing of each flavor when they drink two types of fluids.A variety of food should be changed by a small amount,and feeding different mixed food is prohibited.Not only it is difficult to form a bolus,but the liquid portion may also inflow into the throat and cause aspiration.If necessary,patients should perform“empty swallowing”and“interaction swallowing”.Only when there is no residual food in the mouth and palate,should they take a second bite of the meal.Patients whose food intake cannot reach the required amount should be given high protein food with a large amount of vitamins.
2.2.3.9.Treatment of choking and aspiration
When a cough occurs,we ask patients to bow,lean forward and lower their jaw to their chest.Bedridden patients have to turn their heads to one side immediately and lean forward.(1)If the cough occurs before swallowing,the food in the mouth should be cleared.The patients are asked to perform an“empty swallowing”action after they breathe smoothly to clear food debris in the throat.(2)If the cough occurs simultaneously with swallowing,patients often have violent coughs.Patients are encouraged to cough effectively when they can breathe without interruption.The patients are asked to perform an“empty swallowing”action if it is possible.(3)If patients have wheezing,dyspnea,or hoarseness or are pale and turn blue,an airway obstruction may have occurred.Nurses should use the suction device or work with a doctor to use a fiber bronchoscope to suck out the foreign matter and perform a tracheal intubation for mechanical ventilation;then,patients should be given high concentrations of oxygen and other treatments.(4)Nurses should also master the simple and effective emergency first aid measures;the first choice is the Heimlich maneuver.19They can hold the patients from behind,put their fists below the xiphoid,and extrude to the direction of the diaphragm to push out foreign matter by the strong airflow in the trachea.
2.2.4.Diet intervention
Wang,et al.1argued that the primary task of care givers working for patients with dysphagia is to find the correct patterns of nutrient intake.All patients’diets were formulated by one dietitian who participated in the study,and then,the hospital nutrition department prepared food,and the patients consumed the foods by themselves or with feeding assistance.
2.2.4.1.Eating patterns in the intervention group
As reported in the literature,20when patients with dysphagia take a food that has a viscosity lower or higher than that of honey compared to a food with a viscosity similar to that of honey,the incidence of aspiration was significantly increased.Nutritionists recommend a full mushy diet for patients to allow the family to look after patients discharged from hospital.Trained nurses put all of the food,including staple food,vegetables,meat,soup and other food,into a food masher until it has the viscosity consistent to that of honey.When patients take liquids,water and oral medicine that are ground to a powder,they make them mushy by adding 150 mL of water and 2 g of coagulant.We use Resource Thicken UpA 125 g/tank,which is produced by Nestlé and is specifically designed for patients with dysphagia.It is a whole plant powder that is refined from corn,does not change the nutrition or taste of food,and is low in sugar,sodium and heat.The full mushy diet ruins the morphology and color of food,which can affect patients’acceptance of the food.Because of this,we assigned the participants into the intervention group according to whether patients and their families fully understand the full mushy diet and accept it.
2.2.4.2.Eating patterns in the control group
We gave patients food according to their degree of dysphagia,diet prescription(according to the nutritionists’recommendation)and tastes and preferences.Elderly patients should eat soft food,semi-liquid food,a mushy diet and shredded or boiled large chunks and longfiber foods to compensate for the decline of the chewing function caused by caries and missing teeth.
2.2.5.Observation items
We performed a retrospective review of the medical records,collected two groups of patients’incidence of aspiration pneumonia three months before the intervention and recorded the incidence of aspiration pneumonia within three months of intervention.Diagnostic criteria for aspiration pneumonia.13(1)There are underlying diseases,such as cerebrovascular disease,consciousness disorders caused by various reasons,and so on.(2)Clinical manifestations:Patients with dysphagia may have many manifestations such as the following:Food is stuck in the mouth and chewed for too long time;coughing and choking may occur before,during and after swallowing;residual food in the mouth with another swallowing dysfunction;and positive symptoms or signs of lung inflammation.(3)Iconography reminds lung inflammation.(4)Positive sputum culture.
2.2.6.Statistical methods
We used the statistical software SPSS 20.0 to process the data.The measurement data were represented by, and an independent sample t test was used for the intergroup comparison.The count data were expressed by ratios,and the chi-square test was used for comparison between groups(Table 2).
3.Results
Table 2 shows that there was no significant difference between the two groups(P>0.05)three months before intervention.The difference between the two groups was statistically significant(P<0.05)after the three month intervention.
