Treatment of Primary Dysmenorrhea with Herbpartitioned Moxibustion plus Ultra-short Wave
1 Department of Acupuncture and Moxibustion, Taihe Hospital, Hubei University of Medicine,Shiyan 442000, China
2 People’s Hospital, Hubei University of Medicine, Shiyan 442000, China
CLINICAL STUDY
Treatment of Primary Dysmenorrhea with Herbpartitioned Moxibustion plus Ultra-short Wave
Liu Min-juan1, Wang Kui2
1 Department of Acupuncture and Moxibustion, Taihe Hospital, Hubei University of Medicine,Shiyan 442000, China
2 People’s Hospital, Hubei University of Medicine, Shiyan 442000, China
Author: Liu Min-juan, technician-in-charge
Objective: To observe the clinical effect of herb-partitioned moxibustion plus ultra-short wave for primary dysmenorrhea (PD).
Methods: One hundred and thirty patients with PD were randomly divided into a treatment group and a control group, 65 cases in each group. Patients in the treatment group were treated with herb-partitioned moxibustion plus ultra-short wave, while patients in the control group were treated with oral administration of Ibuprofen sustained-release capsules. After completing three courses of treatments, the clinical effects were evaluated by professional researchers.
Results: The recovery rate of the treatment group was 58.5%, and the total effective rater was 98.5%; versus 24.6% and 81.5% in the control group. The between-group differences were statistically significant (P<0.05).
Conclusion: Herb-partitioned moxibustion plus ultra-short wave is an easy-to-operate and effective therapy for PD.
Moxibustion Therapy; Indirect Moxibustion; Physical Therapy Modalities; Dysmenorrhea
Primary dysmenorrhea (PD) is one kind of dysmenorrhea without organic lesion of the reproductive system, and it is also known as functional dysmenorrhea, which is a common disease affecting adolescent girls or young women who have not given birth[1-2]. The clinical manifestation is mainly characterized by periodic pain in the lower abdomen or lower back during or around menstruation, and sometimes the pain is even unbearable. Some surveys showed that the prevalence of dysmenorrhea was 30% to 40%, and would be up to 50% in adolescent females, and patients with severe symptoms were accounted for 10%-20%[3]. Currently, Western medicine treatments for PD mainly include non-narcotic analgesics, prostaglandin synthetase inhibitors (non-steroidal anti-inflammatory drugs), oral contraceptives for suppressing ovulation, but the effects are not very satisfied because of the short effect and the obvious adverse reactions. We have used herb-partitioned moxibustion plus ultra-short wave therapy for PD since October 2009, compared with Western medicine treatment, and the results are summarized as follows.
1 Clinical Materials
1.1 Diagnostic criteria
The diagnostic criteria referred to the PD diagnostic criteria in theObstetrics and Gynecology[4]andCriteria of Diagnosis and TherapeuticEffects of Disease and Syndrome in Traditional Chinese Medicine[5]: Lower abdominal pain (within 1 week) during or around menstruation; the symptoms occur according with the menstrual cycle, and appear more than three times; normal in the pelvic by ultrasound or gynecological examination (unmarried women can have rectal examination); without the reproductive system organic lesions.
1.2 Inclusion criteria
Those who meet the diagnostic criteria abovementioned; between 14 and 30 years old.
1.3 Exclusion criteria
Those who have gynecological organic diseases (uterine fibroids, etc.); those who fear moxibustion therapy; those who cannot complete the treatment according to the protocol or receive other treatment during the study inducing affecting the efficacy observation.
1.4 Symptom scoring criteria
The symptoms were scored before and after treatment referring to the symptom scoring criteria inGuiding Principles for Clinical Study of New Chinese Medicines[6](Table 1).

Table1. The symptom scoring criteria for PD
1.5 General data
A total of 130 cases with PD were the outpatients in the Department of Acupuncture and Moxibustion, Taihe Hospital, Hubei University of Medicine, and they were enrolled from March 2012 to March 2013. The patients were enrolled according to visiting sequences and randomly divided into a treatment group and a control group according to the random number table. There were 65 patients in the treatment group, aged from 15 to 30 years old, with an average of 20.4 years; their duration ranged from 0.7 to 5.1 years. There were 65 cases in the control group, aged from 14 to 29 years old, with an average of 19.8 years; their duration ranged from 0.8 to 4.9 years. Patients in both groups had no history of induced abortion or drug abortion. There were no significant differences between the two groups in the general materials such as gender, age, duration, dysmenorrhea degree (P>0.05), thus the two groups were comparable.