There were 20 patients respectively in the intervention group and control group.The study showed that therewas no significant difference between the two groups(P>0.05)three months before intervention.The incidence of aspiration pneumonia in both groups decreased three months after intervention.The self-matching test difference was statistically significant(P<0.05).There were seven patients with aspiration pneumonia in the control group during the three month intervention,including two cases of dysphagia that were aggravated on the 45th day and 76th day.Their dysphagia degree decreased from level 3 to level 2,being given a nasogastric intubation and one case died on the 85th day.In addition,three cases of aspiration pneumonia emerged on 31st day,56th day and 68th day,caused by aspiration.Then,patients agreed to have a full mushy diet.In the mushy diet group,there were four cases with aspiration pneumonia and no dropouts.Statistical comparison between the two groups after interventions was not performed due to the limitations of the study and the smaller sample number.
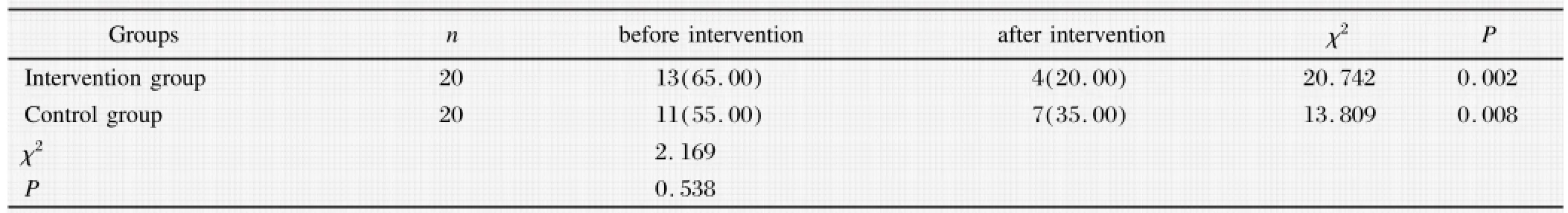
Table 2Comparison of the two groups of patients with aspiration pneumonia[cases(%)].
4.Discussion
4.1.Carrying out feeding management with a group work model and nurses’active participation can reduce the incidence of aspiration pneumonia in elderly patients with dysphagia.
Ferguson et al.21observed that there were many elderly people with dysphagia,but that they seldom reported to health care professionals.Many elderly people had chronic dysphagia despite appearing normal.Chinese dysphagia rehabilitation assessment and treatment expert consensus(2013 edition)5considers the evaluation and treatment of dysphagia and requires close collaboration of a team composed of various professionals. However,we need to develop an efficient collaborative model according to the domestic configuration.Nurses trained by a professional team can find patients with dysphagia early and observe them at any time.All the details of patients’feeding should be taken into account to provide professional eating safety guidance.This study showed that there was no significant difference between the two groups(P>0.05)three months before intervention.In addition,the incidence of aspiration pneumonia in both groups decreased after three months of intervention.The self-matching test difference was statistically significant(P<0.05).It showed that early detection of dysphagia and focusing on eating safety in elderly patients with dysphagia can reduce the occurrence of aspiration pneumonia.Symptoms of aspiration pneumonia in elderly patients are often atypical.They may have no irritating cough,shortness of breath or other symptoms at that time.They may show listlessness,unconsciousness,cough,sputum and fever.The proportion of patients whose leucocytes increased was lower(relative to young adults).This disease is known as occult aspiration.22It was reported that the incidence of occult aspiration is even higher than dominant aspiration by up to 40%-70%.23Ramsey,et al.24believed that the only clue to diagnosing occult aspiration is the sudden decline of oxygen saturation or a fever.Because of this,the clinical observation of nurses becomes more important.
4.2.Dietary intervention can reduce aspiration pneumonia due to choking or cough in elderly patients with dysphagia
Elderly patients’chewing ability decreased due to tooth damage and loss,salivary secretion reduction,as well as a decline in exercise capacity caused by a variety of diseases.Because of this,many patients experienced persistent or intermittent dysphagia therefore they could not swallow solids or liquids.Food that is easy to swallow is characterized by having a uniform density and appropriate viscosity,is not easy to become loose or easily deformed through the pharynx and esophagus and do notleave residual on the mucous membrane.This study had seven patients with aspiration pneumonia in the control group during the three month intervention,including two cases of dysphagia that were aggravated on the 45th day and 76th day.Their dysphagia degree decreased from level 3 to level 2,and one case died on the 85th day after being given a nasogastric intubation.In addition,three cases of aspiration pneumonia emerged on 31st day,56th day and 68th day,caused by aspiration;the patients agreed to have a full mushy diet.There were four cases with aspiration pneumonia in the mushy diet group and no dropouts.Statistical comparison between the two groups after the interventions was not performed due to the limitations of the study,and the size of sample was smaller than normal.However,we still believe that dietary intervention can reduce the risk of aspiration in elderly patients with dysphagia.Because the nonmushy food does not easily form a bolus and slide into the throat and dispersed food particles can easily enter the trachea or larynx with breathing,choking and aspiration can occur.However,there are many patients who think that mixing a variety of food together to make a mushy diet will affect the senses and reduce the taste of food.We recommended that patients break different foods apart and put them in different places to increase the pleasure of eating.
4.3.The importance of maintaining oral intake in elderly patients
Patients with severe dysphagia(level 1-2)must be given gastrointestinal and parenteral nutrition,while mild dysphagia patients(level 6)should take food by mouth.Patients with moderate dysphagia(level 3-5)have a risk of aspiration;the most common treatment for them is limiting oral intake,nasogastric feeding,percutaneous endoscopic gastrostomy(PEG),and so on. These treatments can easily lead to psychological symptoms,such as depression,social isolation and others. Tube feeding is seemingly effective,low in cost,and easy for nurses to manage.Because of this,it is convenient for health care workers and family members,and leads to the widespread use of tube feeding therapy. However,nasogastric feeding is uncomfortable,cannot prevent oral secretions aggregation,and may hinder cardiac function and leads to regurgitation and aspiration easily.25Compared with nasogastric feeding,PEG’s risk of death and poor prognosis after six months increased significantly.26In recent years,with the increase of the aging population,people have a new awareness that oral intake is important for a person to survive.Dysphagia in elderly patients due to disease and physiological degradation is usually persistent and develops progressively.Inappropriate restriction of oral intake will not only increase the psychological pressure on elderly patients but also cause apraxia of the pharynx and palate and tongue atrophy.In addition,it degenerates patients’swallowing function,27leading to a lifetime use of a feeding tube. Therefore,even if the patient is unable to have entire meals via oral intake,patients should make sure that part of their oral intake should undergo dietary adjustments. It is also important for elderly patients to perform a certain degree of swallowing activities every day to improve or maintain the swallowing function.
5.Conclusions
Elderly patients with dysphagia require a multidisciplinary team working closely together to carry out feeding management.Nurses have more opportunities to contact patients in clinical work,so they must learn the correct guidance of safe eating and feeding for elderly patients with dysphagia.Then,they can improve patients’and their families’awareness of aspiration and encourage them to eat a mushy diet.These treatments can effectively reduce the incidence of aspiration pneumonia and delay feeding tube treatment.The treatments can also help meet elderly patients’requirements for oral intake to maintain a normal physiological function and improve their quality of life.
Conflicts of interest
All contributing authors declare no conflicts of interest.
References
1.Wang RM,Zhang L,Zhang CJ.How to carry out rehabilitation of feeding and dysphagia in general hospitals.Chin J Phys Med Rehabil.2013;35:988-992[in Chinese].
2.Han WJ,Sun JQ,Yi Q,et al.A research on the dysphagia and nutrition risk of senior citizens who live in conservation agencies in the Shanghai area.Geriatr Health Care.2012;18: 170-172[in Chinese].
3.Jin SC,Zhang D,Dou ZL.Clinical studies and new challen-ges of swallowing dysfunction.Chin J Phys Med Rehabil. 2011;33:883-884[in Chinese].
4.Ellul J,Barer D.On behalf of ESDB/COSTAR collaborative dysphagia study.Interobserver reliability of a Standardized Swallowing Assessment(SSA).Cerebrovasc Dis.1996;6: 152-153.
5.Chinese dysphagia rehabilitation assessment and treatment expert consensus group.Chinese dysphagia rehabilitation assessment and treatment expert consensus(2013 Edition).Chin J Phys Med Rehabil.2013;35:916-929[in Chinese].
6.Cichero JA,Heaton S,Bassett L.Triaging dysphagia:nurse screening for dysphagia in an acute hospital.Clin Nurs.2009;18:1649-1659.
7.Ma YL,Zhang LM,Zhu QY,et al.Reliability and validity of using standard rating scales to assess swallowing function in elderly patients with swallowing.J Nurs.2012;19:65-67[in Chinese].
8.Lin T,Cai CY.Effect of feeding details management on nutritional status and complications of Alzheimer’s patients.Chin Nurs Res.2009;23:3042-3043[in Chinese].