2 Therapeutic Methods
2.1 Treatment group
2.1.1 Acupuncture-moxibustion
Herb cake composition:San Qi(Radix Notoginseng) 50 g,Yan Hu Suo(Rhizoma Corydalis) 30 g,Bai Jie Zi(Semen Sinapis Albae) 30 g,Ding Xiang(Flos Syzygii Aromatici) 30 g,Rou Gui(Cortex Cinnamomi) 30 g,Ru Xiang(Olibanum) 20 g,Mo Yao(Myrrha) 20 g,Chuan Shan Jia(Squama Manitis) 20 g,Fang Feng(Radix Sapshnikoviae) 20 g,Du Huo(Radix Angelicae Pubescentis) 20 g,Hua Jiao(Fructus Zanthoxyli) 15 g,Xi Xin(Herba Asari) 15 g,Gan Sui(Radix Kansui) 15 g.
Major points: Guanyuan (CV 4), Zhongji (CV 3) and blilateral Sanyinjiao (SP 6).
Adjunct points: Taichong (LR 3) and Xuehai (SP 10) were adder for qi stagnation and blood stasis; Xingjian (LR 2) and Yinlingquan (SP 9) for liver-qi stagnation and damp-heat; Shenshu (BL 23) and Mingmen (GV 4) for deficiency of liver and kidney; Qihai (CV 6) and Zusanli (ST 36) for qi and blood deficiency.
Operation: Firstly dry the herbs and grind them into extremely fine powder, then mix them with honey and ginger juice (1:1 ratio) in order to form a paste, which is a round cake of 2-3 cm in diameter and 0.5-1 cm thick, with several small holes in the middle punctured by a small sized three-edged needle. Ask the patient to take a supine position and fully expose the abdomen. Place the prepared herb cakes on the major points above-mentioned, and then put a moxa cone on an herb cake, finally light the moxa cone for moxibustion. The herb cake can be moved away slightly when the patient feels too hot, and if the moxa cone is burned up, wipe away the ashes and replace a new one. Drop a few drops of ginger juice if the herb cake is dried out. Light 3 moxa cones for one point, and skin redness would be acceptable except blistering. During moxibustion, the adjunct points above-mentioned were punctured. The disposable acupuncture needles of 0.30 mm in diameter and 40 mm in length were chosen for operation. After routine disinfection of the point areas, insert the needle into the skin quickly, with a depth of 1.5-2 cun according to the patient’s body shape, and then impose appropriate lifting and thrusting, twisting and rotating manipulations to enhance acupuncture sensation. After completing herb-partitioned moxibustion, remove the needles. Acupuncture treatment was conducted once a day, and 7 d for one course.
2.1.2 Ultra-short wave therapy
LDT.CD31 type ultra-short wave therapy apparatus produced by Shanghai Medical Instruments High Technology Corporation was used in the study, with 50 Hz in frequency, 7.2 m in wavelength and 80-100 mA in current intensity. Ask the patient lie in the prone position, and put two electrodes in the middle of the waist and the abdomen. Press and fix the abdomen with sandbags; make the output wires in parallel, let the patient expose to the ultra-short wave for 25 min, once a day.
2.2 Control group
The patients in the control group orally took 300 mg of Ibuprofen sustained-release capsule 1-2 d before menstruation or when there was abdominal pain (produced by Tianjin Smith Kline & French Laboratories Limited), twice a day, and insisted on the treatment for 2-3 d until symptom relieved. Patients with stomach discomfort took supplemented Vitamin B6.
Ask patients to avoid cold, raw or spice food, to eat more fresh fruits and vegetables and to avoid catching cold. Therapeutic effects of the both groups were statistically analyzed after three treatment courses.
3 Therapeutic Results
3.1 Therapeutic efficacy criteria[6]
Recovery: The symptom score turns to zero, and abdominal coldness and pain, pale face and other symptoms disappear, and there is no recurrence after 3 menstrual cycles.
Remarkable effect: The symptom score after treatment is less than 1/2 of that before treatment, and abdominal pain relieves obviously, and there is no dizziness, palpitations and other discomforts, not affecting daily life.
Effect: The symptom score after treatment is more than 1/2 but less than 3/4 of that before treatment, there is slight abdominal pain and other symptoms relieve.
Failure: There is no obvious relief of abdominal pain and other symptoms.
3.2 Statistical management
The SPSS 19.0 version statistical software was used for all the data analysis, and measurement data were expressed as mean ± standard deviationIntra-group comparison of measurement data were processed byt-test, while inter-group was compared by analysis of variance. AndP<0.05 indicates a statistically significant difference.
3.3 Results
The recovery rate of treatment group was 58.5%, and the total effective rate was 98.5%; the recovery rate of control group was 24.6%, and the total effective rate was 81.5%. The differences between the two groups were statistically significant(P<0.05), indicating that both treatments of herb-partitioned moxibustion plus ultra-short wave therapy and Ibuprofen were effective, but the former one was higher in recovery rate and total effective rate (Table 2).
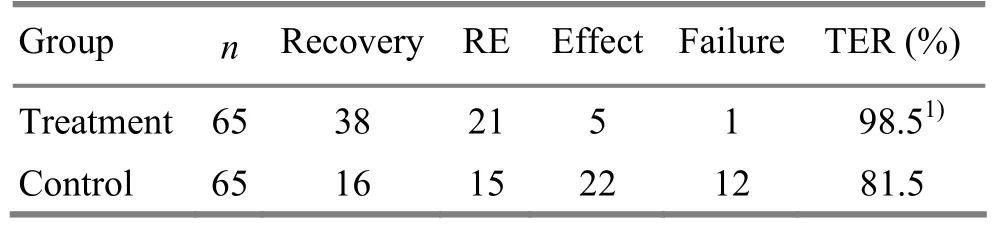
Table 2. Comparison of therapeutic effect between the two groups (case)
4 Discussion
In traditional Chinese medicine, PD belongs to the category of ‘abdominal pain during menstruation’. It often occurs as a result of inhibited flow of qi and blood. Based on syndrome differentiation of traditional Chinese medicine, PD can be divided into two categories: excess syndrome and deficiency syndrome. The former is usually caused by emotional discomfort, liver qi stagnation, or cold congealing in the uterus due to blocked qi and blood movement caused by cold drink or other cold pathogen during menstruation, and this is so-called meridian blockage leading to pain. And the latter is usually due to qi and blood deficiency, liver and kidney deficiency, malnourishment of the uterus and meridian, which is so-called deficiency leading to pain[7]. The disease is characterized by abdominal pain during menstruation, the onset according with the menstrual cycle. Female menstrual cycle reflects women’s physiological process of growth and decline of yin and yang as well as changes in rhythm of qi and blood, therefore, if conforming to the uterus filling or deficiency, regulating and treating the patient timely can achieve significant effect. PD is related to blood retention in uterus and impeded circulation of menstruation induced by spasmodic contraction, and the disease may be alleviated or cured after a normal delivery[8]. It’s thought in modern medicine that the onset of PD mainly has a relationship with endometrial synthesis during menstruation and the increase of prostaglandin release[9].
Moxibustion has effects of warming meridian and expelling cold, activating yang qi, as well as tonifying qi and preventing exhaustion. Mugwort floss smells fragrant and is pungent, hot, mobile and penetrating. Some experiments have proven that the heat and light generated by it can be effective to increase vascular permeability of the lesion, improve some indicators of haemorheology and hemodynamics such as blood thickening concentration, blood viscosity, blood aggregation, and reduce interleukin-1 (IL-1) and tumor necrosis factor (TNF) levels in the site of inflammation to decrease inflammation stimulation and promote local blood circulation, as a result to accelerate the clear of local pathological metabolites, and achieve the purpose of smooth flow of qi and blood which can kill pain.
Guanyuan (CV 4) is the crossing point of the Three Yin Meridians of Foot and the Conception Vessel, and can greatly tonify the Yuan-Primary qi. Acupuncturing Guanyuan (CV 4) can promote qi to activate blood and expel blood stasis to kill pain; moxibustion on Guanyuan (CV 4) can warm meridian to expel cold as well as regulate and tonify the Thoroughfare Vessel and the Conception Vessel. Herb-partitioned moxibustion has both effects of moxibustion and herbs, and it can increase the herb effect by the fire to make the effects of moxibustion and herb reach the lesion site, improve blood circulation, and strengthen the killing pain effect of moxibustion in order to regulate the body’s metabolism imbalance and immunity function. Meanwhile, the fire of herb-partitioned moxibustion is mild, and the heat can directly reach deep tissues through skin, thus can be accepted by the patients and can be applied for chronic diseases[10-11].