9.Zygo J.Feeding the patient who cannot take care of themselves.Foreign Med Sci Nurs.2003;22:499[in Chinese].
10.Ma YN.Basic nursing and technology in the elderly(Continued 3).Foreign Med Sci Nurs.2004;23:53-59[in Chinese].
11.Fu ZY,Wu F.Rehabilitation training for dysphagia in poststroke pharyngeal phase.Chin Gen Prac Nurs.2009;7:755-756[in Chinese].
12.Park BH,Seo JH,Ko MH,et al.Effect of 45°reclining sitting posture on swallowing in patients with dysphagia.Yonsei Med J.2013;54:1137-1142.
13.Zheng H,Chen JN,Yu X,et al.The clinical features and etiological analysis of the elderly patients with aspiration pneumonia.Chin J Nosocomiol.2008;18:372-375[in Chinese].
14.Huo JS,Dou ZL,Zhang D,et al.The safety feeding techniques of the stroke patients in dysphagia recovery period. Chin Nurs Res.2012;26:141-142[in Chinese].
15.Gross RD,Steinhauer KM,Zajac DJ,et al.Direct measurement of subglottic air pressure while swallowing.Laryngoscope.2006;11:753-761.
16.Yoneryama T,Yoshida M,Ohmi T,et al.Oral care reduces pneumonia in order patients in nursing homes.J Am Geriatr Soc.2002;50:430-433.
17.Ishikawa A,Yoneyama T,Hirota K,et al.Professional oral health care reduces the number of oropharyngeal bacteria.J Dent Res.2008;87:594-598.
18.Adachi M,Ishihara K,Abe S,et al.Professional oral health care by dental hygienists reduced respiratory infections in elderly persons requiring nursing care.Int J Dent Hyg.2007;5: 69-74.
19.Du GQ,The first aid and nursing for choking and suffocation in frail elderly patients.Chin J Geriatr Care.2010;08:83[in Chinese].
20.Kuhlemeier KV,Palmer JB,Rosenberg D.Effect of liquid bolus consistency and delivery method on aspiration and pharyngeal retention in dysphgia patients.Dysphagia.2001;16: 119-122.
21.Ferguson R,Greener M.Dysphagia pilot study.Pharmacy. 2005;3:44.
22.Hu YH.Aspiration pneumonia in elderly patients:clinical analysis of 36 cases.J Clin Pulm Med.2013;18(5):876-877[in Chinese].
23.Du J,Zheng SB.Advances in the diagnosis of aspiration. Chin J Mult Organ Dis Elderly.2011;10:563-565[in Chinese].
24.Ramsey DJ,Smithard DG,Kalra L.Early assessments of dysphagia and aspiration risk in acute stroke patients.Stroke. 2003;34:1252-1257.
25.Marik PE.Aspiration pneumonitis and aspiration pneumonia. N Engl J Med.2001;344:665-671.
26.Dennis MS,Lewis SC,Warlow C.FOOD Trial Collaboration.Effect of timing and method of enteral tube feeding for dysphagic stroke patients(FOOD):a multicentre randomized controlled trial.Lancet.2005;365:764-772.
27.Song ZH,Zhe M,Ma SP,et al.The efficacy of comprehensive rehabilitation therapy for stroke combined pseudobulbar palsy patients’dysphagia.Chin J Phys Med Rehabil.2006;28:255-256[in Chinese].
30 December 2014
in revised form
☆This work was supported by the nursing scientific research foundation of Fudan University(No.FNF201019).
.
E-mail address:liu_xu0028@sina.com(Z.Wang).
Peer review under responsibility of Shanxi Medical Periodical Press.
http://dx.doi.org/10.1016/j.cnre.2015.09.004
2095-7718/©2015 Shanxi Medical Periodical Press.Production and hosting by Elsevier B.V.This is an open access article under the CC BY-NC-ND license(http://creativecommons.org/licenses/by-nc-nd/4.0/).
- Frontiers of Nursing的其它文章
- The Outcomes and Influencing Factors of Telecare Managing Patients with Type 2 Diabetes
- Progress in Traditional Chinese and Western Medicine Treatments and Nursing Care of Knee Osteoarthritis☆
- Subglottic Secretion Drainage for Preventing Ventilator Associated Pneumonia:A Meta-analysis
- Study on the Relationships between Nurses'Job Burnout and Subjective Well-being
- Practice and Evaluation:Management of Acupuncture Needle Disinfection and Sterilization
- Active Learning Improves Nursing Student Clinical Performance in an Academic Institution in Macao☆