Secondly, mugwort floss can relieve the stiffness and pain in the spine by its effects of tonifying liver and kidney, warming yang and tonifying spleen as well as warming meridians to expel cold.San Qi(Radix Notoginseng) andYan Hu Suo(Rhizoma Corydalis) in the herb cake can stimulate qi and blood movement and relieve swelling and kill pain;Ding Xiang(Flos Syzygii Aromatici),Rou Gui(Cortex Cinnamomi),Hua Jiao(Fructus Zanthoxyli) andXi Xin(Herba Asari) can warm meridian, expel cold and kill pain;Fang Feng(Radix Sapshnikoviae) andDu Huo(Radix Angelicae Pubescentis) can expel wind and cold and remove dampness;Ru Xiang(Olibanum),Mo Yao(Myrrha) andChuan Shan Jia(Squama Manitis) can stimulate blood circulation and dredge meridian, and remove blood stasis to kill pain. Various herbs combination can not only expel wind and cold and remove dampness and kill pain, but also tonify qi and blood and strengthen muscles and bones. Many studies have showed that herb-partitioned moxibustion has been widely used in treating a variety of pain and achieved good effect, this therapy can warm and dredge the meridians, invigorate qi and consolidate the exterior, and can increase the clinical effect as well as enhance the body's immune system. A study has also indicated that Guanyuan (CV 4) has regulation function for endocrine system[11].
Guanyuan (CV 4), Qihai (6) and Zhongji (CV 3) are located in the lower abdomen and have effects of warming lower jiao, replenishing vital essence and blood as well as regulating and tonifying the Thoroughfare Vessel and the Conception Vessel. Sanyinjiao (SP 6) is the crossing point of Three Yin Meridians of Foot, and is also an important point for regulating the Liver, Spleen and Kidney Meridians. Ding YM, et al[12]treated 52 cases with PD by warm needling therapy at Sanyinjiao (SP 6) and the total effective rate was 98.1%. Moxibustion on Sanyinjiao (SP 6) can tonify qi, nourish blood and kill pain. In our study, Sanyinjiao (SP 6) was also selected, because we aimed at dredging meridian and killing pain through warming and tonifying qi of the Three Yin Meridians of Foot to warm uterus vessels, regulate the Thoroughfare Vessel and the Conception Vessel, and regulate qi movement and stimulate blood circulation.Sanyinjiao (SP 6) combined with Guanyuan (CV4), Qihai (CV 6) and Zhongji (CV 3) can warm the uterus and expel cold, regulate and tonify the liver and kidney, dredge meridian and expel stasis as well as regulate qi movement and kill pain, in order to harmonize the Thoroughfare Vessel and the Conception Vessel, make smooth flow of qi and blood, and regulate menstruation, thus dysmenorrhea can be cured[13].
Ultra-short wave therapy makes use of electromagnetic wave of specific wavelength and frequency for treatment. Ultra-short wave can have effects of making the small blood vessels especially deep capillary persistently dilate, increasing vascular wall permeability and blood flow velocity, which can benefit the edema dissipation and excretion and elimination of metabolic waste products, inflammation products, substances causing pain and bacterial and toxins. Ultra-short wave can inhibit sensory nerve conduction, and thus achieve analgesic effect.
PD mainly affects adolescent females. According to foreign reports, dysmenorrhea’s incidence is the highest among menstrual problems that adolescent girls are suffering from, and it can have impact on their daily life and work in varying degrees[14-15]. Ibuprofen is an effective prostaglandin (PG) synthesis inhibitor, which has strong anti-inflammatory, antirheumatic and fever and pain relief effects. And it can play an antispasmodic and analgesic role in menstruation use. However, the rate of recurrence is high after treatment stops. It can only relieve pain temporarily, and around 20% of patients may have adverse reactions such as headache, dizziness, nausea in different degrees. This study has showed that herb-partitioned plus ultra-short wave therapy for this disease is simple to operate, has significant effect, no adverse reaction, thus is worthy of clinical application.
Conflict of Interest
There is no conflict of interest in this article.
Acknowledgments
This work was supported by Taihe Hospital, Hubei University of Medicine.
Statement of Informed Consent
All the patients knew and volunteered to participate in this clinical study.
[1] Jamieson DJ, Steege JF. The prevalence of dysmenorrheal, dyspareunia, pelvic pain, and irritable bowel syndrome in primary care practices. Obstet Gynecol, 1996, 87(1): 55-58.
[2] Davis AR, Westhoff CL. Primary dysmenorrhea in adolescent girls and treatment with oral contraceptives. J Pediatr Adolesc Gynecol, 2001, 14(1): 3-8.
[3] Yang JL, Ou YY, Wang JY. Genecology Diseases: Clinical Diagnosis and Treatment of Traditional Chinese Medicine. Beijing: People’s Medical Publishing House, 2001, 14(1): 3-8.
[4] Le J. Gynecology and Obstetrics. 6th Edition. Beijing: People’s Medical Publishing House, 1980: 347.
[5] State Administration of Traditional Chinese Medicine. Criteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine. Nanjing: Nanjing University Press, 1994: 61-62.
[6] Ministry of Health of the People’s Republic of China. Guiding Principles for Clinical Study of New Chinese Medicines. Beijing: People's Medical Publishing House, 1993: 263-265.
[7] Lu Y. Clinical observation of treating dysmenorrheal with combining Taohong Siwu decoction and warm acupuncture. Liaoning Zhongyiyao Daxue Xuebao, 2013, 15(1): 169-170.
[8] Wu RD, Zhang HD, Lin LF. Observation on ear point taping and pressing therapy for treatment of primary dysmenorrhea. Zhongguo Zhenjiu, 2007, 27(11): 815-817.
[9] Fang ZR, Li YH. An observation of moxibustion’s effects and benefits for killing pain. Zhenci Yanjiu, 1993, 18(4): 296-299.
[10] Jiang ZY, Li CD. Clinical observation on treatment of cervical spondylosis with poking Dazhui Bazhen points. Zhongguo Zhenjiu, 2001, 21(2): 94-96.
[11] Wang HL, Hu L, Gao XZ. Effects of electroacupuncture of“Guanyuan” and “Sanyinjiao” on neuroendocrine function in perimenopausal model rats. Zhenci Yanjiu, 2003, 28(2): 124-127.
[12] Ding YM, Ma XY. Warm needling at Sanyinjiao (SP 6) for treating primary dysmenorrhea. Zhongguo Zhenjiu, 2009, 29(11): 883.
[13] An Y, Du DQ, Gao SZ, Ma YX. Clinical study on different intervention times of acupuncture for primary dysmenorrheal. Shanghai Zhenjiu Zazhi, 2013, 32(2): 91-93.
[14] Dangal G. Menstrual disorders in adolescents. BJOG, 2005, 4(1): 79.
[15] Sharma P, Malhotra C, Taneja DK, Saha R. Problems related to menstruation amongst adolescent girls. Indian J Pediatr, 2008, 75(2): 125-129.
Translator:Deng Ying
Wang Kui, technician-in-charge.
E-mail: zhengsu0413@126.com
R245.8
: A
Date:December 28, 2013
 Journal of Acupuncture and Tuina Science2014年2期
Journal of Acupuncture and Tuina Science2014年2期
- Journal of Acupuncture and Tuina Science的其它文章
- Effect of Combined Acupuncture and Shen Zao An Shen Tang on Sleep Quality of Insomnia Patients Due to Deficiency of the Heart and Spleen
- Effect of Moxibustion on the Motility, Absorption and Activities of ATPase in Small Intestine of Spleen-deficiency Rats
- Analysis of the Frequency of Clinical Acupoint Use Based on ‘Traditional Chinese Medical Acupuncture-moxibustion Information Databank’
- Systematic Review of Acupuncture for Functional Constipation
- Therapeutic Efficacy Observation on Combined Aerobic Exercise with Auricular Point Sticking for Insomnia in College Students
- Effect of Foot Bath and Massage on Insomnia in Patients with Liver Cirrhosis and Investigation of Nursing Satisfaction
